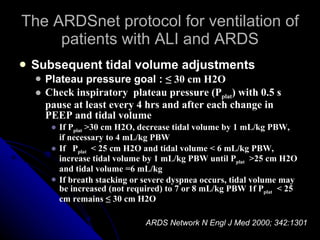
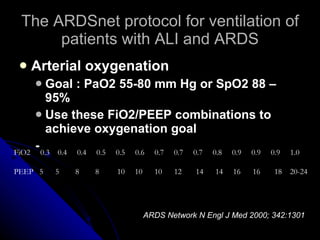
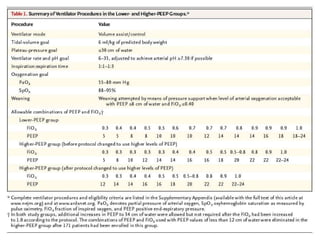
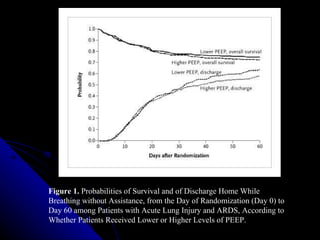
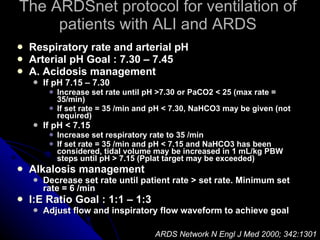
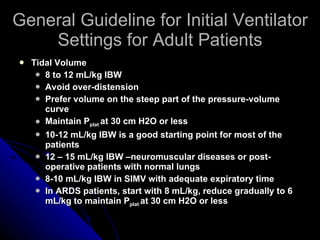
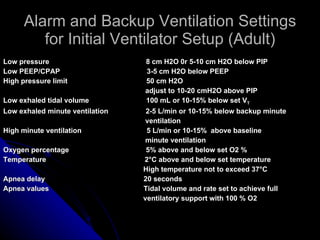
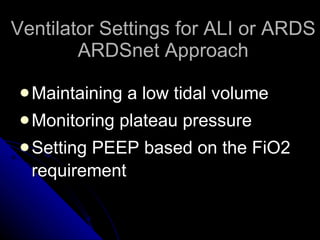
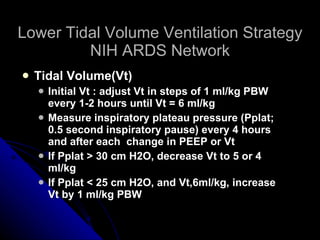
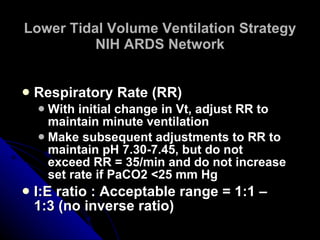
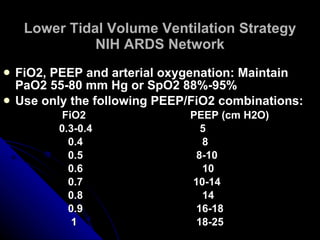
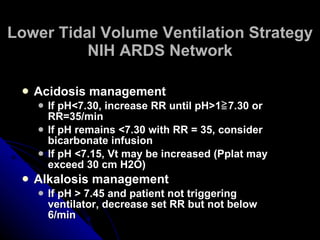
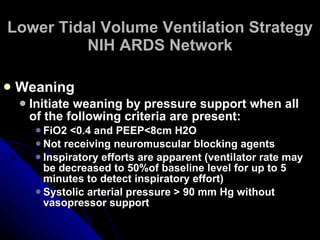
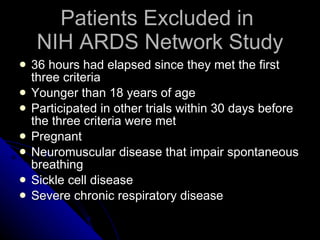
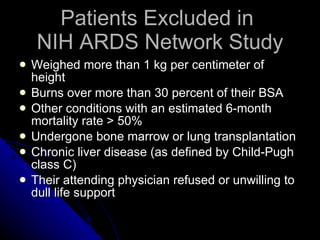
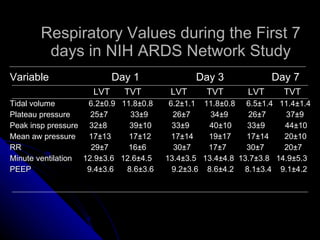
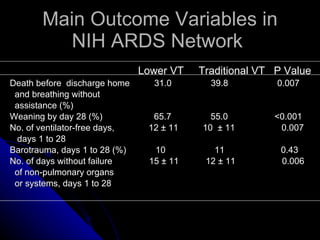
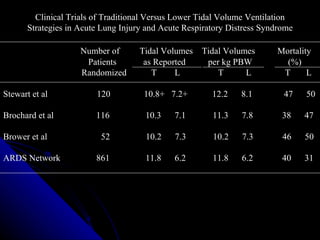
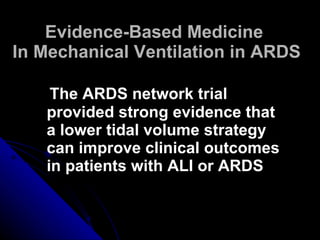
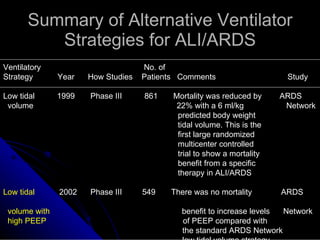
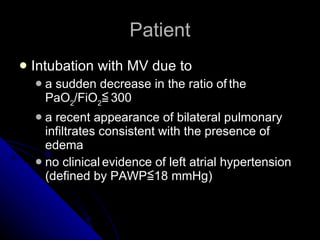
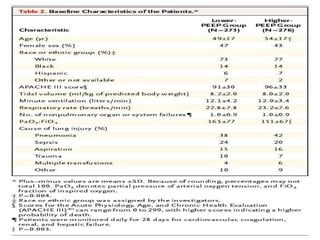
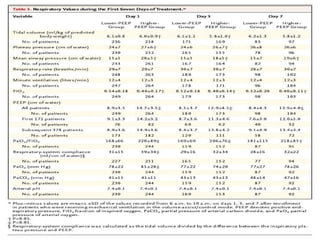
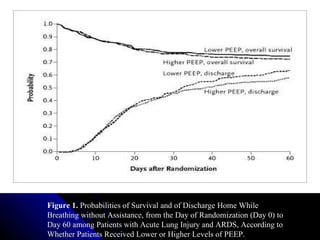
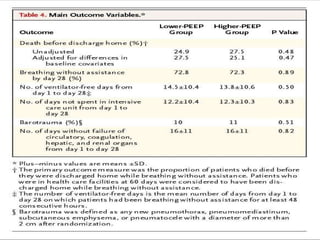
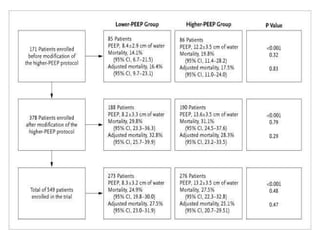
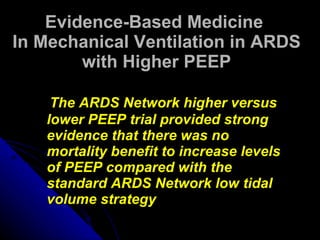
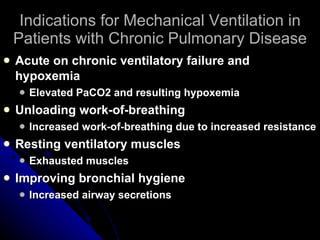
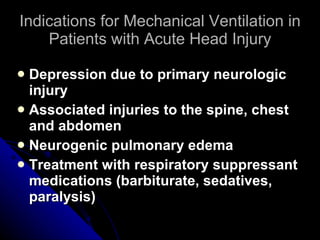
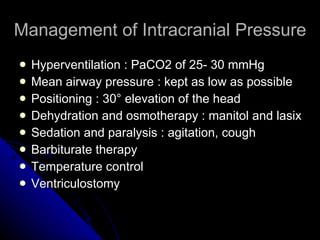
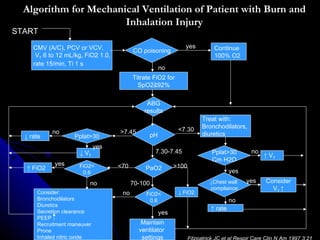
The document discusses ventilator management in different disease entities. It covers indications for mechanical ventilation in conditions like respiratory failure, ARDS, COPD, chest trauma, and head injury. For ARDS specifically, it summarizes the key findings of the NIH ARDS Network trial which demonstrated that a lower tidal volume strategy of 6 ml/kg predicted body weight reduced mortality compared to the traditional higher tidal volume approach.
![Lower Tidal Volume Ventilation Strategy NIH ARDS Network Calculate predicted body weight Male : PBW (kg) = 50 ± 2.3 [(height in inches)-60] = 50 ± 0.91[(height in cm) –152.4] Female : PBW (kg) = 45.5 ± 2.3 [(height in inches)-60] = 45.5 ± 0.91[(height in cm) –152.4] Ventilator mode : Volume assist/control until weaning](https://image.slidesharecdn.com/ventilatormanagementindifferentdiseaseentities-100330220411-phpapp01/85/Ventilator-Management-In-Different-Disease-Entities-9-320.jpg)
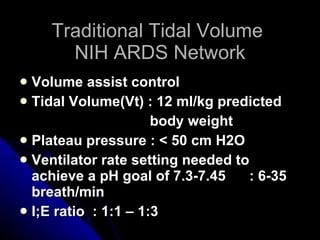
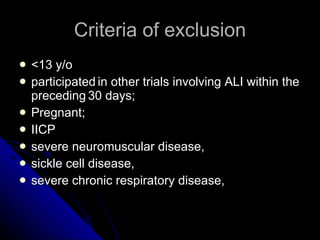
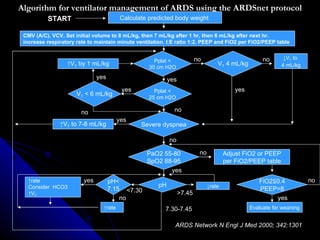


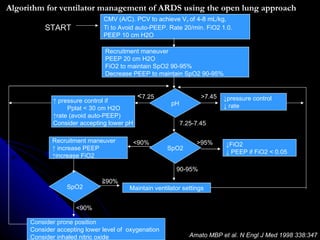
![The ARDSnet protocol for ventilation of patients with ALI and ARDS Initial ventilator tidal volume and rate adjustment Calculate predicted body weight Male = 50 + 2.3 [ht (in) – 60 ] kg Female = 45.5 + 2.3 [ht (in) – 60 ] kg Mode : volume Assist-Control Set initial tidal volume to 8 mL/kg PBW Reduce tidal volume to 7 mL/kg PBW after 1-2 hrs and then to 6 mL/kg PBW after a further 1-2 hrs Set initial ventilator rate to maintain baseline minute ventilation (not > 35 /min) ARDS Network N Engl J Med 2000; 342:1301](https://image.slidesharecdn.com/ventilatormanagementindifferentdiseaseentities-100330220411-phpapp01/85/Ventilator-Management-In-Different-Disease-Entities-70-320.jpg)