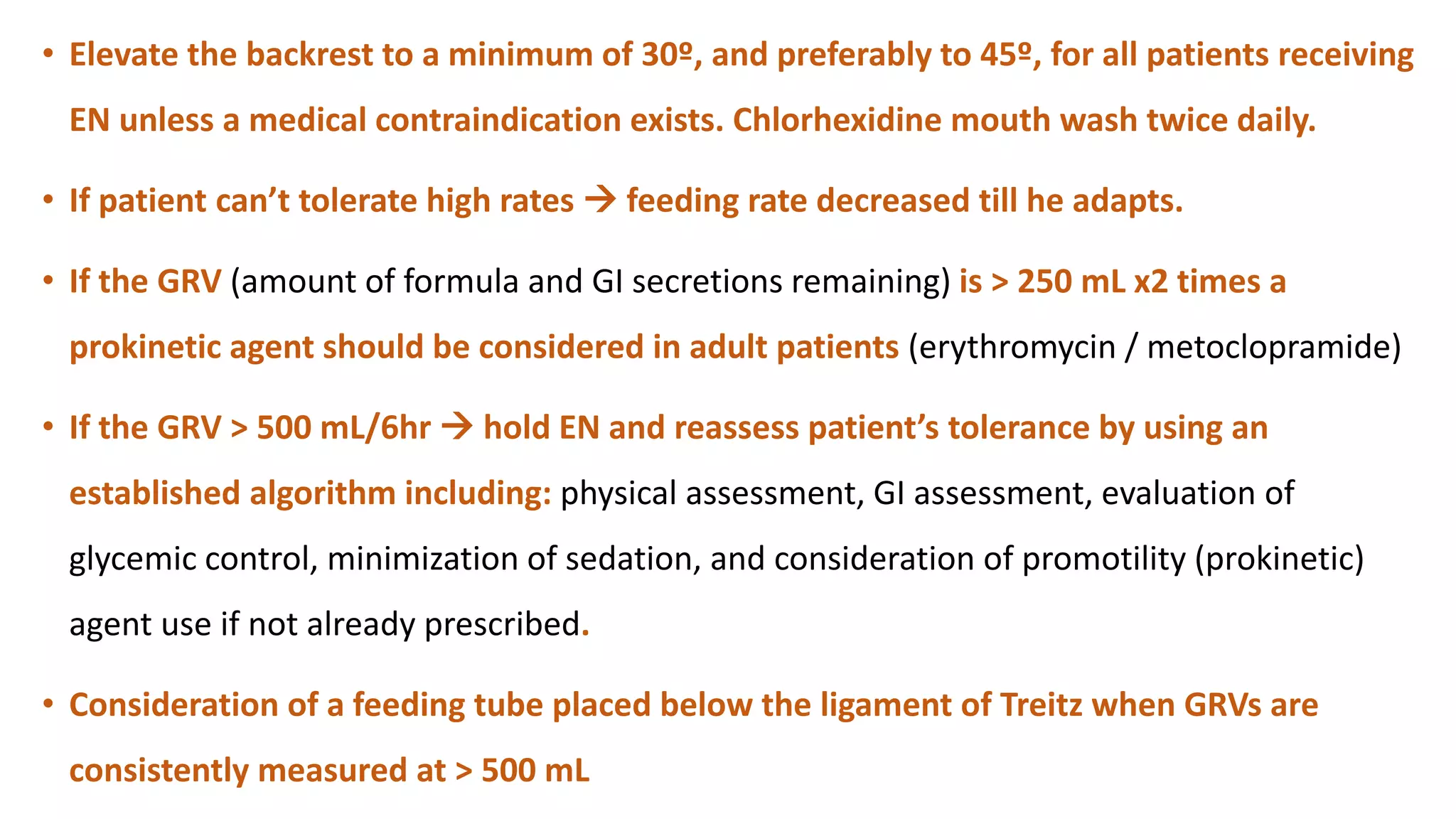
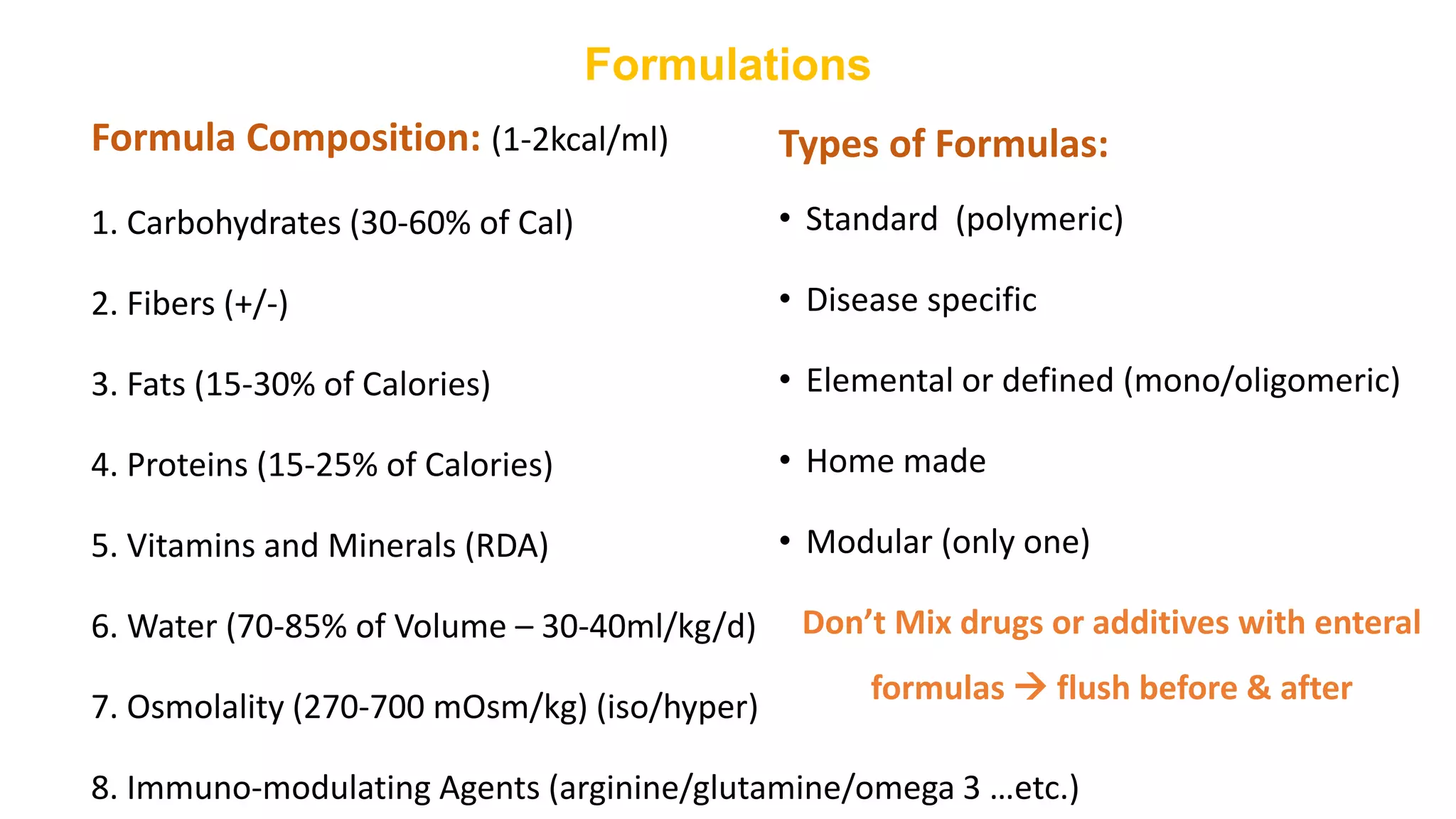
The document discusses enteral nutrition in ICU patients, noting the prevalence of malnutrition and the critical need for nutritional support via enteral or parenteral feeding. It highlights the benefits, indications, contraindications, and complications associated with enteral feeding, alongside detailed protocols for tube placement and administration. The document emphasizes the importance of early nutritional intervention to improve patient outcomes and outlines considerations for different delivery methods and feeding regimens.