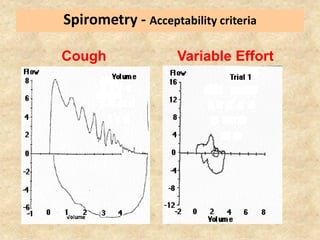
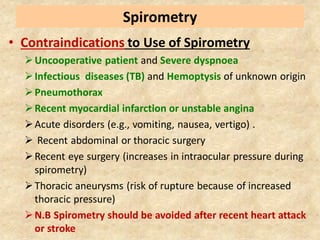
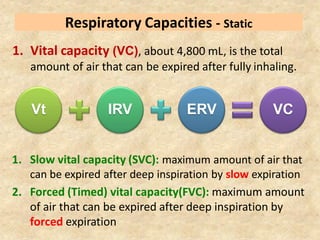
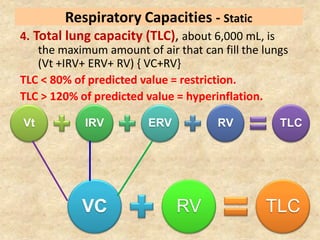
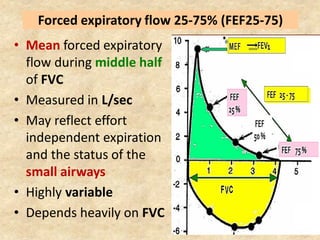
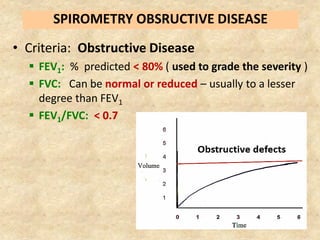
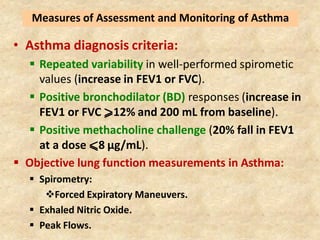
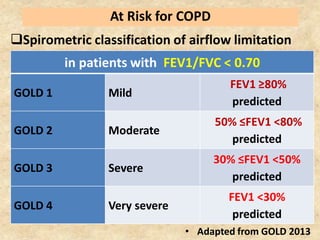
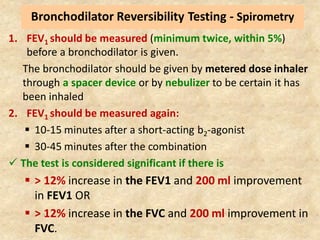
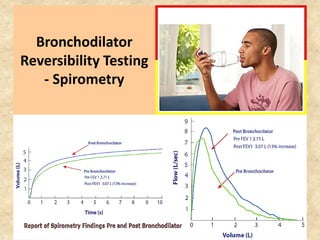
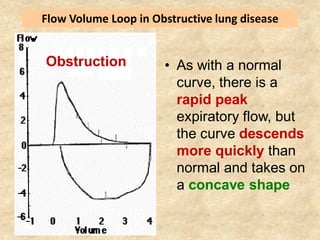
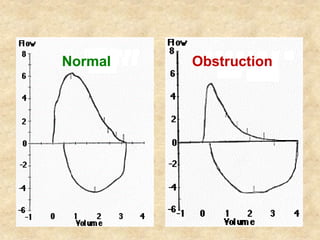
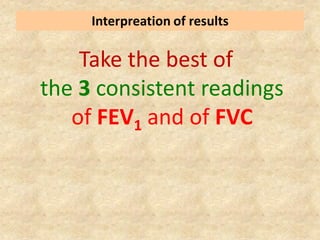
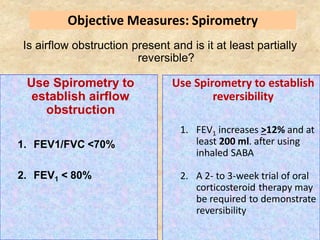
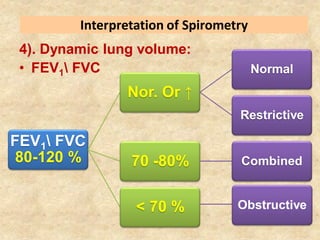
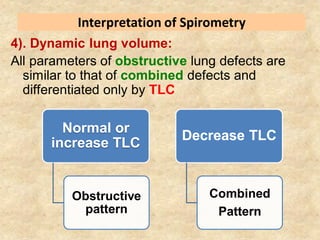
Pulmonary function tests (PFTs) such as spirometry help diagnose and monitor respiratory diseases. Spirometry measures expiratory volumes and flow rates through forced inhalation and exhalation into a mouthpiece. For a test to be valid, exhalation must be smooth, continuous for 6 seconds, and meet reproducibility criteria of two largest FVC and FEV1 values within 0.2 L of each other. PFTs can detect restrictive and obstructive lung diseases and assess response to treatment.