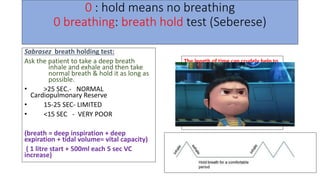
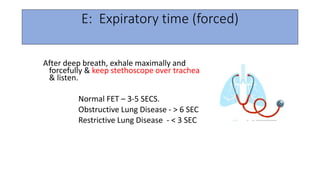
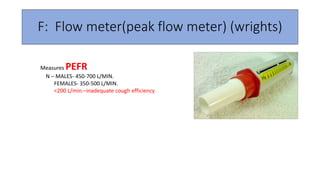
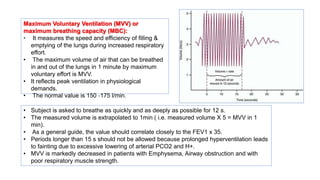
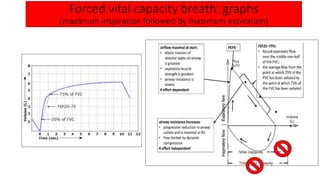
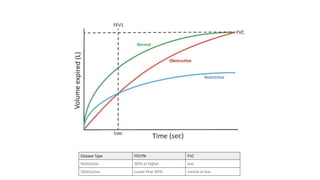
Pulmonary function tests (PFTs) evaluate lung function through non-invasive tests. PFTs can be done at bedside or in traditional labs and include tests of lung volumes, capacities, flows and gas exchange. Bedside PFTs include breath-holding tests to assess vital capacity, single-breath tests for functional residual capacity, cough tests for strength, blowing tests for maximum breathing capacity, and peak flow tests. PFTs help diagnose and monitor pulmonary diseases, assess disease severity and surgical risk, and track response to treatment. Common diseases detected include obstructive disorders like asthma which limit expiration and restrictive disorders like fibrosis which limit both expiration and inspiration.