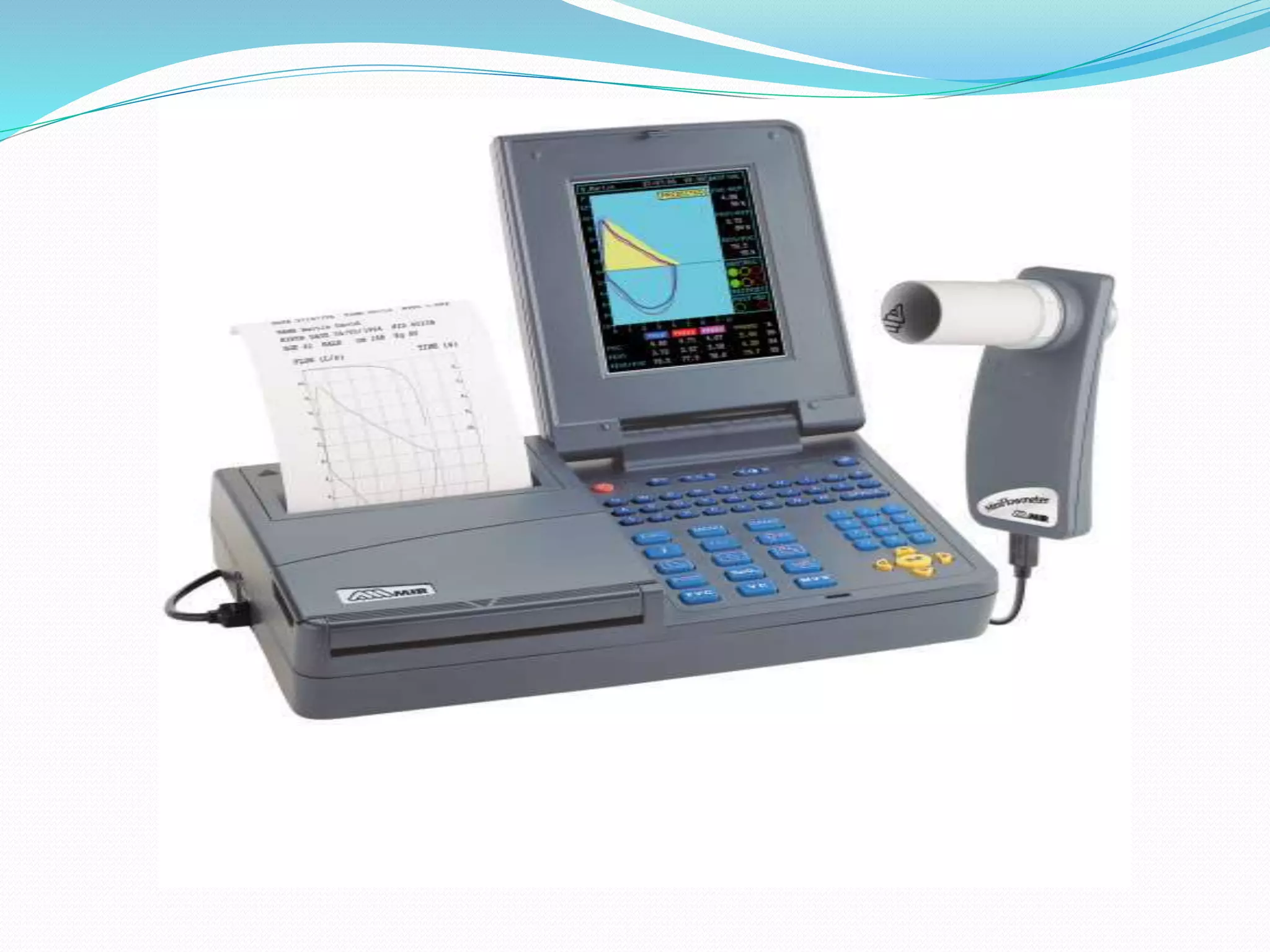
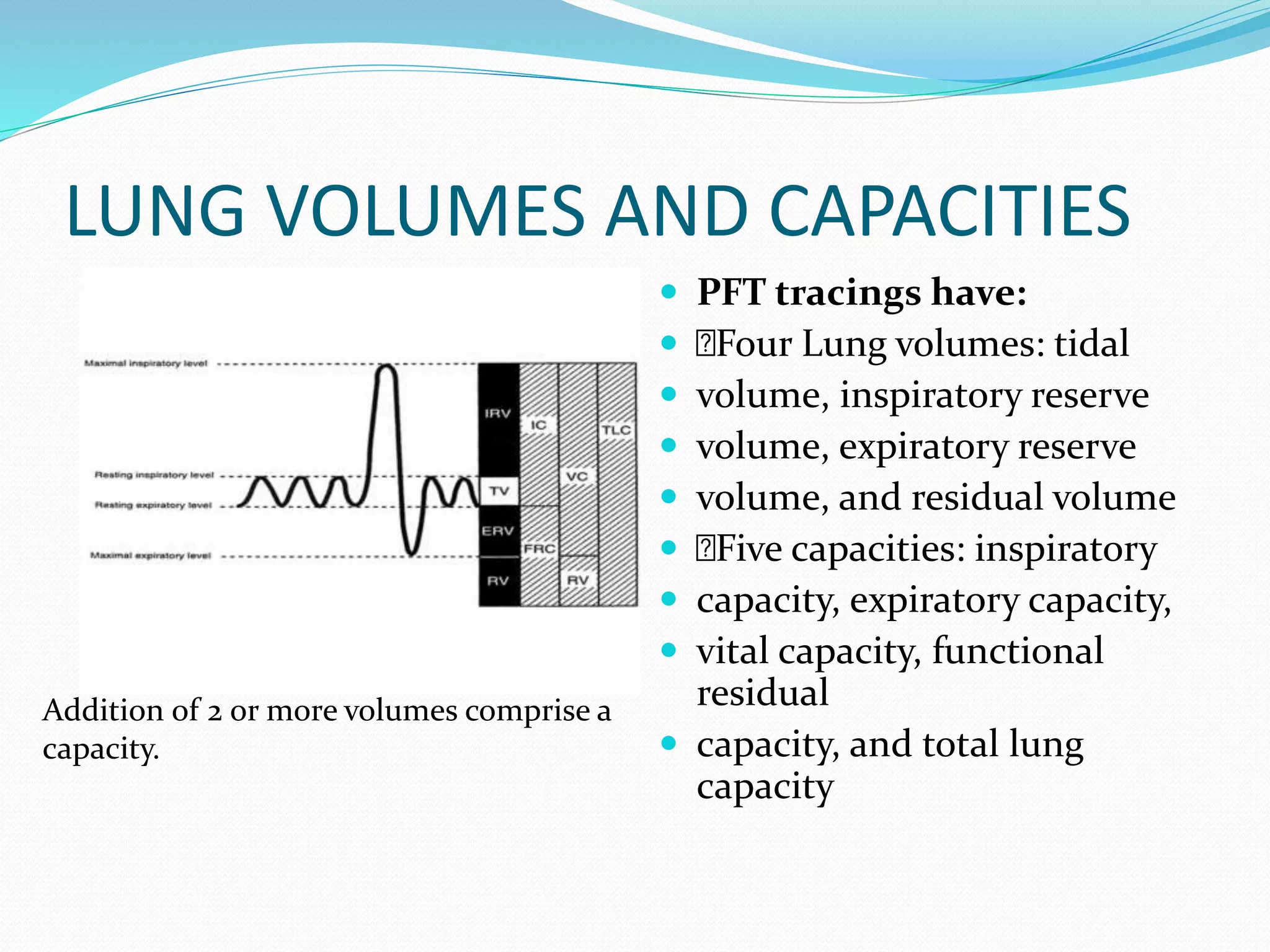
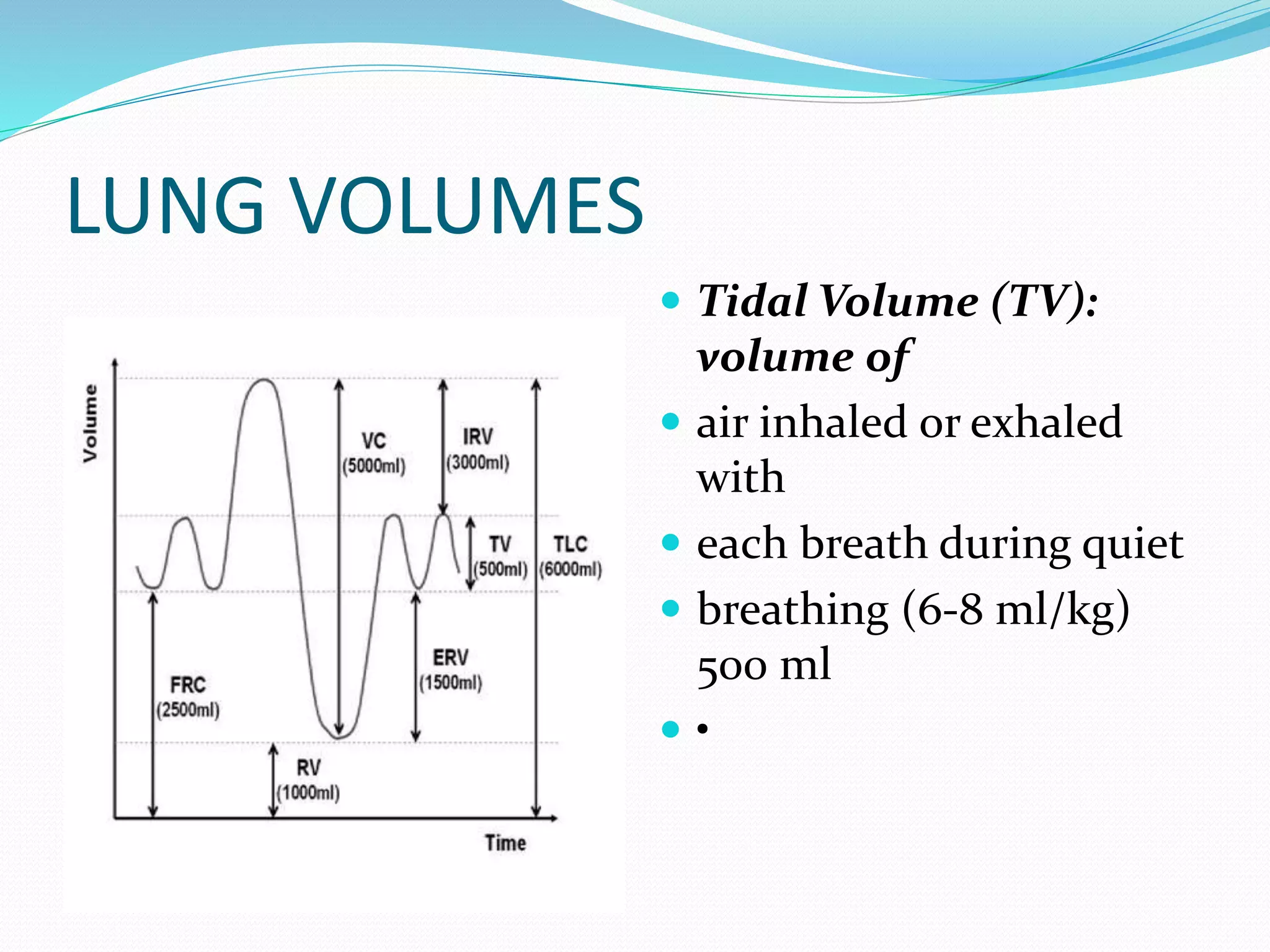
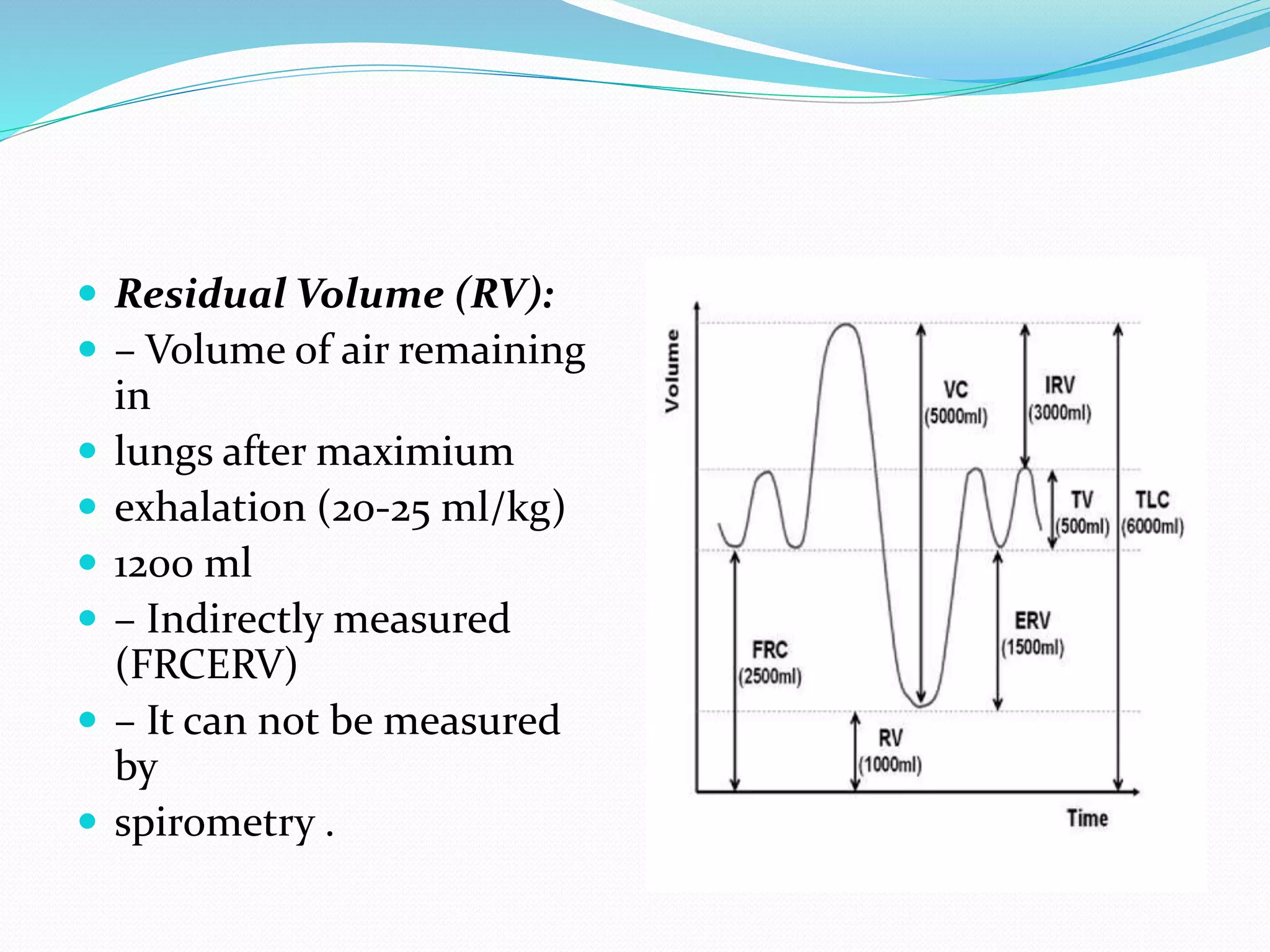
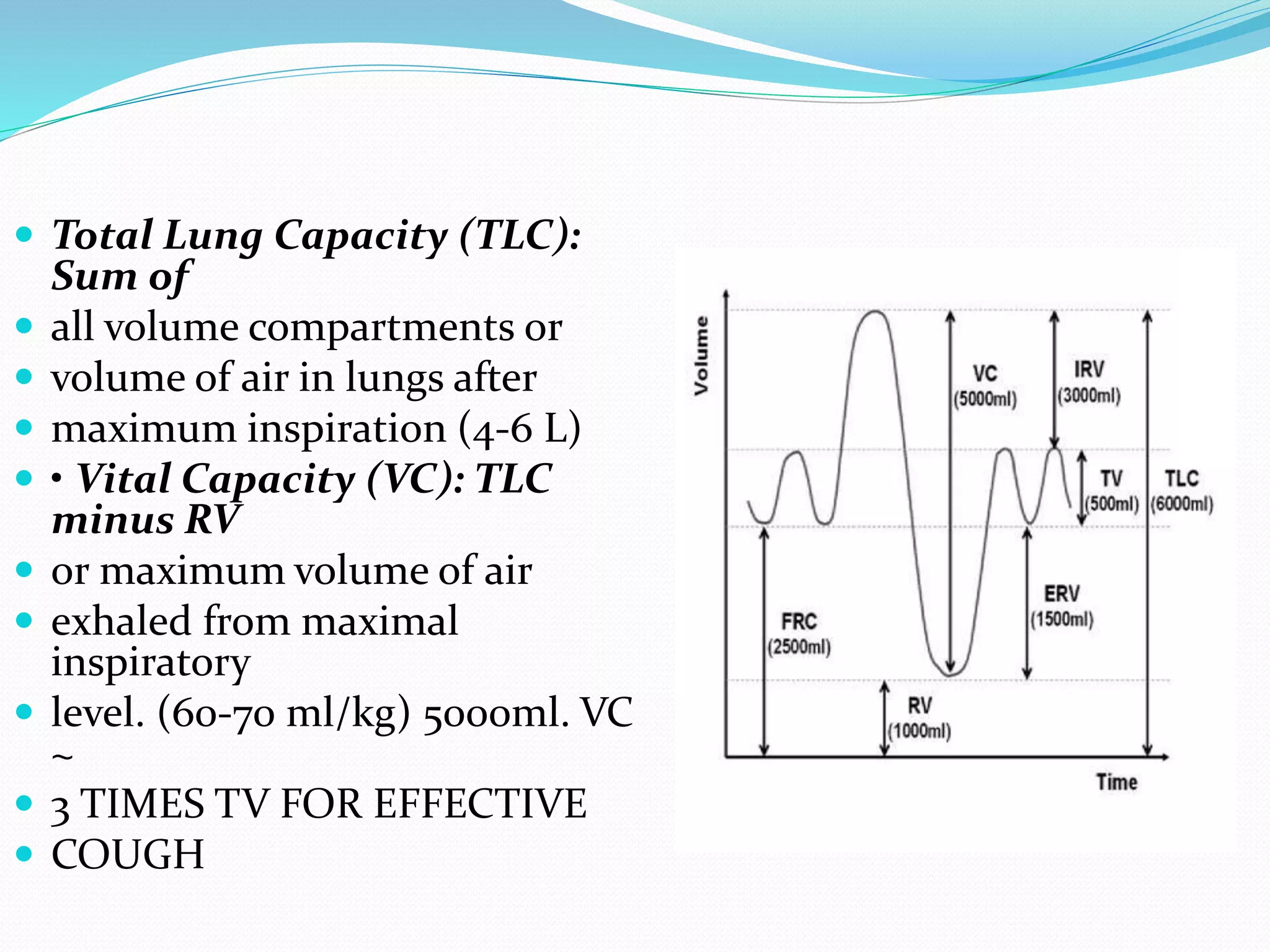
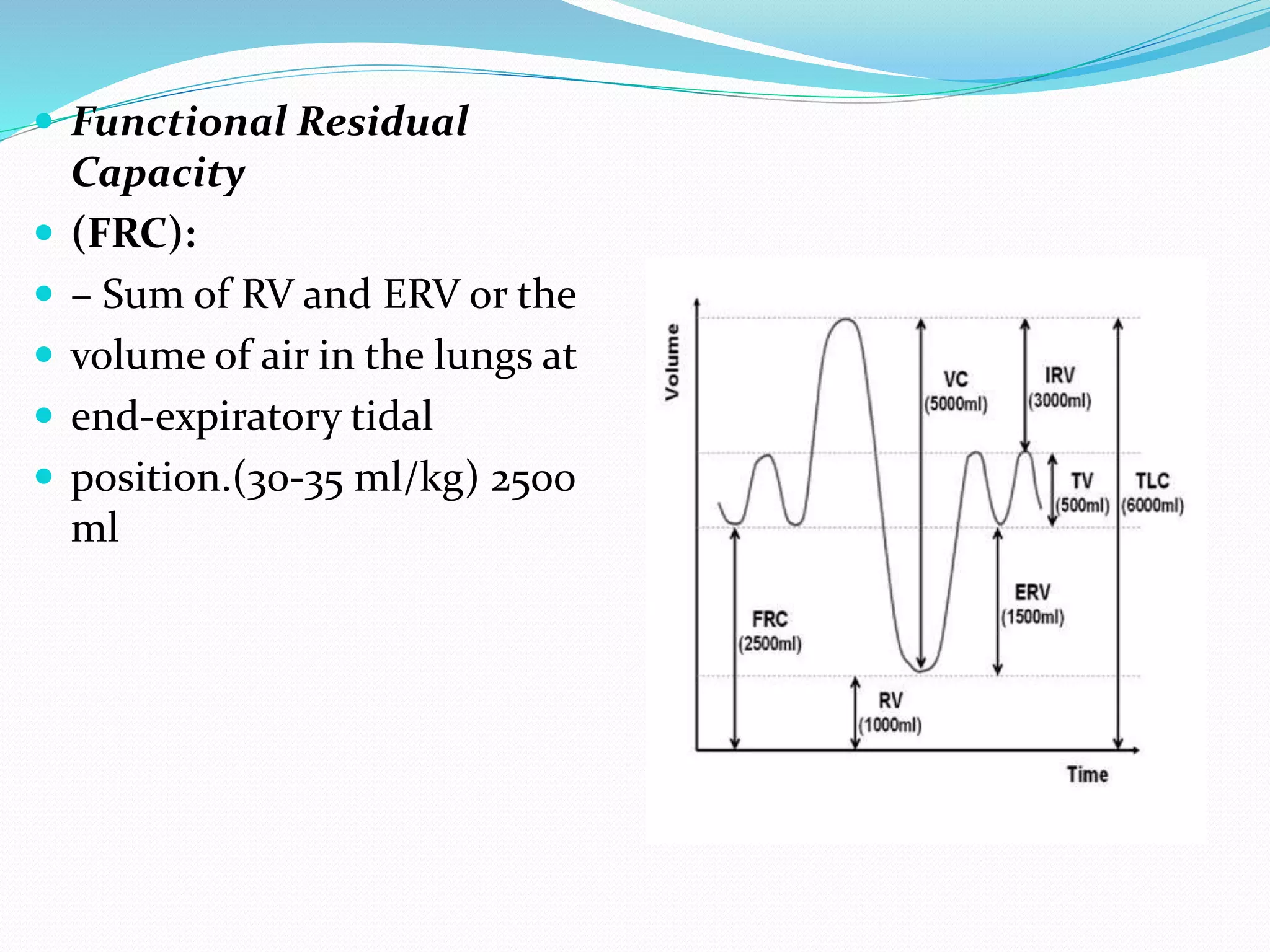
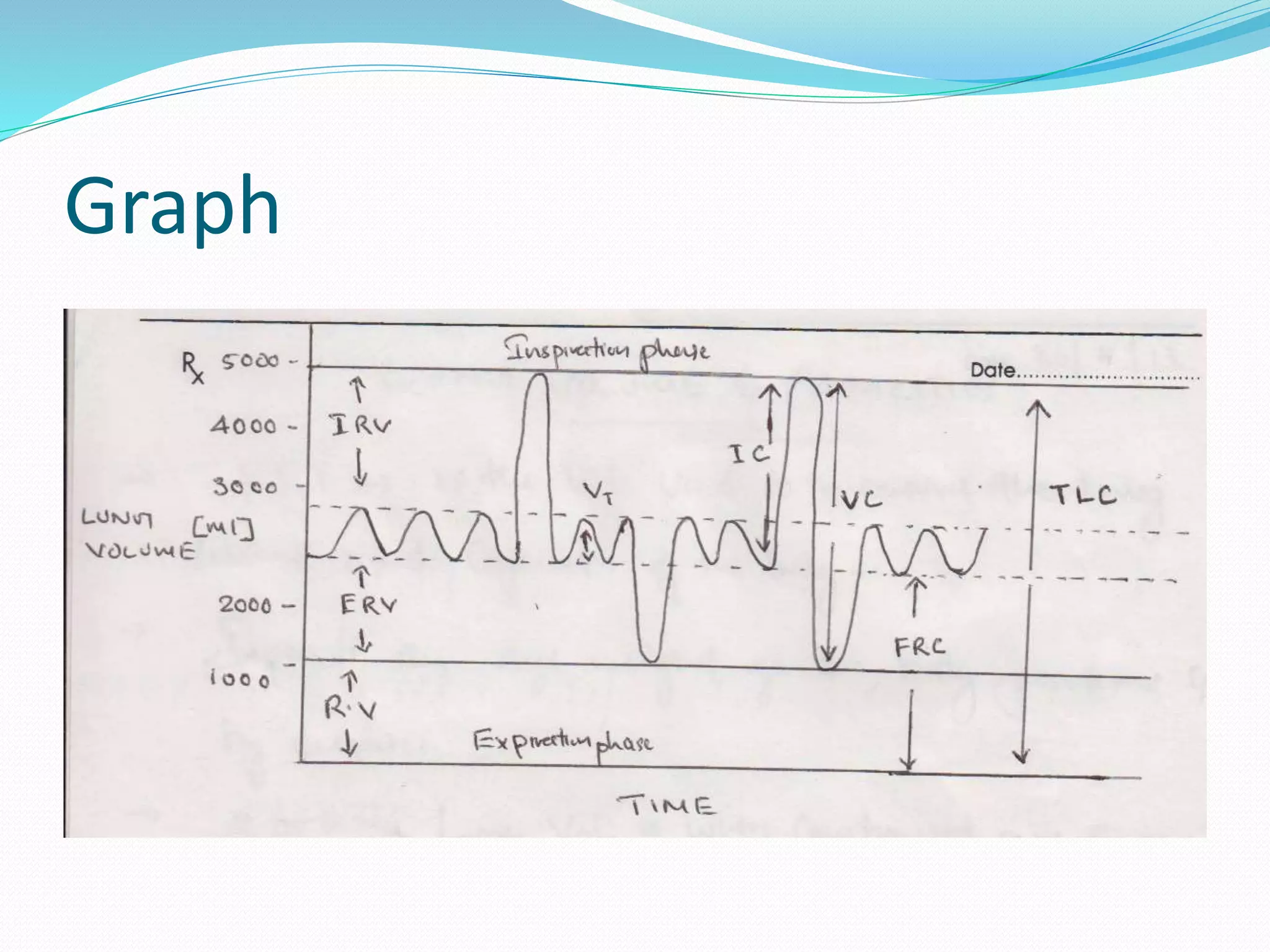
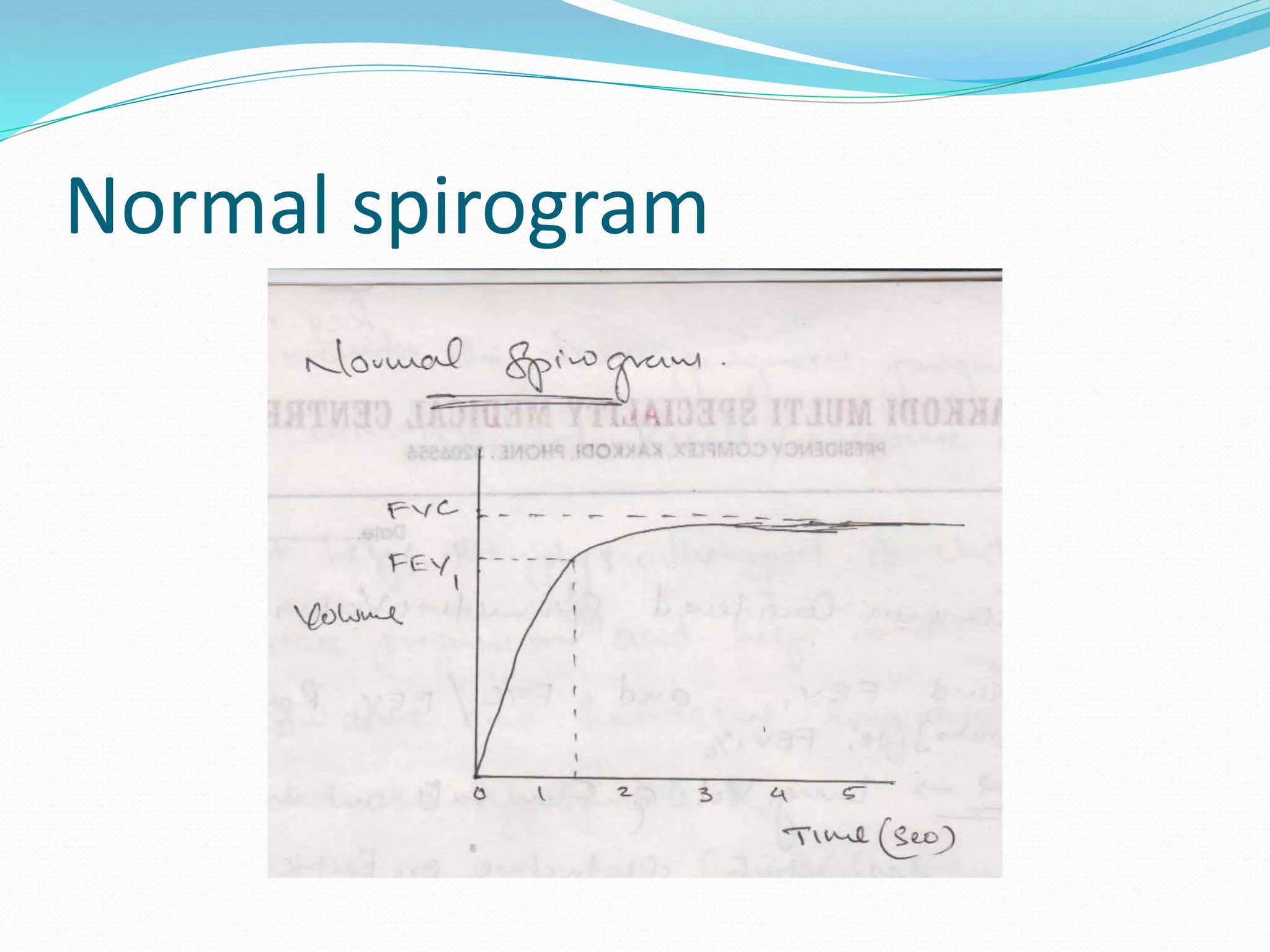
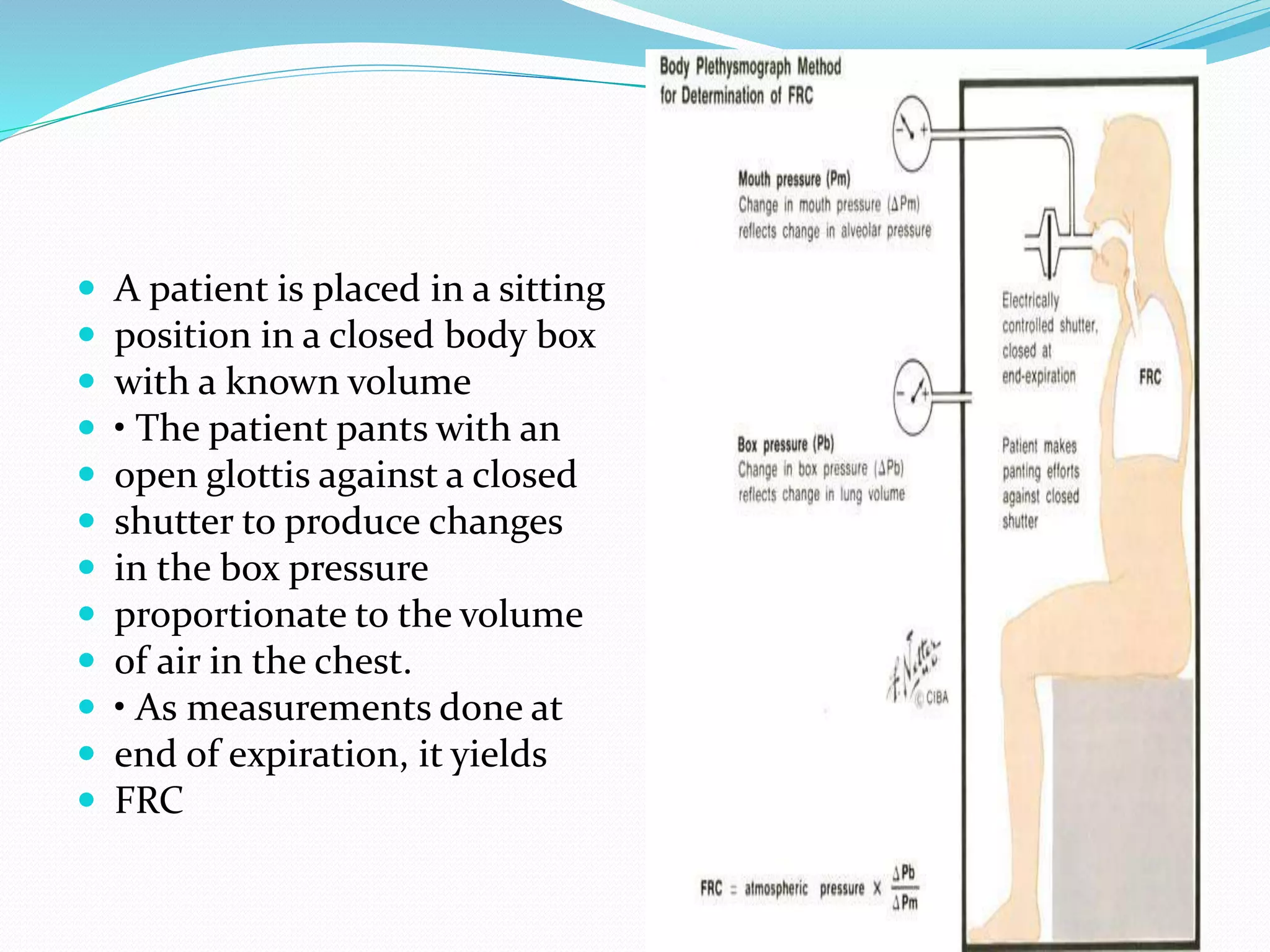
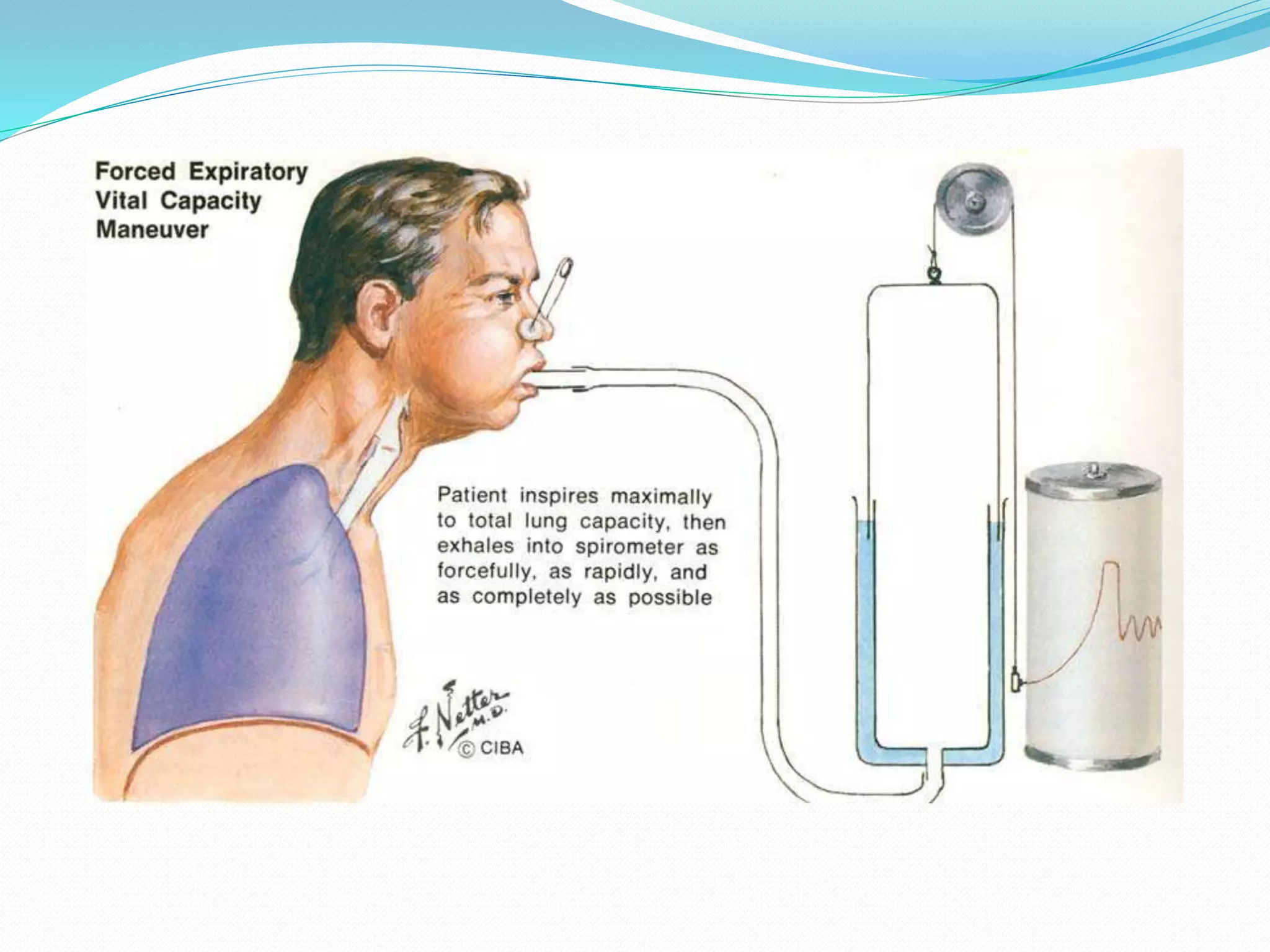
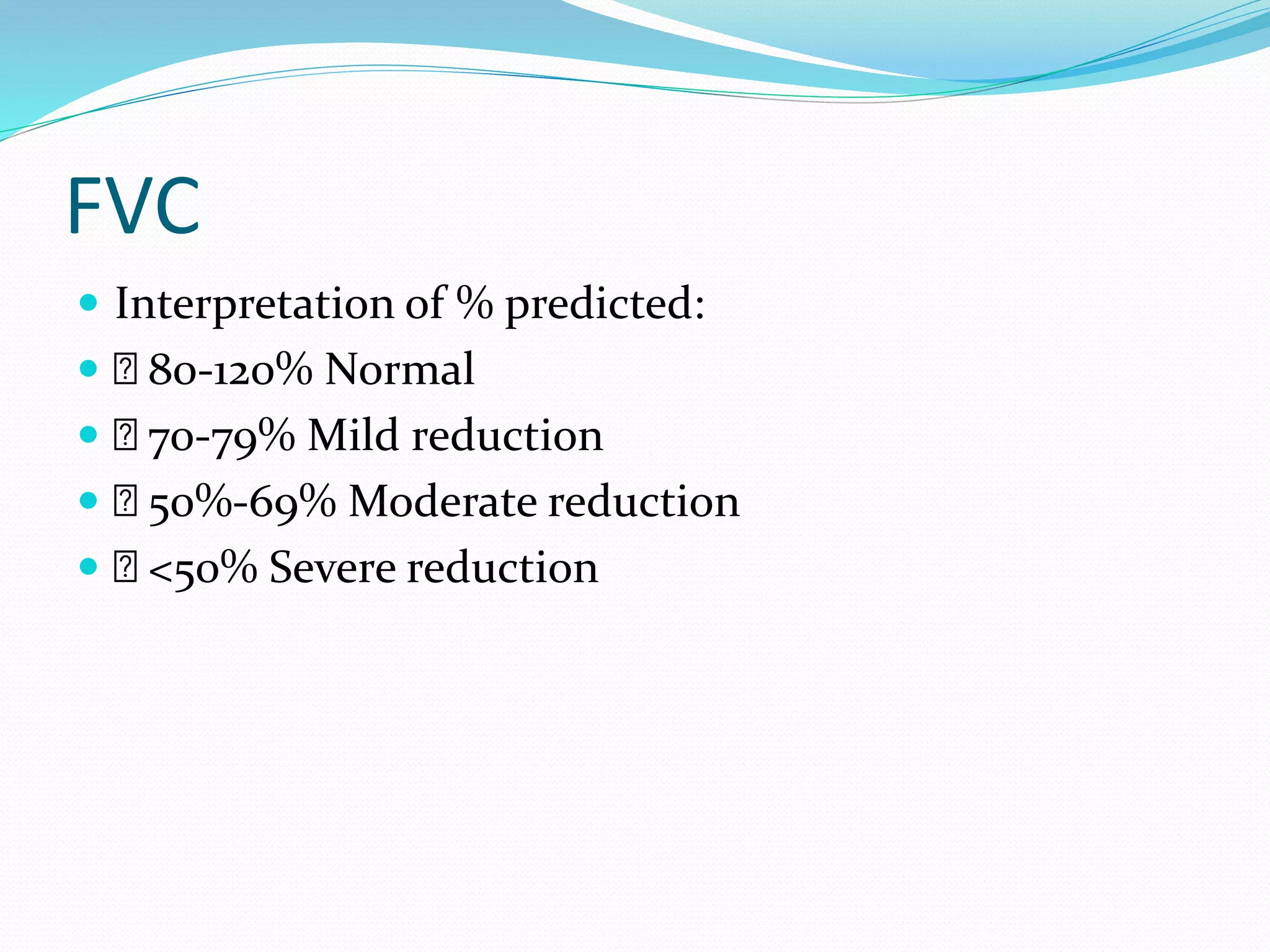
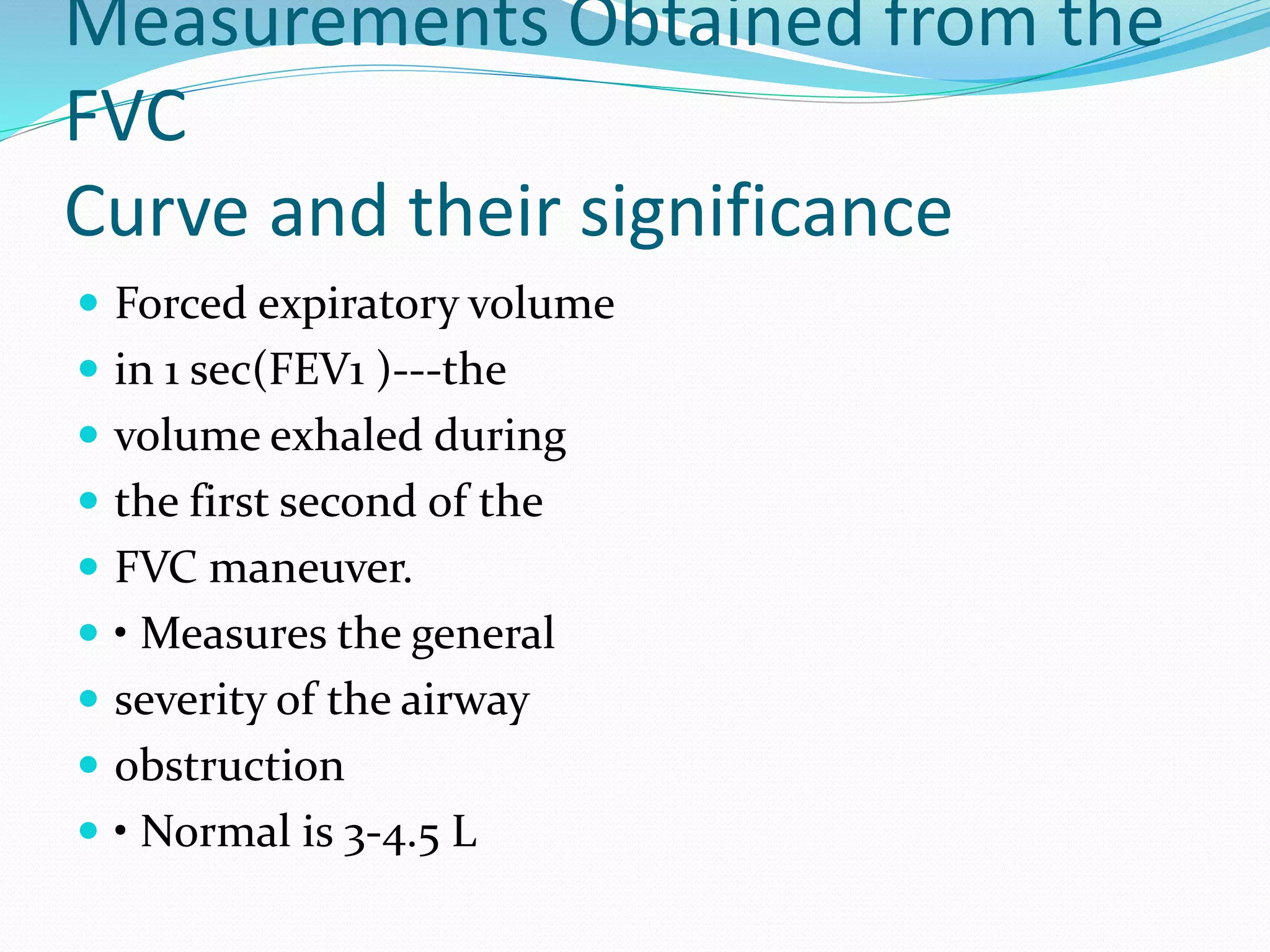
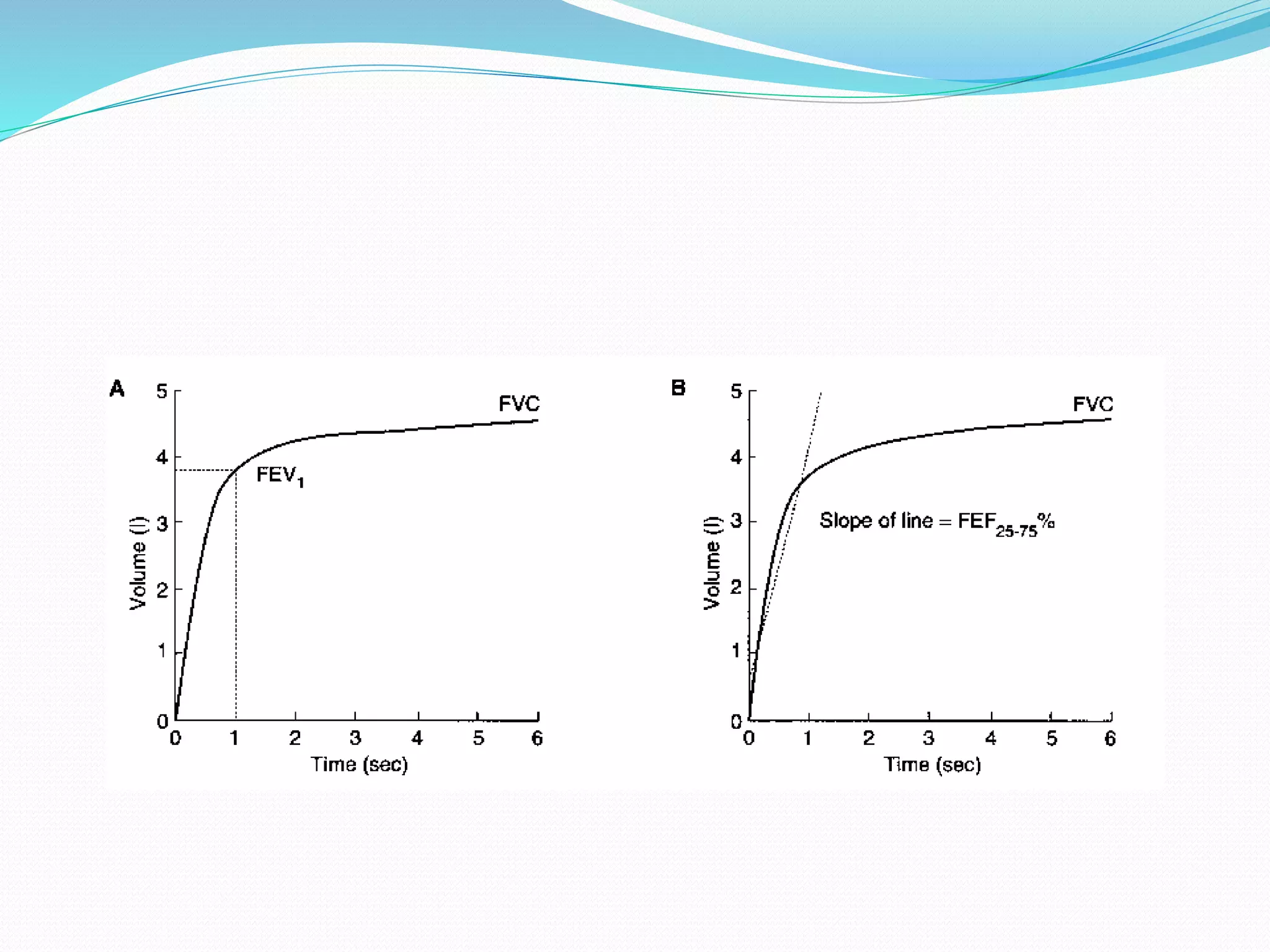
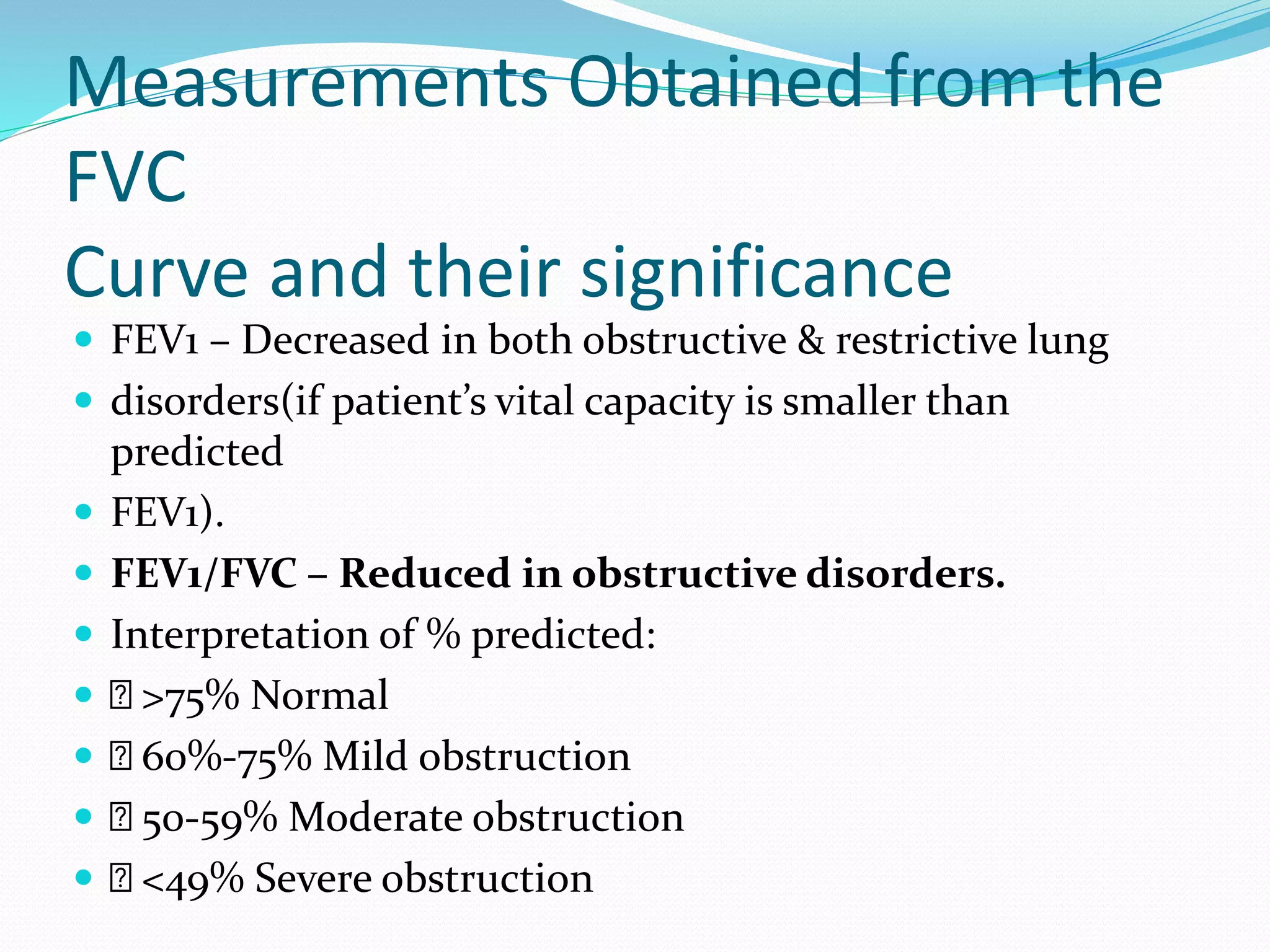
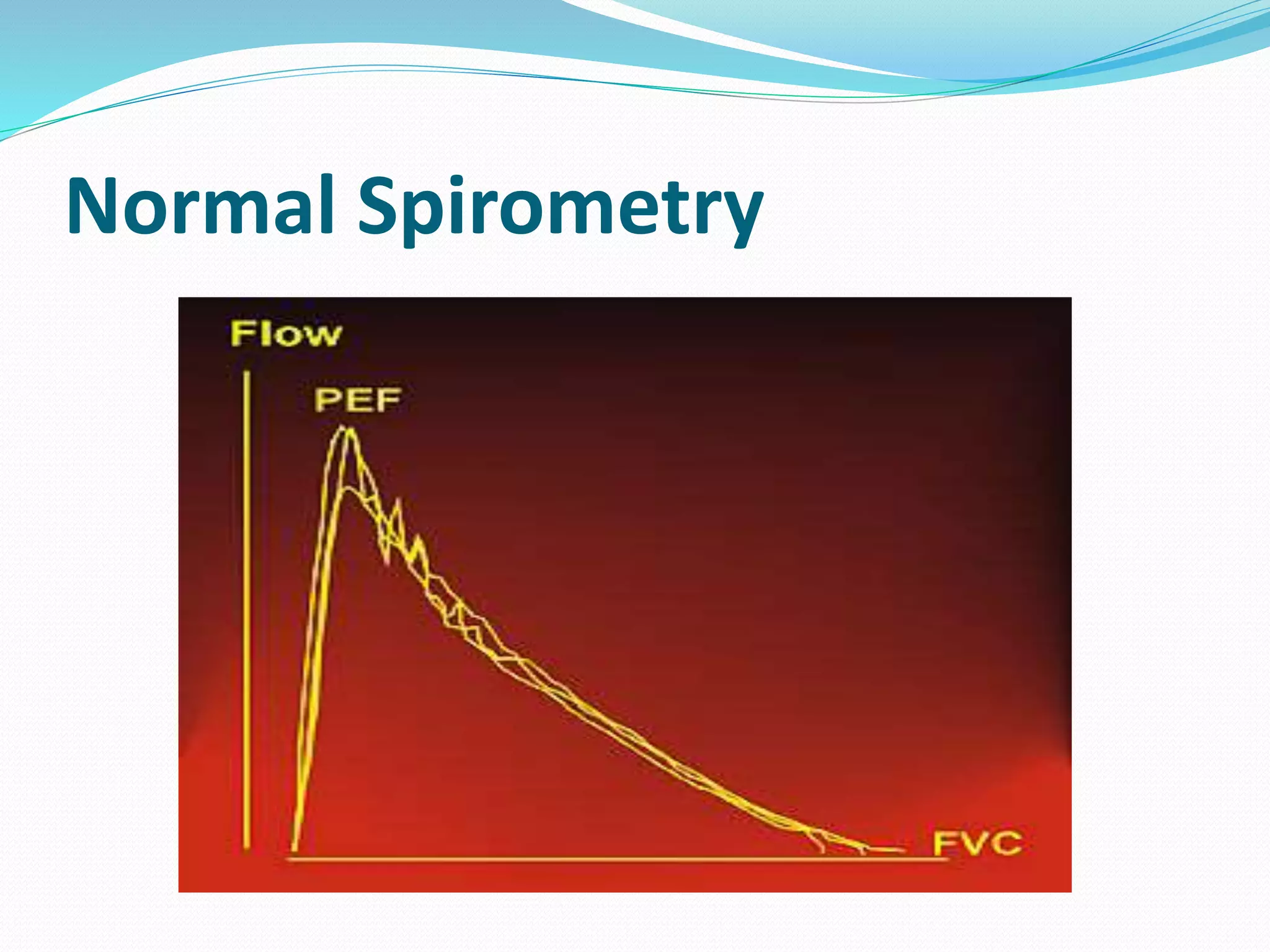
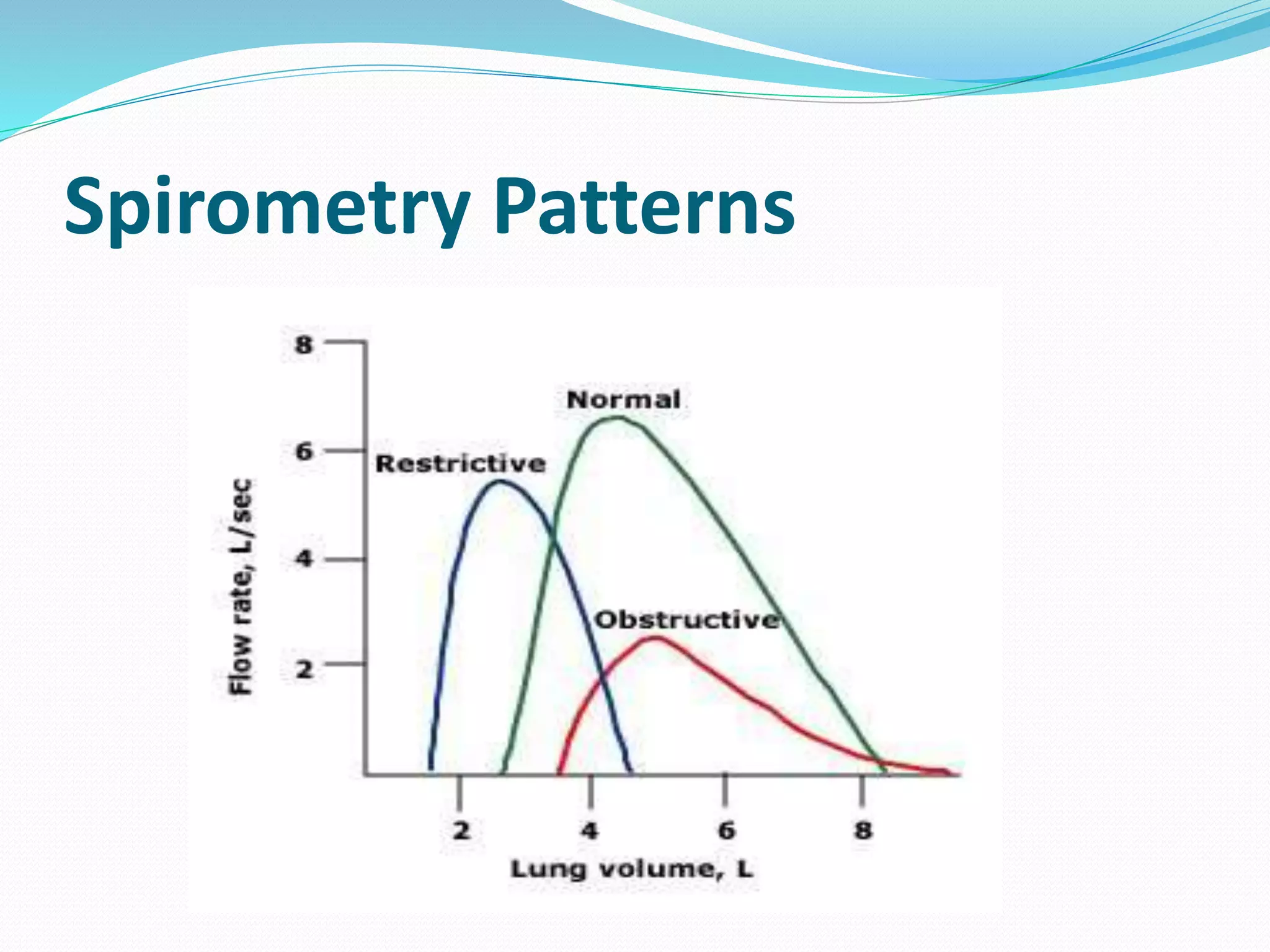
The document discusses pulmonary function tests (PFTs) designed to measure and evaluate lung function, including how well they take in and exhale air and transfer oxygen into the blood. It covers various aspects of PFTs such as spirometry, lung volumes and capacities, and diagnostic applications for respiratory conditions. The text illustrates how PFTs help distinguish between obstructive and restrictive lung problems and highlights important measurement values and their interpretations.