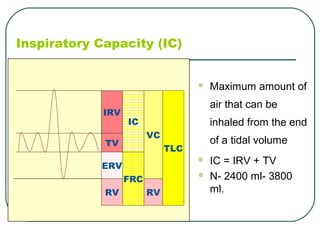
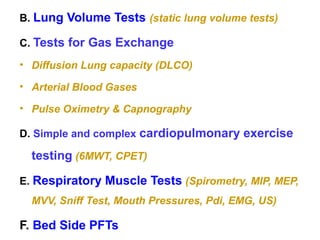
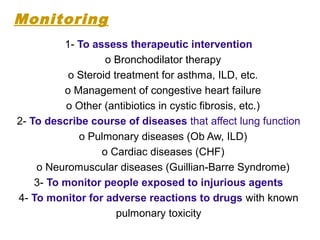
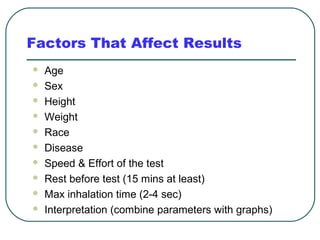
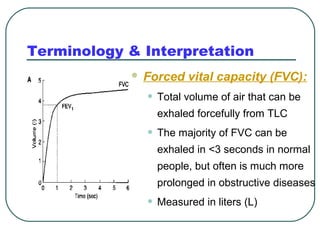
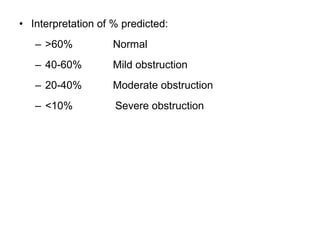
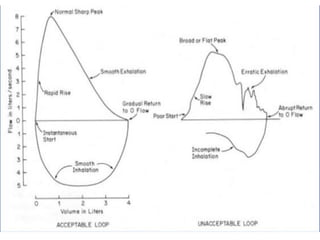
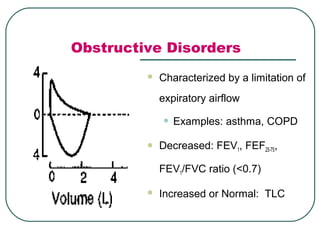
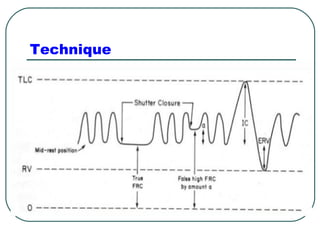
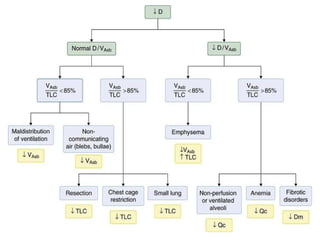
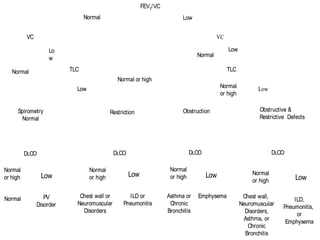
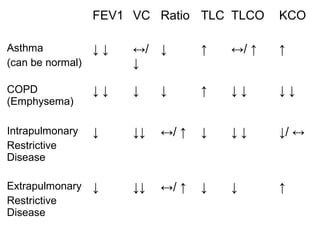
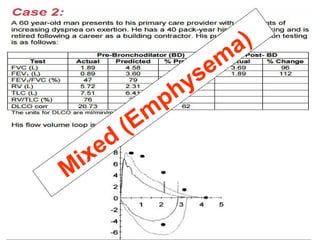
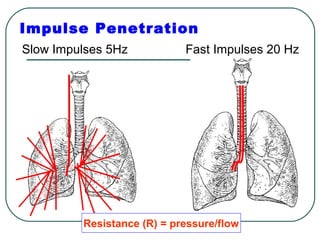
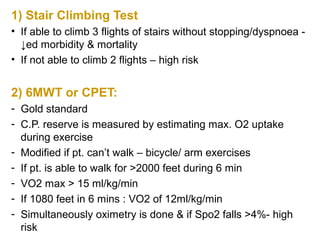
The document provides a comprehensive overview of pulmonary anatomy, physiology, and the principles of pulmonary function tests (PFTs). It includes discussions on lung volumes, capacities, and the significance of spirometry in diagnosing and managing respiratory conditions. Additionally, it outlines the indications, methods, and interpretations of various PFTs, while addressing contraindications and safety measures during testing.