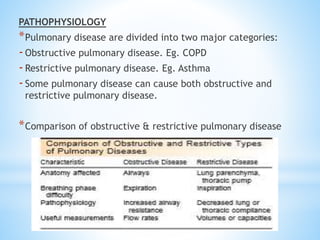
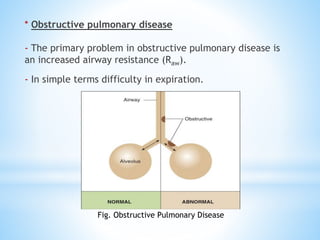
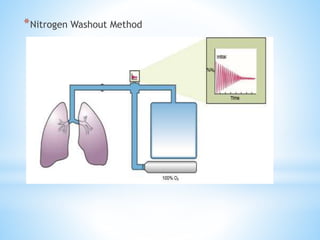
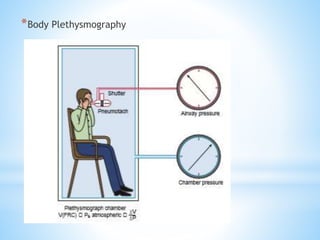
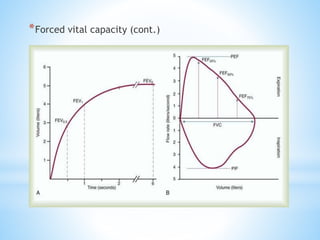
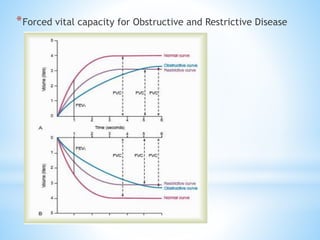
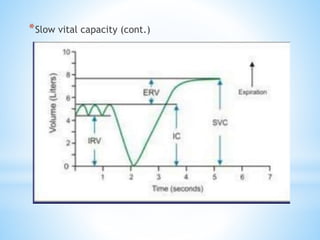
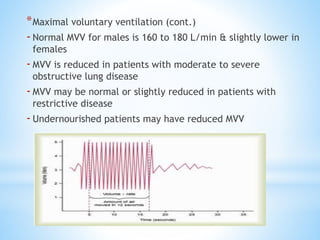
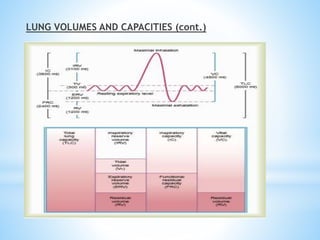
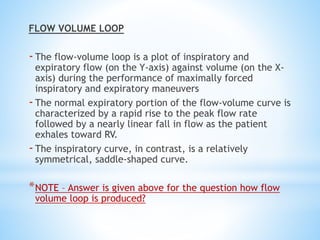
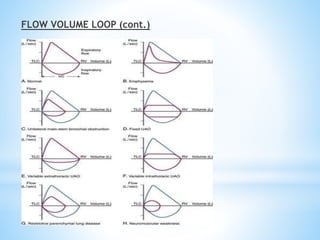
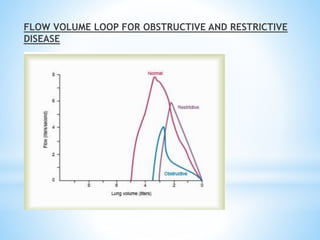
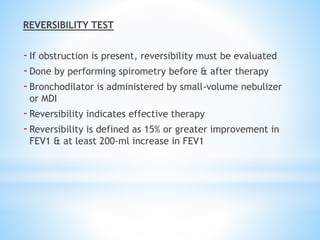
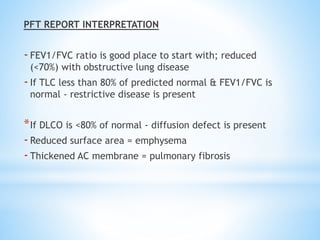
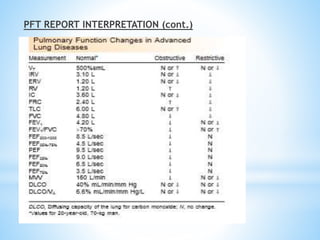
Pulmonary function tests (PFTs) measure lung function in three categories: dynamic air flow, lung volumes and capacities, and gas diffusion. PFTs identify and quantify changes from pulmonary disease, evaluate therapy effectiveness, and assess postoperative risk. Spirometry is the most common PFT and measures forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV1) to detect airway obstruction. Other PFTs include slow vital capacity, maximal voluntary ventilation, flow-volume loops, and reversibility testing with bronchodilators. PFT interpretation considers ratios like FEV1/FVC and compares values to predicted normals to diagnose obstructive or restrictive lung disease.