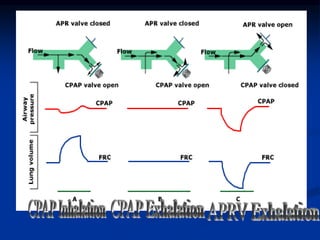
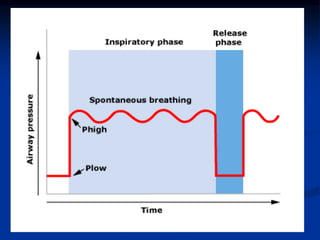
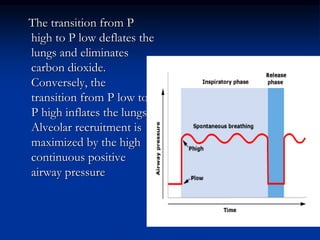
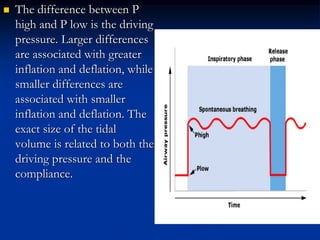
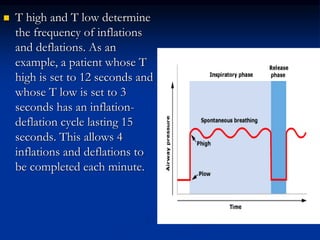
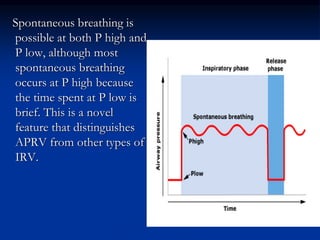
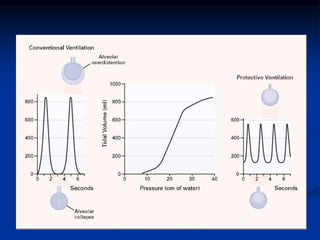
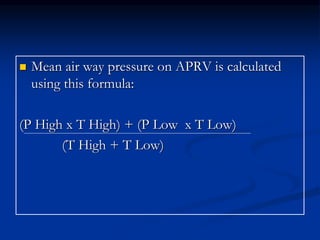
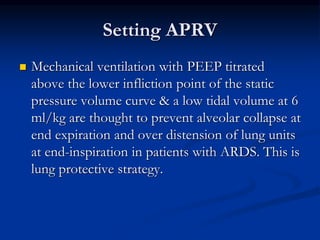
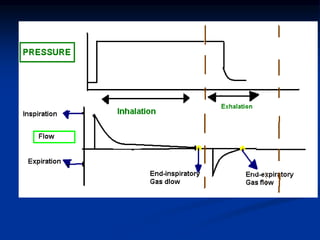
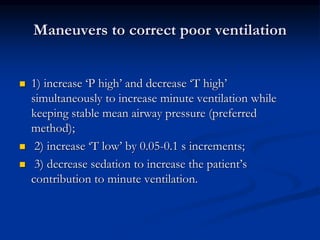
APRV (Airway Pressure Release Ventilation) is a ventilation mode that applies continuous positive airway pressure (CPAP) for a prolonged high-pressure phase (T high) to recruit and maintain lung volume. It then has a brief low-pressure release phase (T low) where most ventilation and CO2 removal occurs. Compared to conventional ventilation, APRV may cause less ventilator-induced lung injury due to maintaining higher end-expiratory lung volumes without repetitive opening/closing of alveoli. It also allows for spontaneous breathing which improves patient comfort and outcomes. While APRV does not reduce mortality, it can improve other outcomes such as shorter ventilation times and ICU stays.