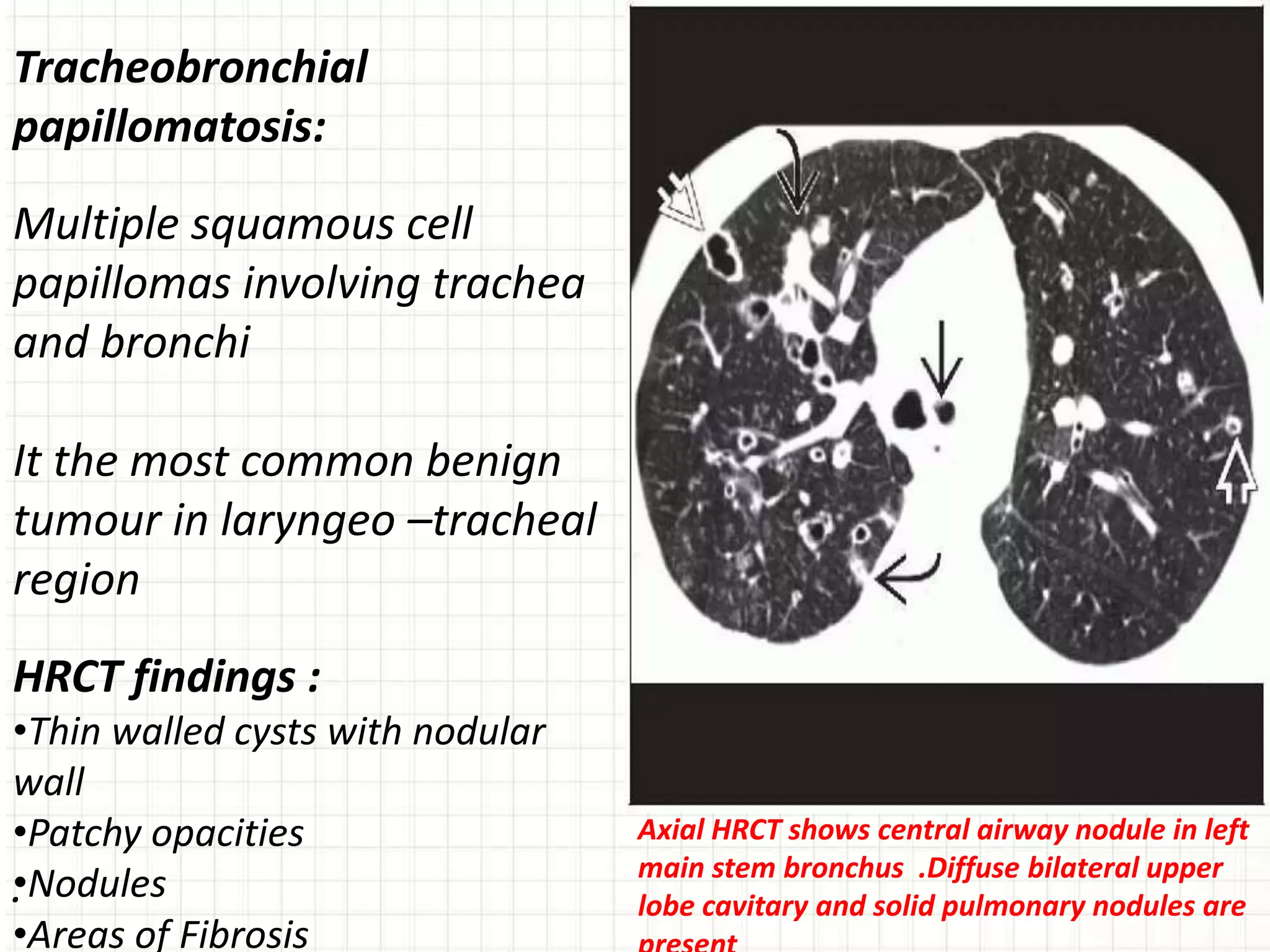
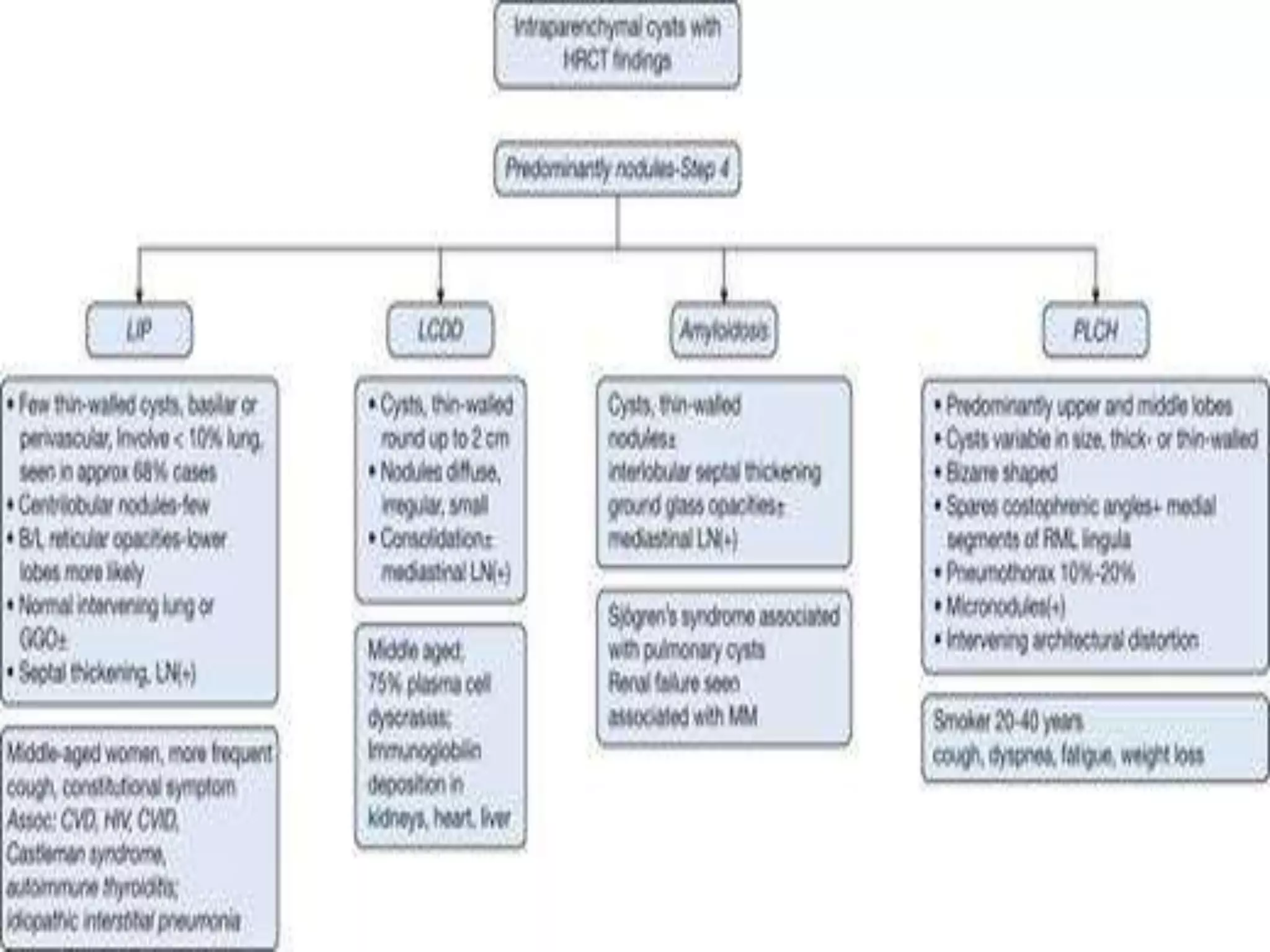
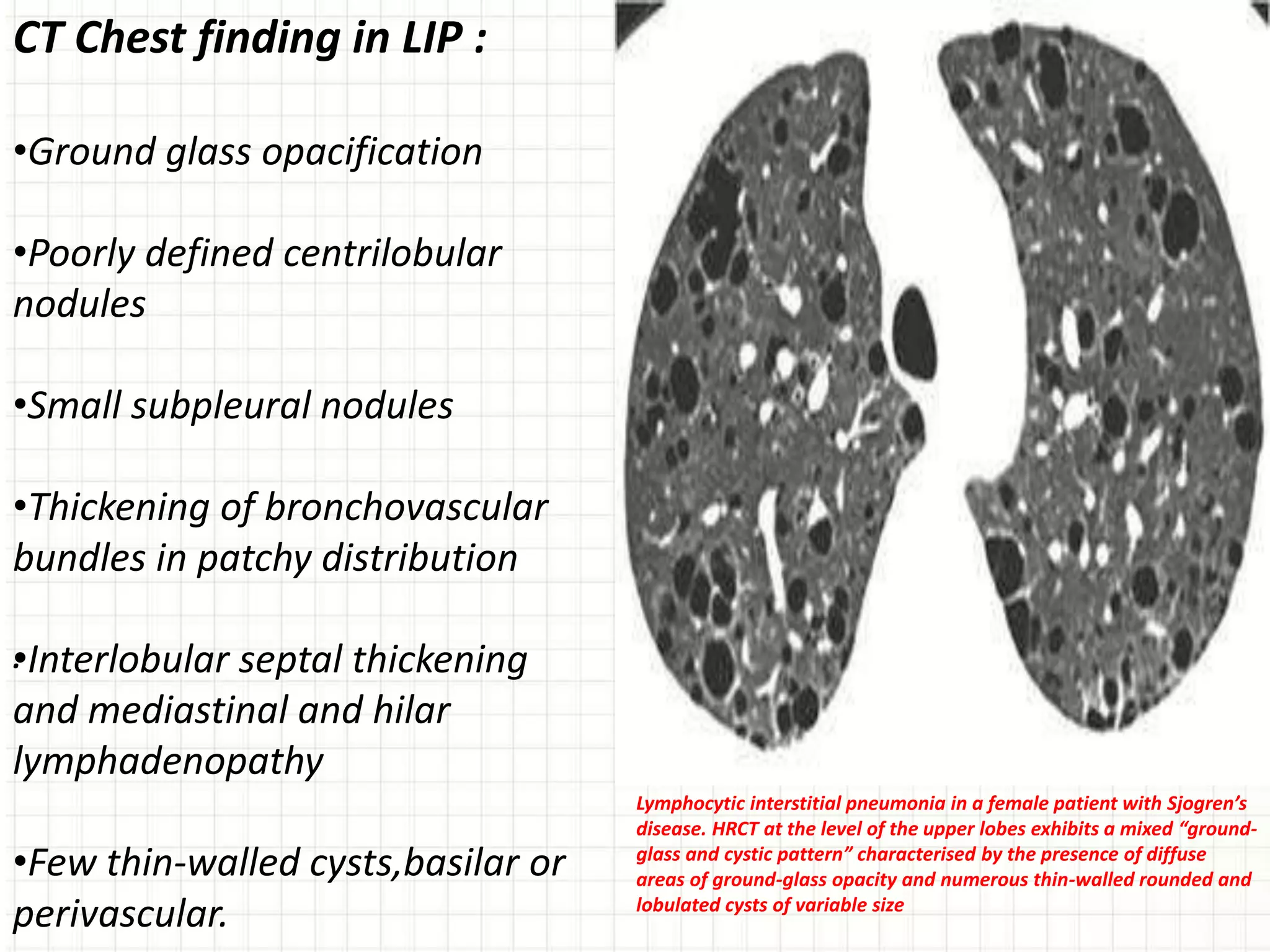
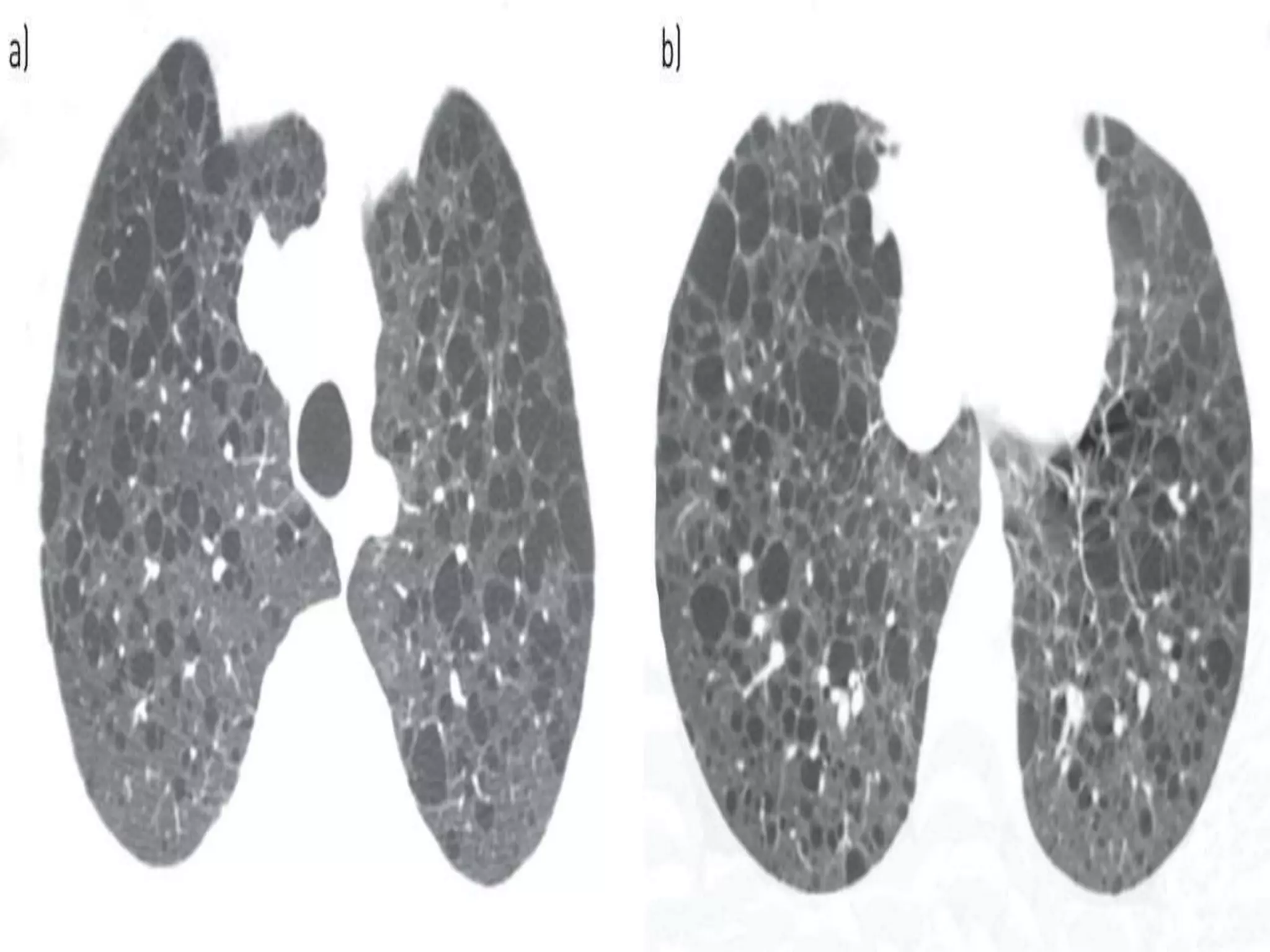
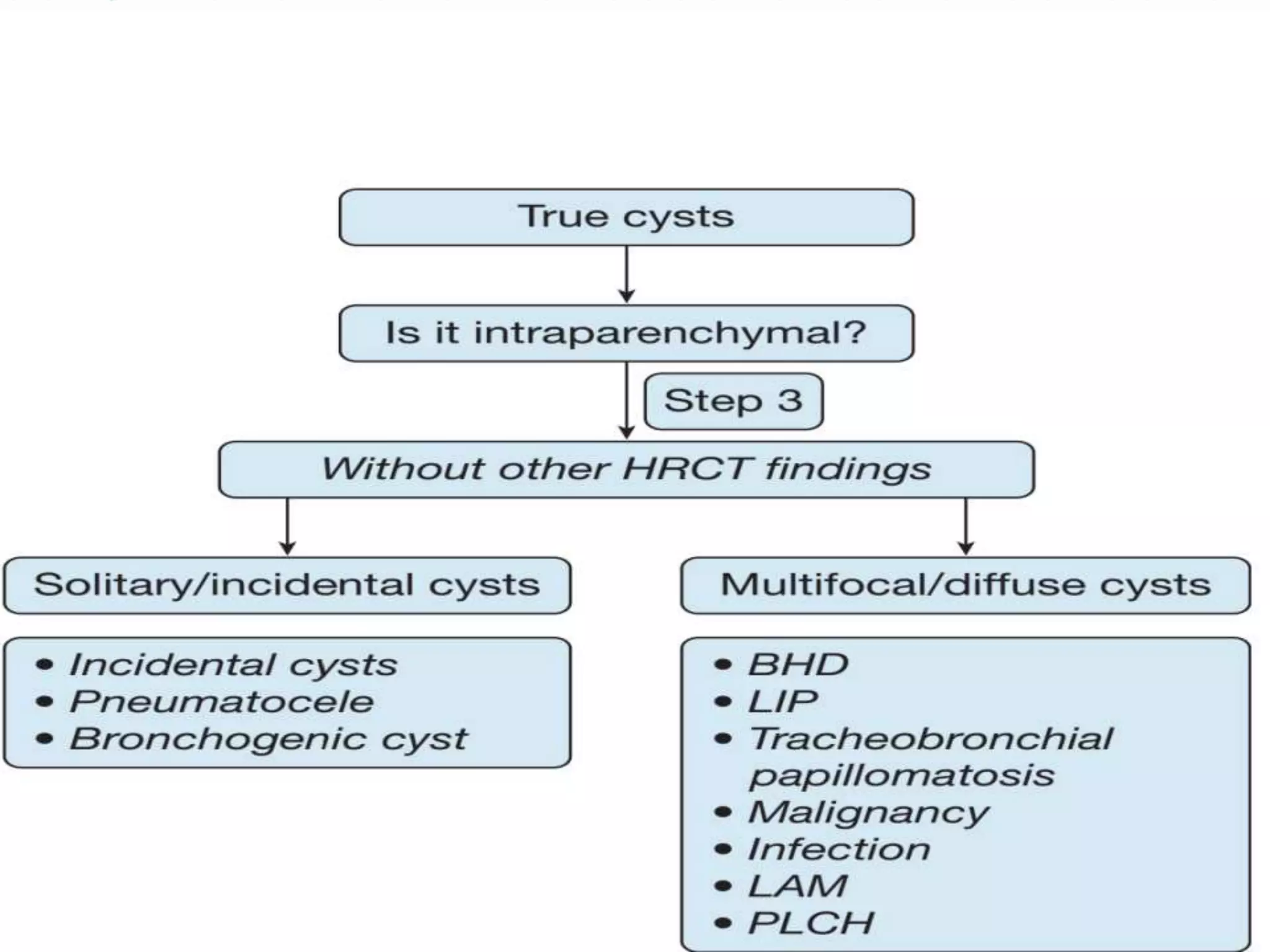
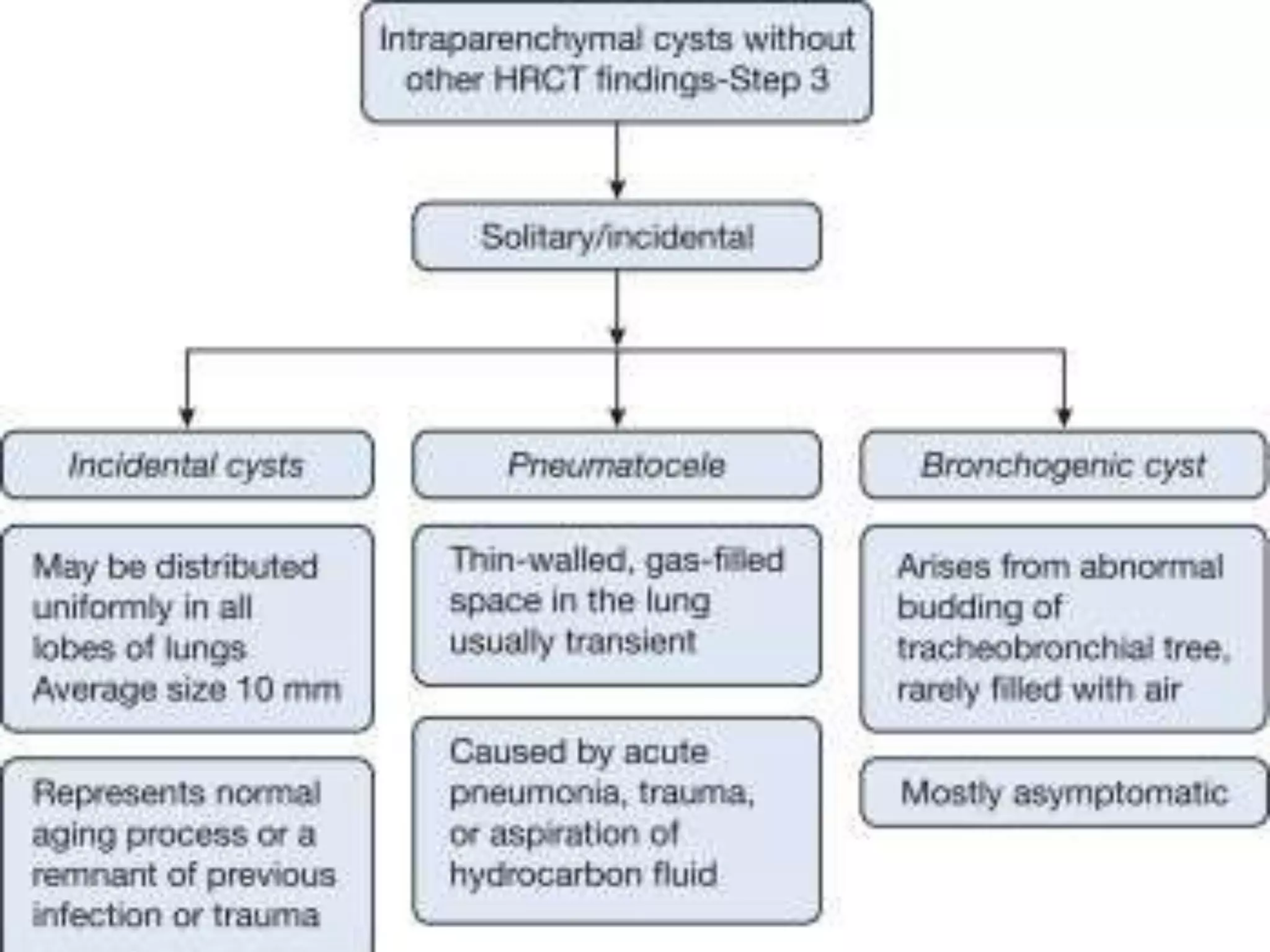
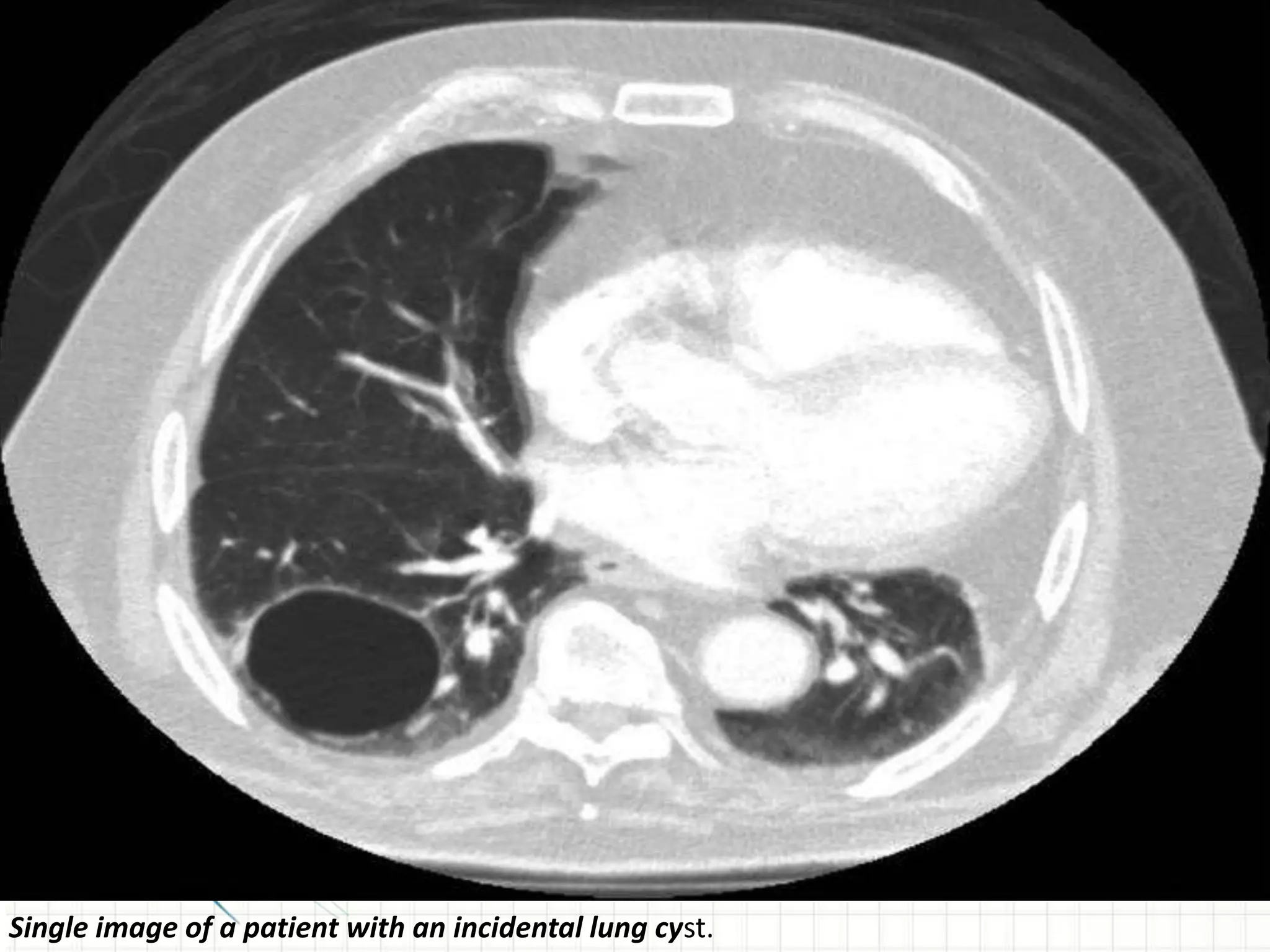
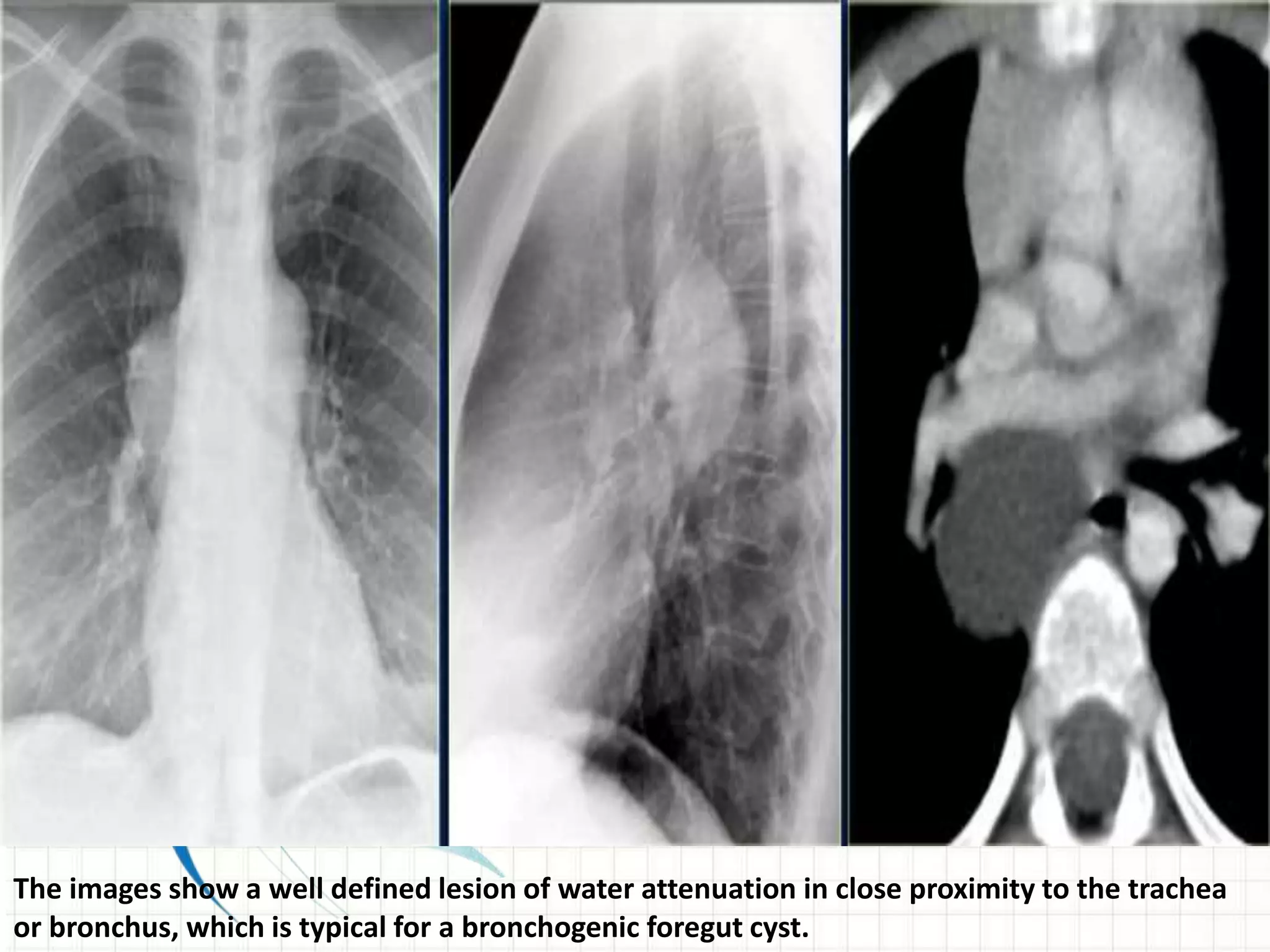
The document provides an overview of cystic lung diseases and discusses a systematic approach to evaluating cystic lung lesions on CT scans. It begins by defining pulmonary cysts and differentiating them from cavities. It then categorizes cysts based on their location, number, distribution, and associated CT findings. The document outlines a 5-question approach to systematically evaluate cystic lung lesions: 1) Are they true cysts? 2) Are cysts subpleural? 3) Are cysts solitary or multifocal without other findings? 4) Are cysts associated with nodules? 5) Are cysts associated with ground glass opacities? It then provides examples of specific diseases that present with various cyst patterns, such as



















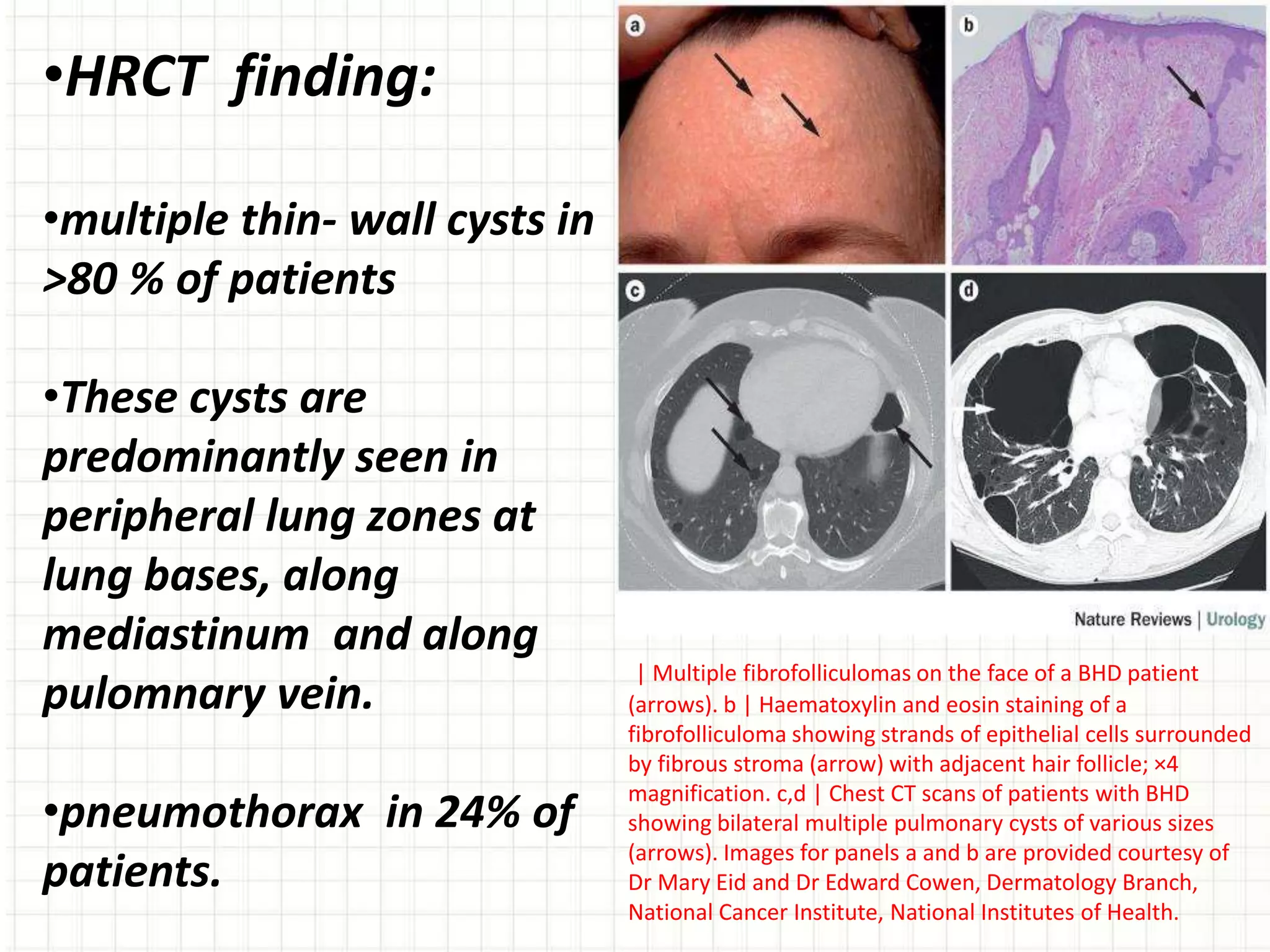
![What is BHD?
Birt-Hogg-Dubé syndrome (also known as BHD) is a hereditary
condition named after the three Canadian doctors that first
described it in 1977 – Arthur R. Birt, Georgina R. Hogg, and
William J. Dubé.
Birt-Hogg-Dubé syndrome is an autosomal dominant disorder
clinically manifested by fibrofolliculomas, renal cell carcinoma,
lung cysts, and spontaneous pneumothorax.
Cutaneous lesions are found in 82-92% of Birt-Hogg-Dubé
syndrome patients by age 25 years. [20, 21, 40, 44] Dermatologic
manifestations typically have an earlier onset than associated
renal cell cancer. Spontaneous pneumothorax develops most
frequently before age 40 years. [24]](https://image.slidesharecdn.com/cysticlungdiseases-170722190441/75/Cystic-Lung-Diseases-30-2048.jpg)
![Lymphangioleiomyomatosis:
(LAM) is a rare disorder resulting from proliferation in the lung, kidney,
and axial lymphatics of abnormal smooth muscle–like cells (LAM cells)
that exhibit features of neoplasia and neural crest origin.
Proliferation of lymphangioleiomyomatosis (LAM) cells may obstruct
bronchioles, possibly leading to airflow obstruction, air trapping,
formation of bullae, and pneumothoraces. Obstruction of lymphatics
may result in lymphangioleiomyomas, chylothorax, and chylous ascites.
Excessive proteolytic activity, which relates to an imbalance of the
elastase/alpha1-antitrypsin system or metalloprotease (MMPs) and
their inhibitors (tissue inhibitors of metalloproteases [TIMPs]), may be
important in lung destruction and formation of cysts.](https://image.slidesharecdn.com/cysticlungdiseases-170722190441/75/Cystic-Lung-Diseases-33-2048.jpg)