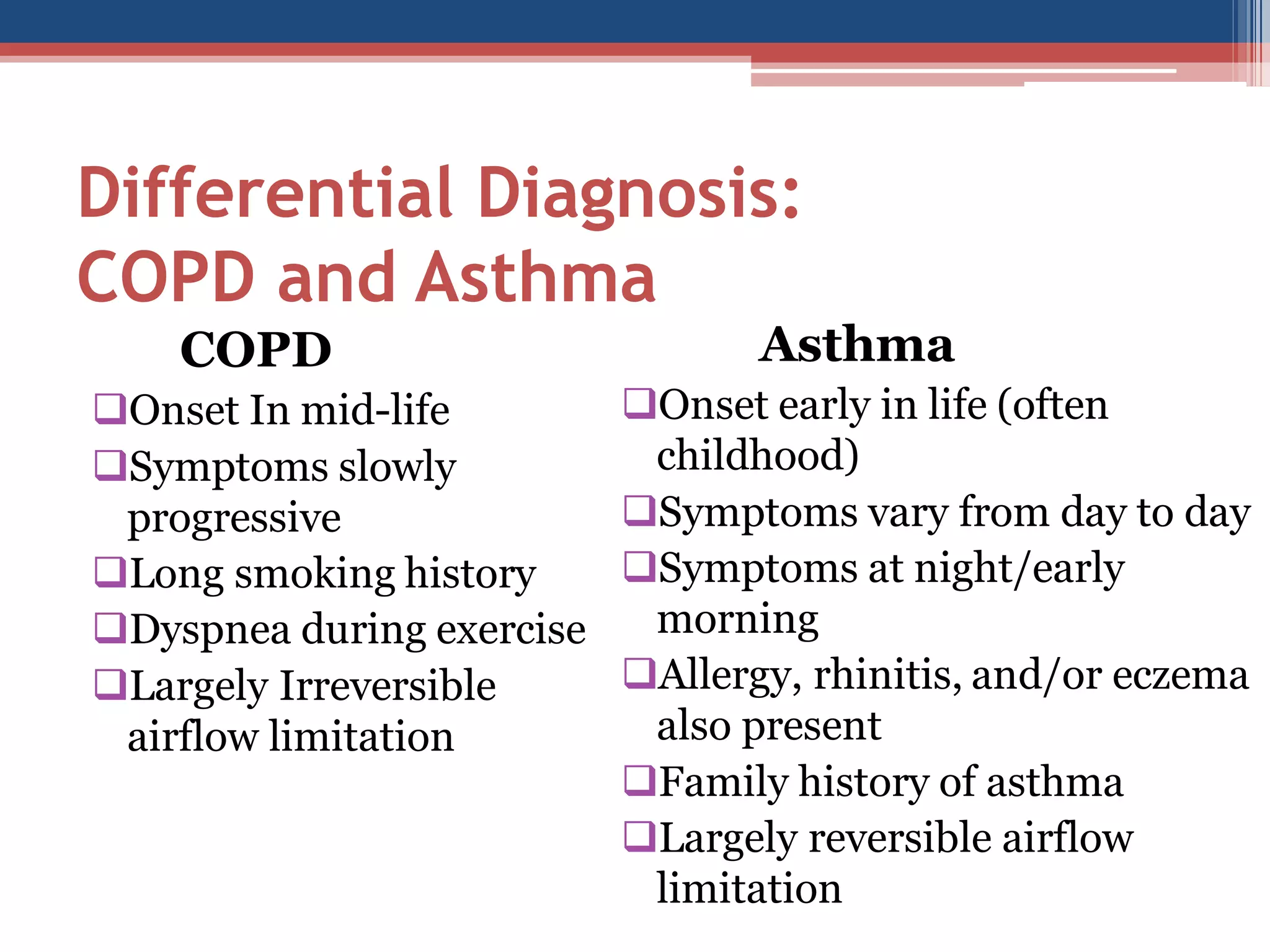
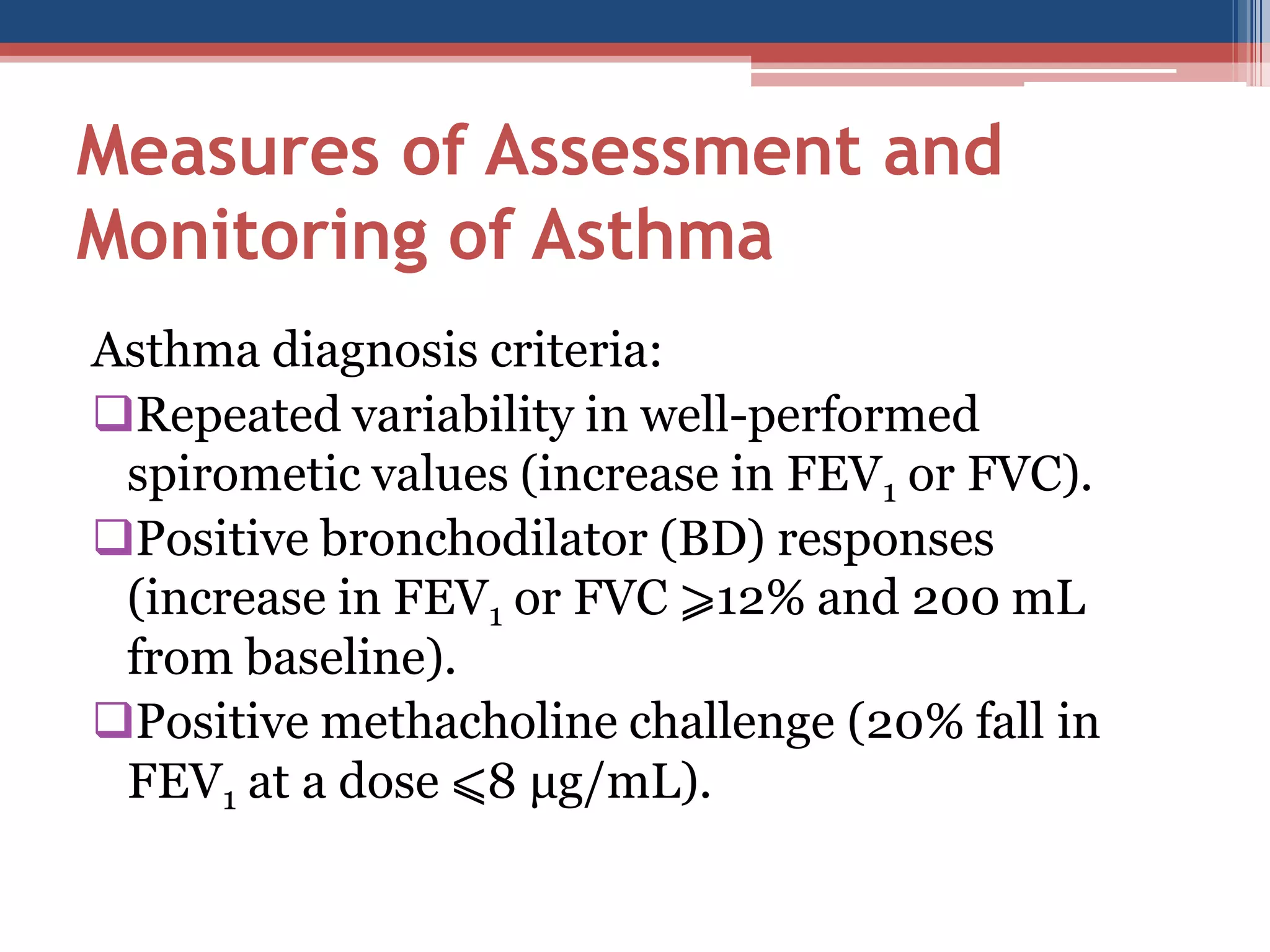
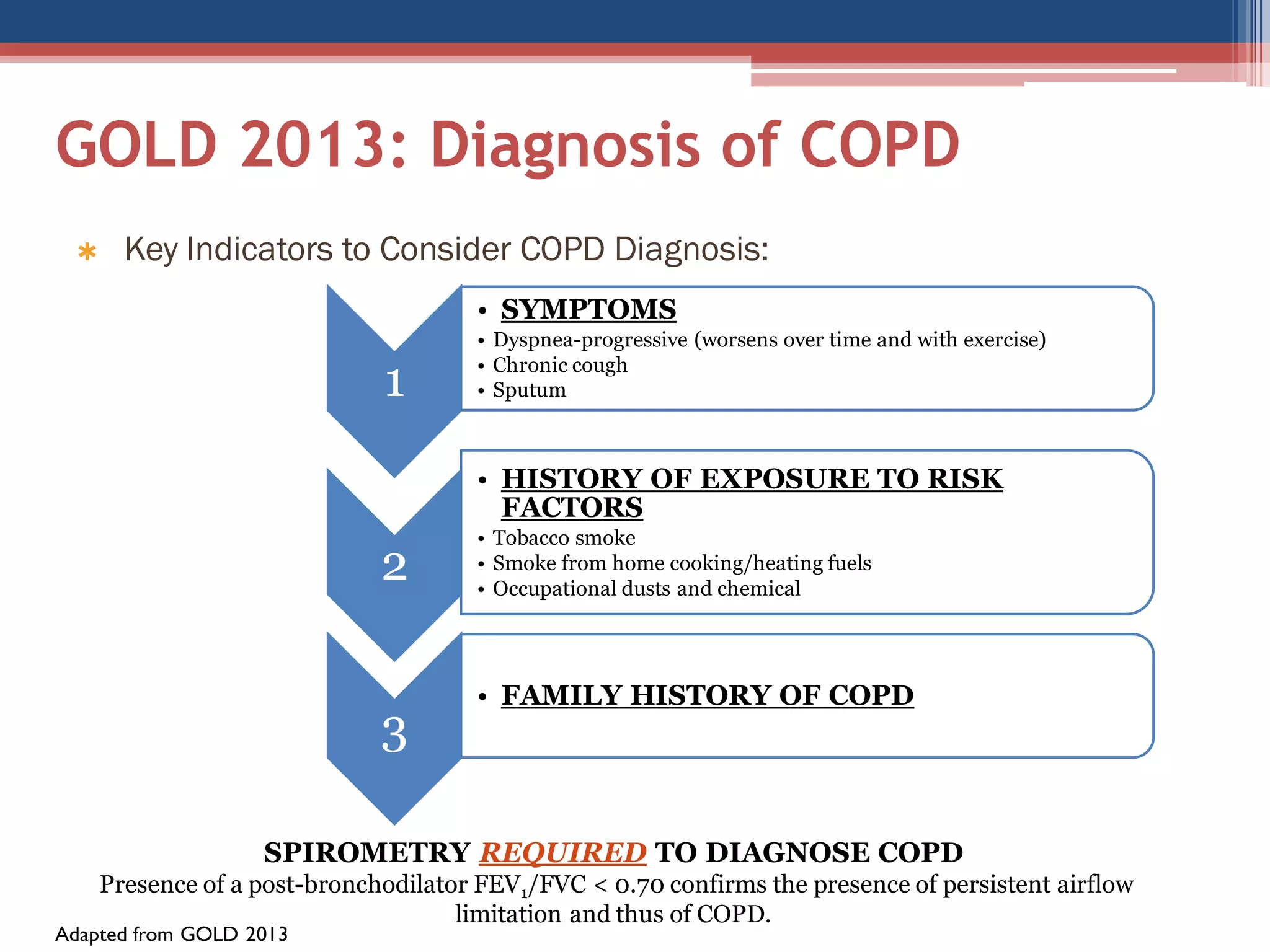
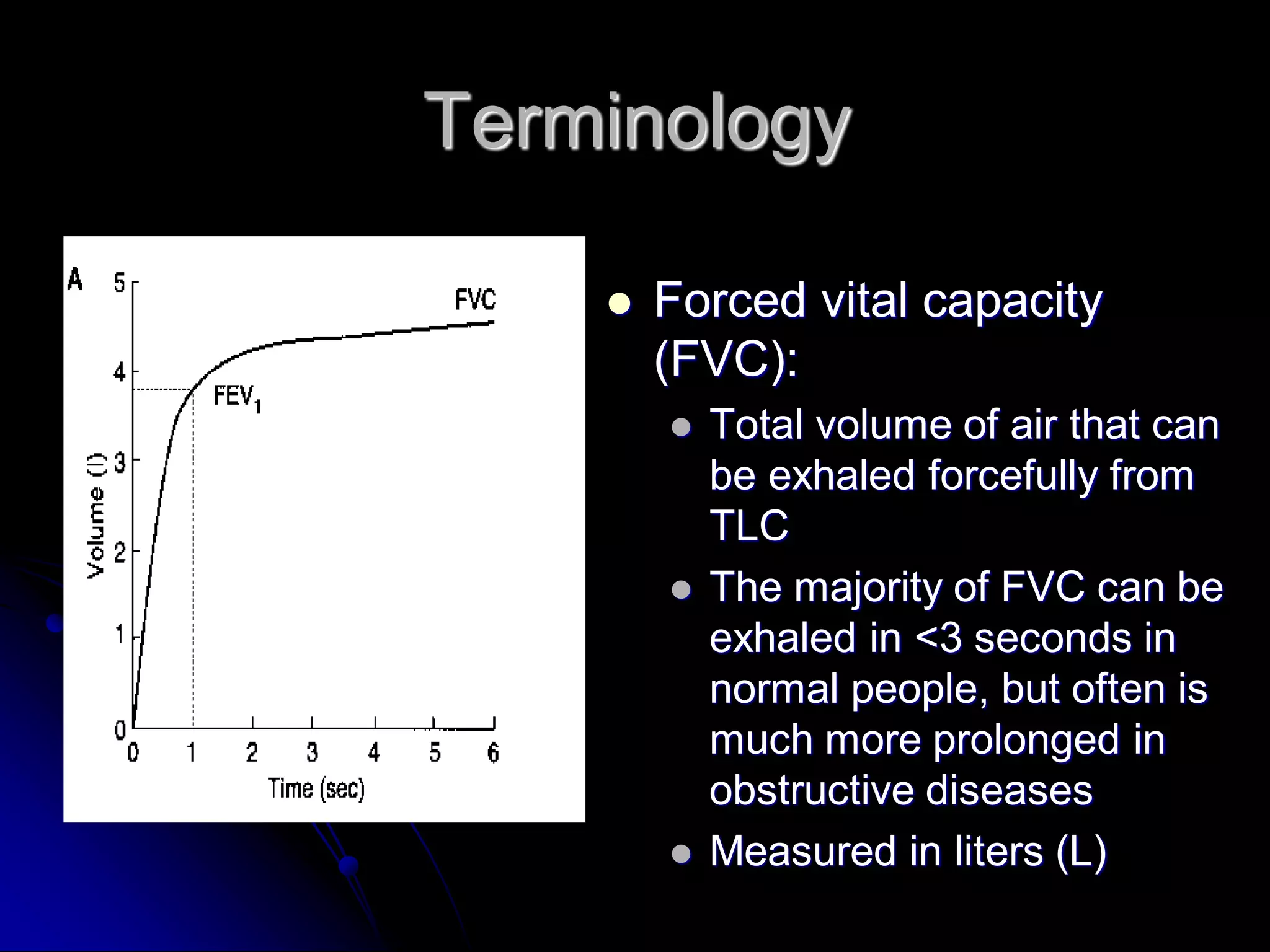
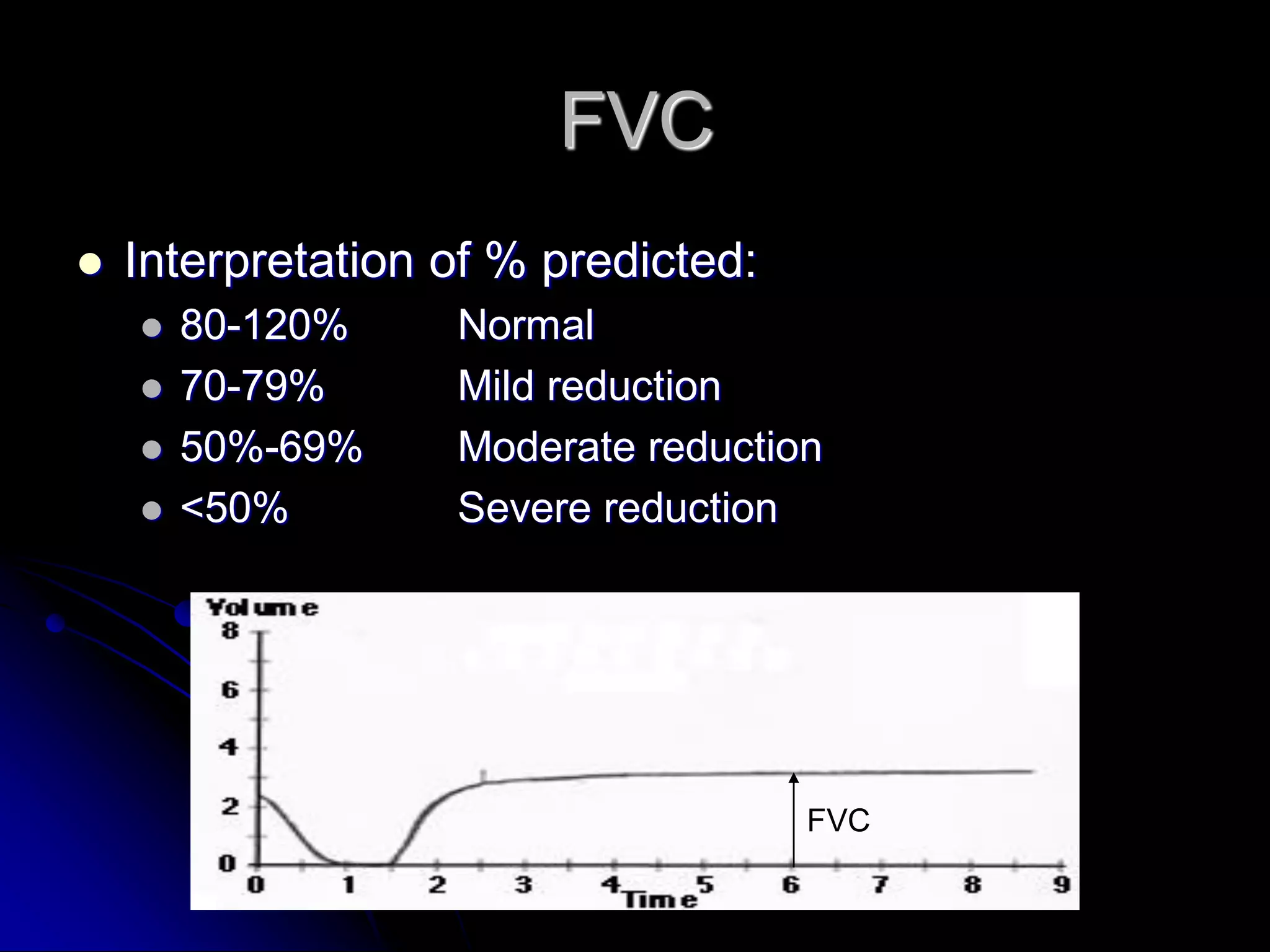
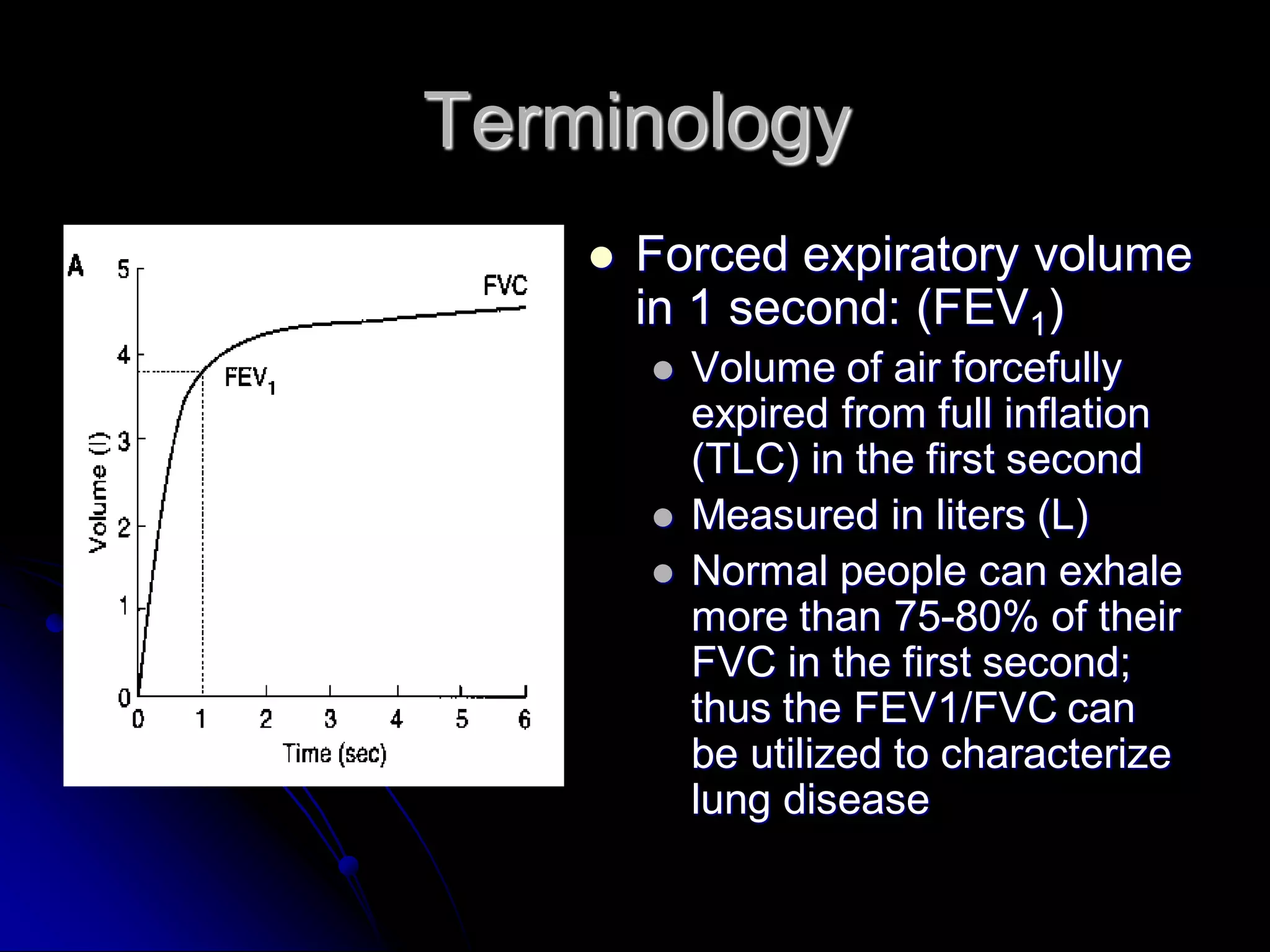
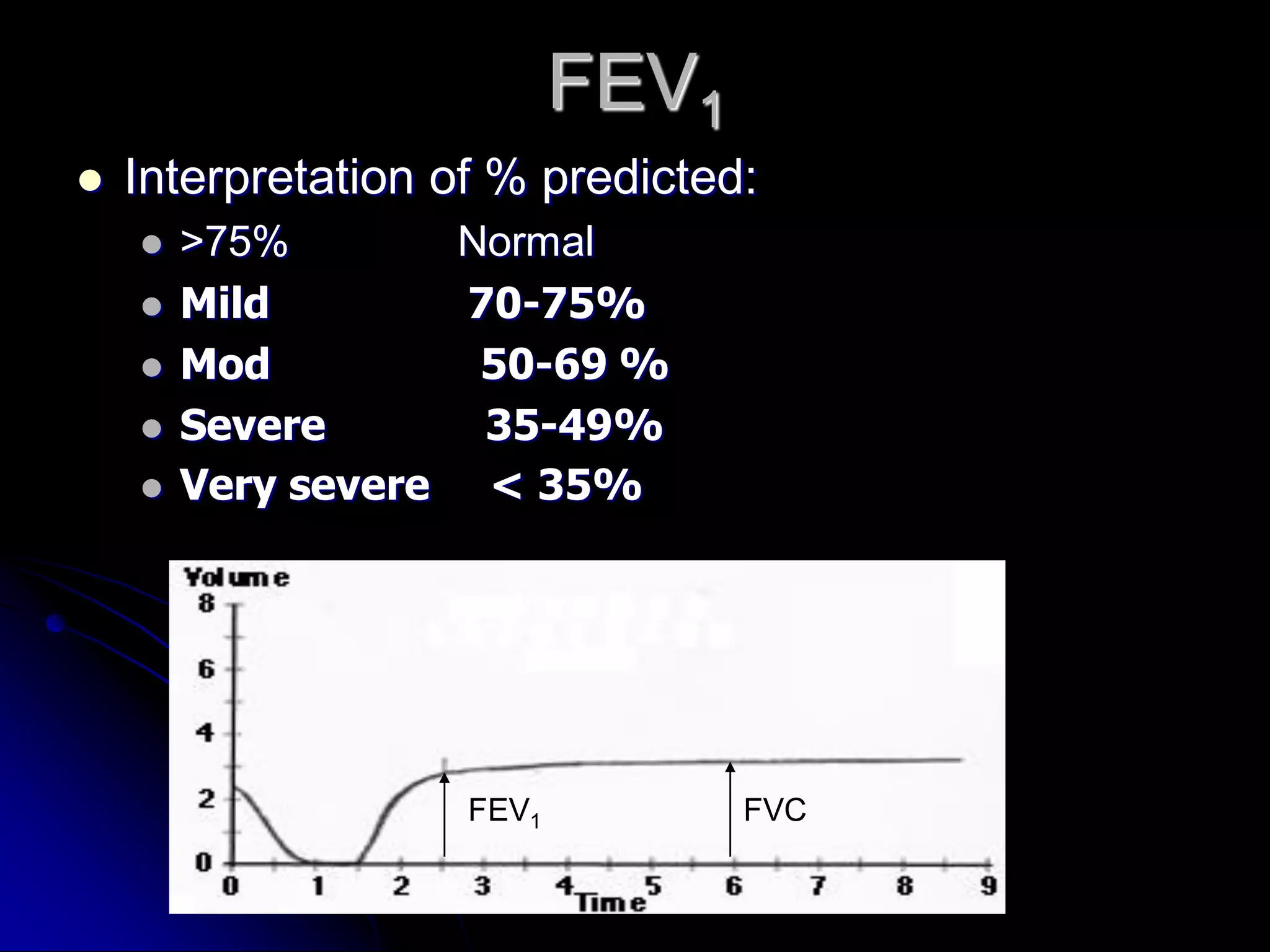
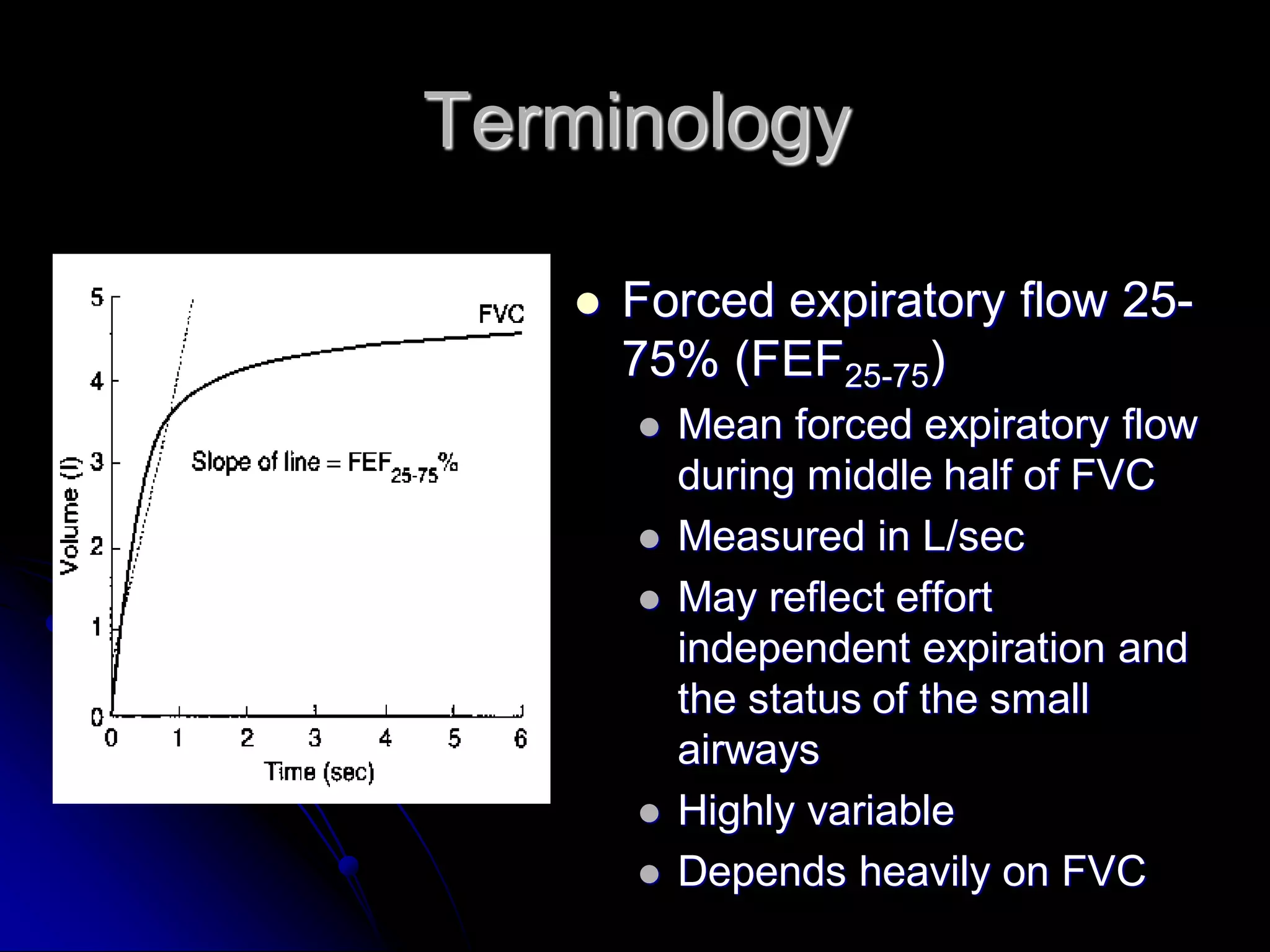
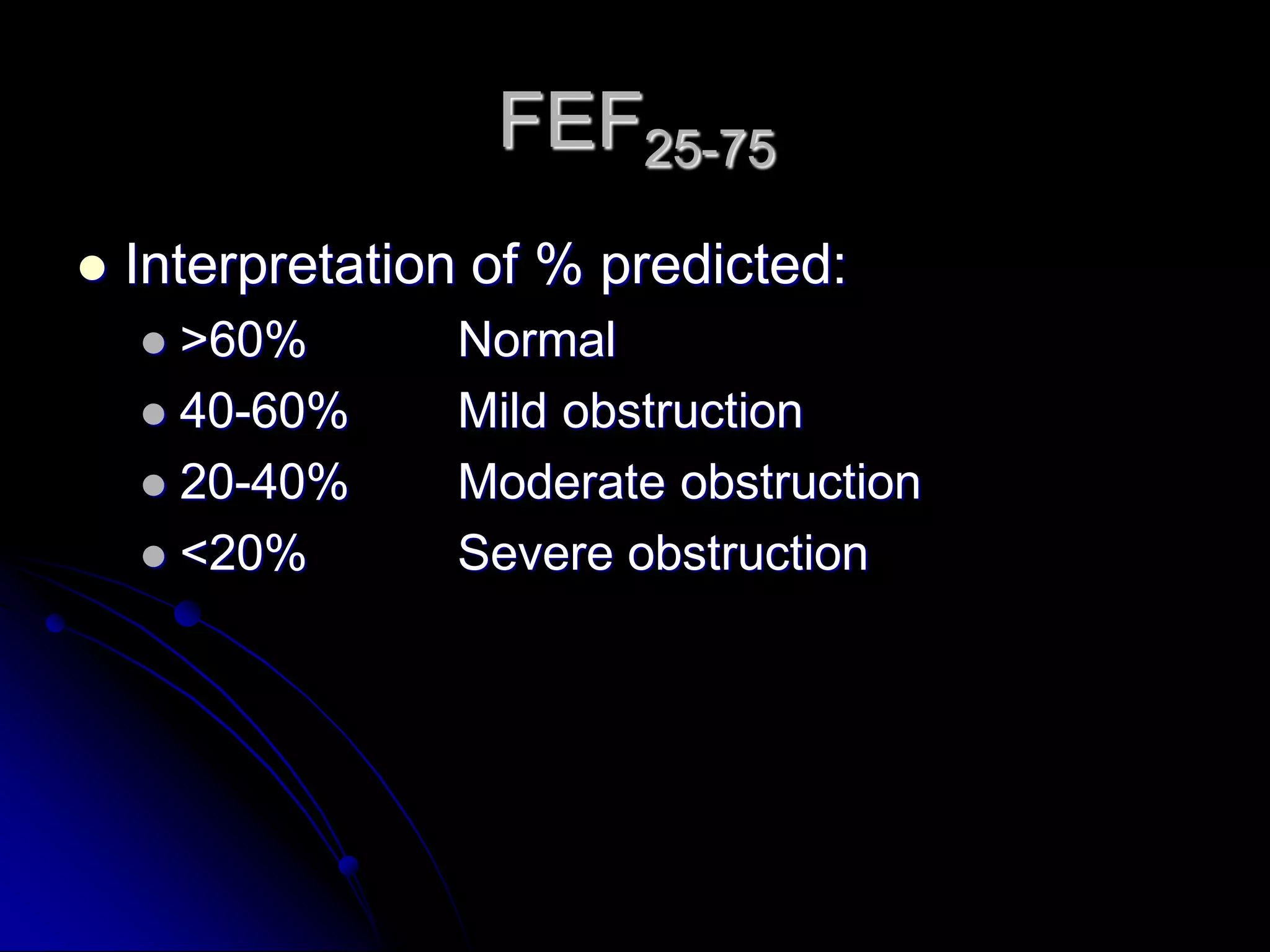
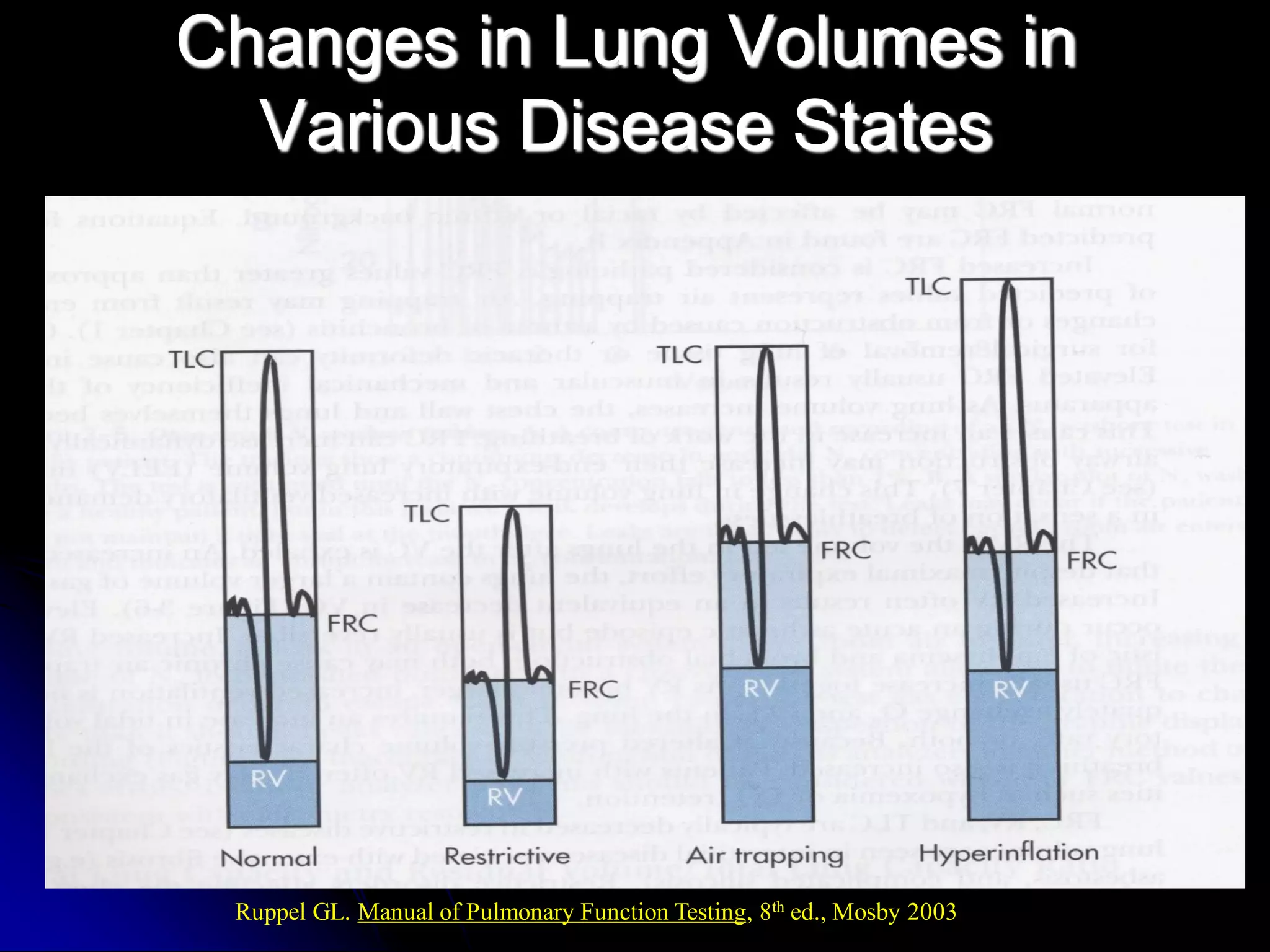
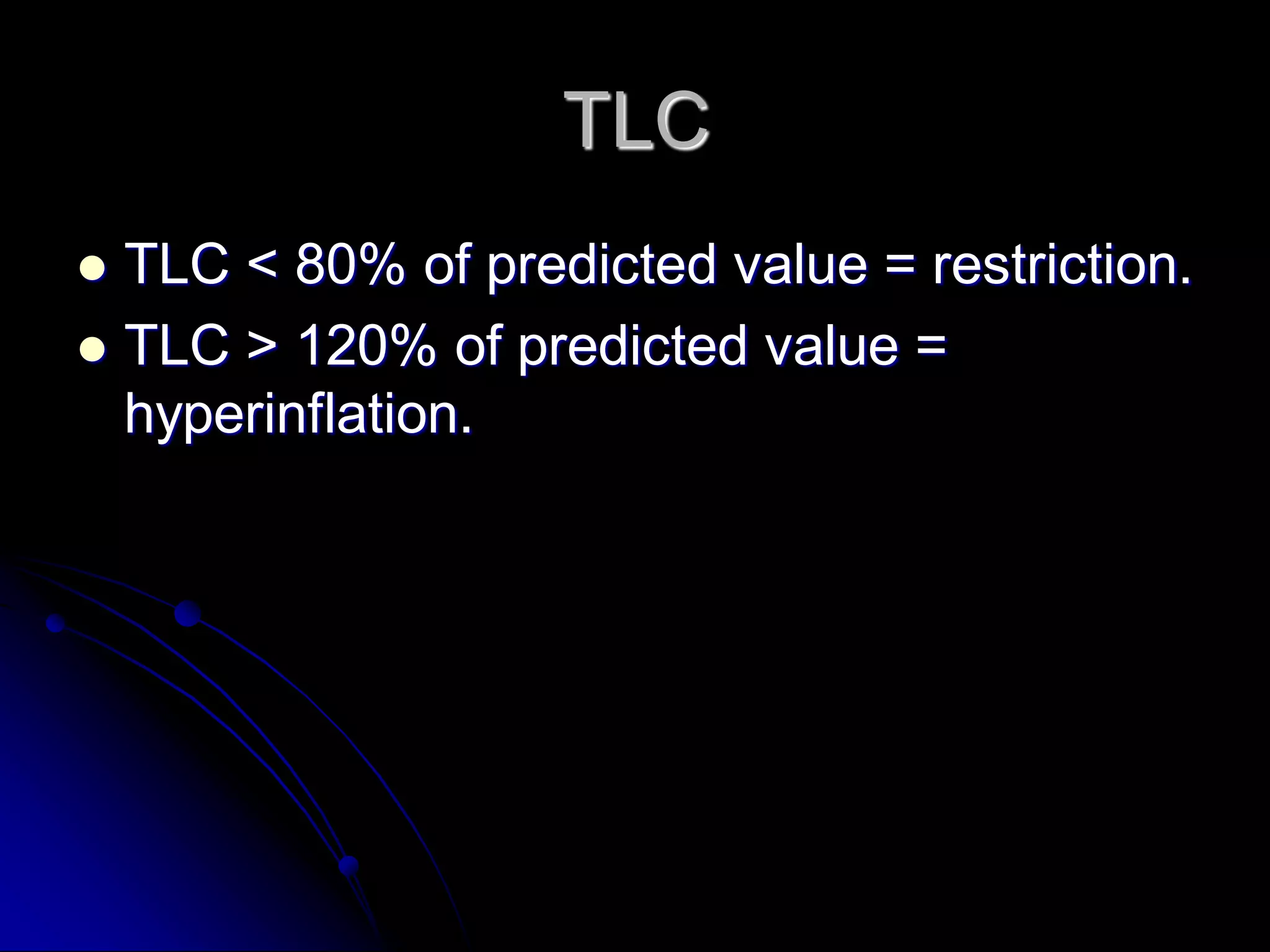
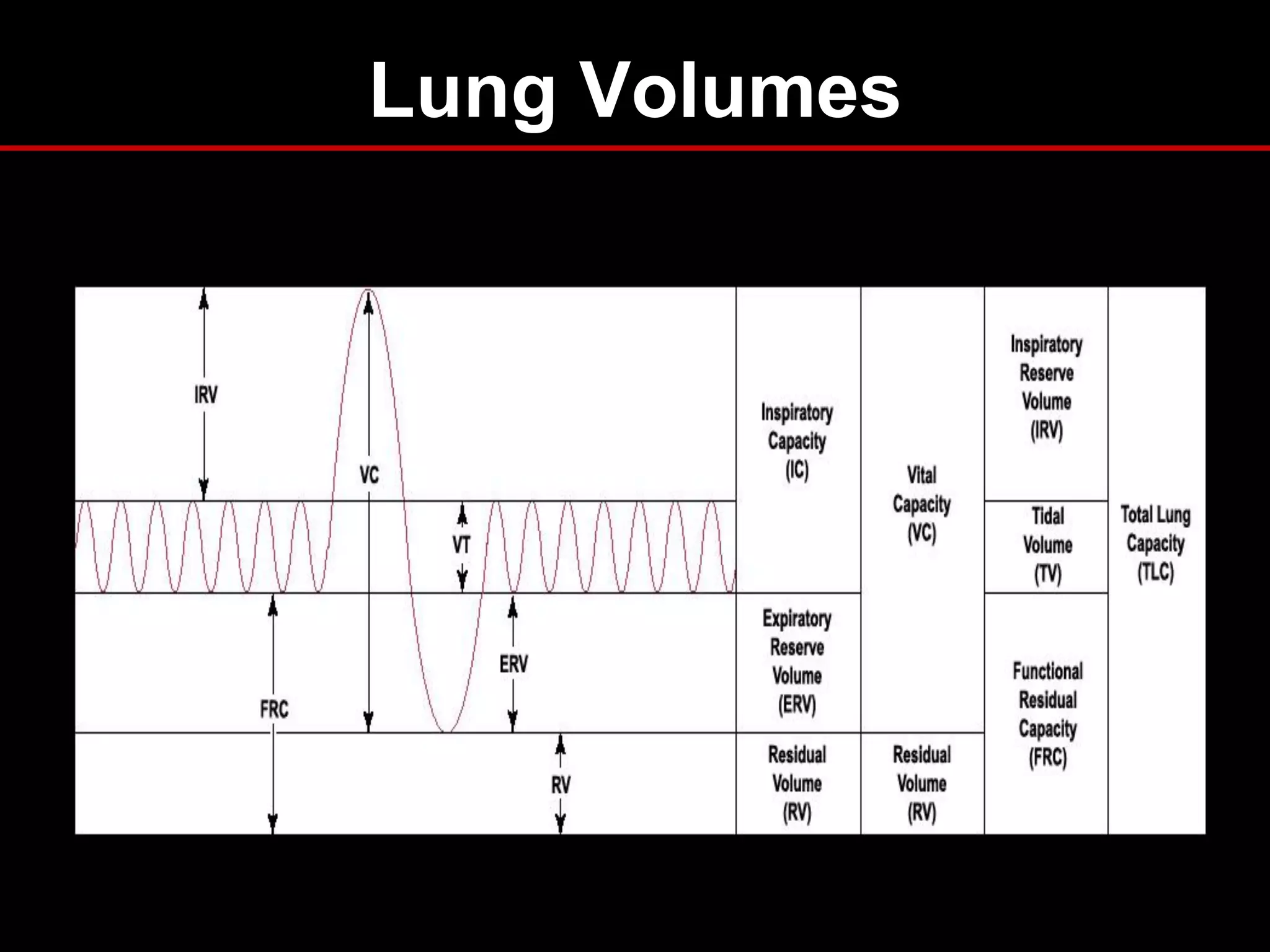
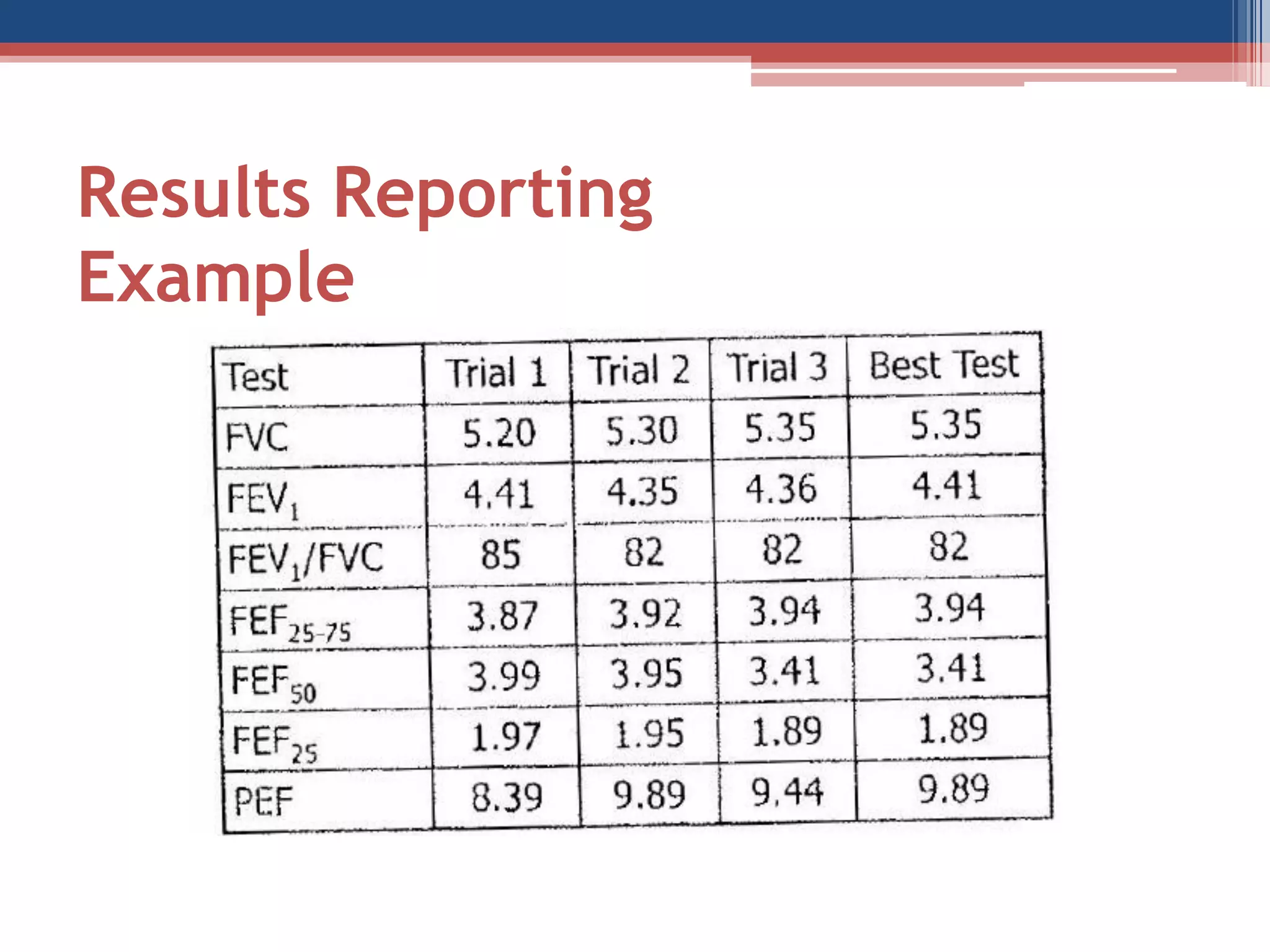
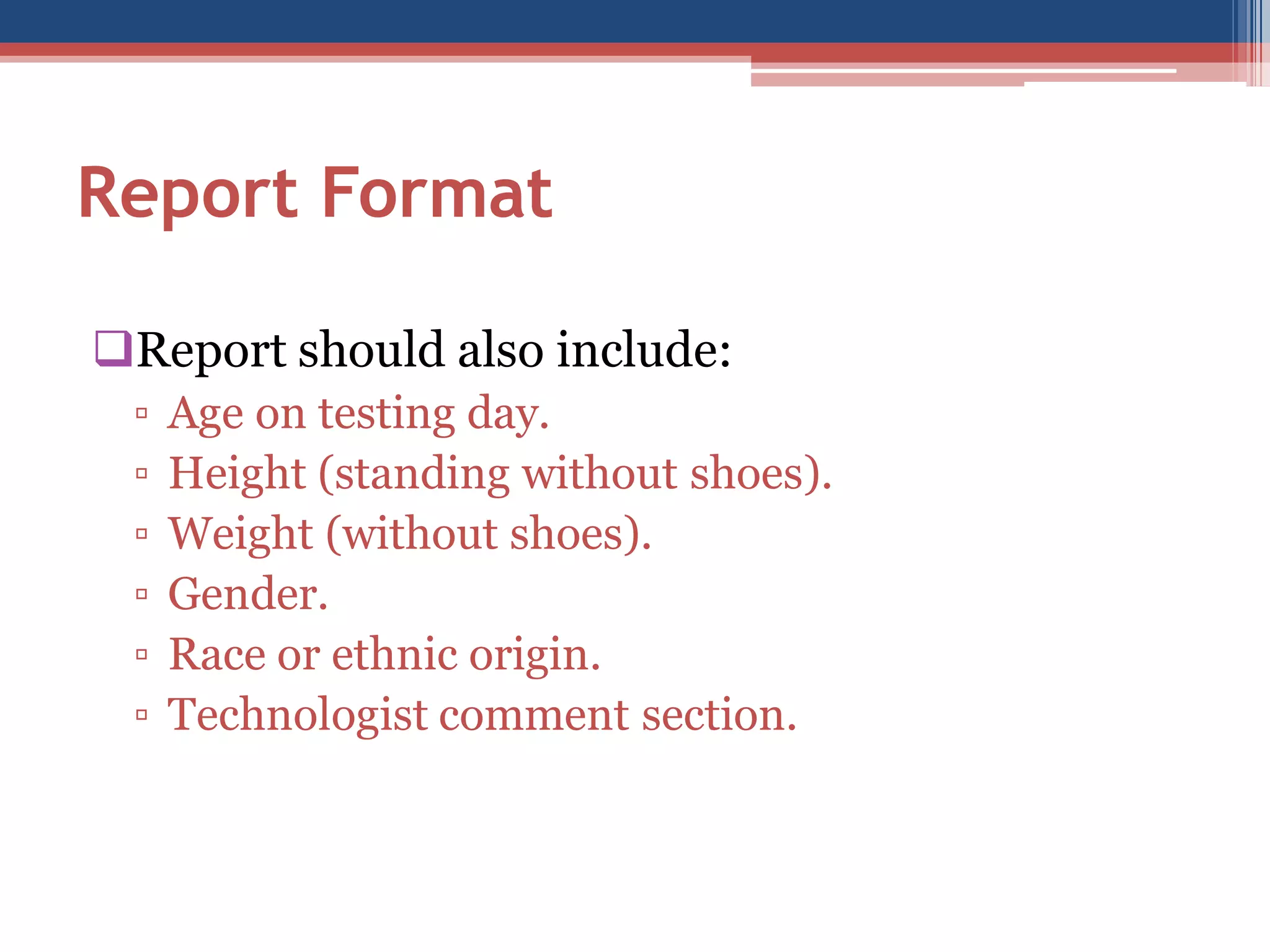
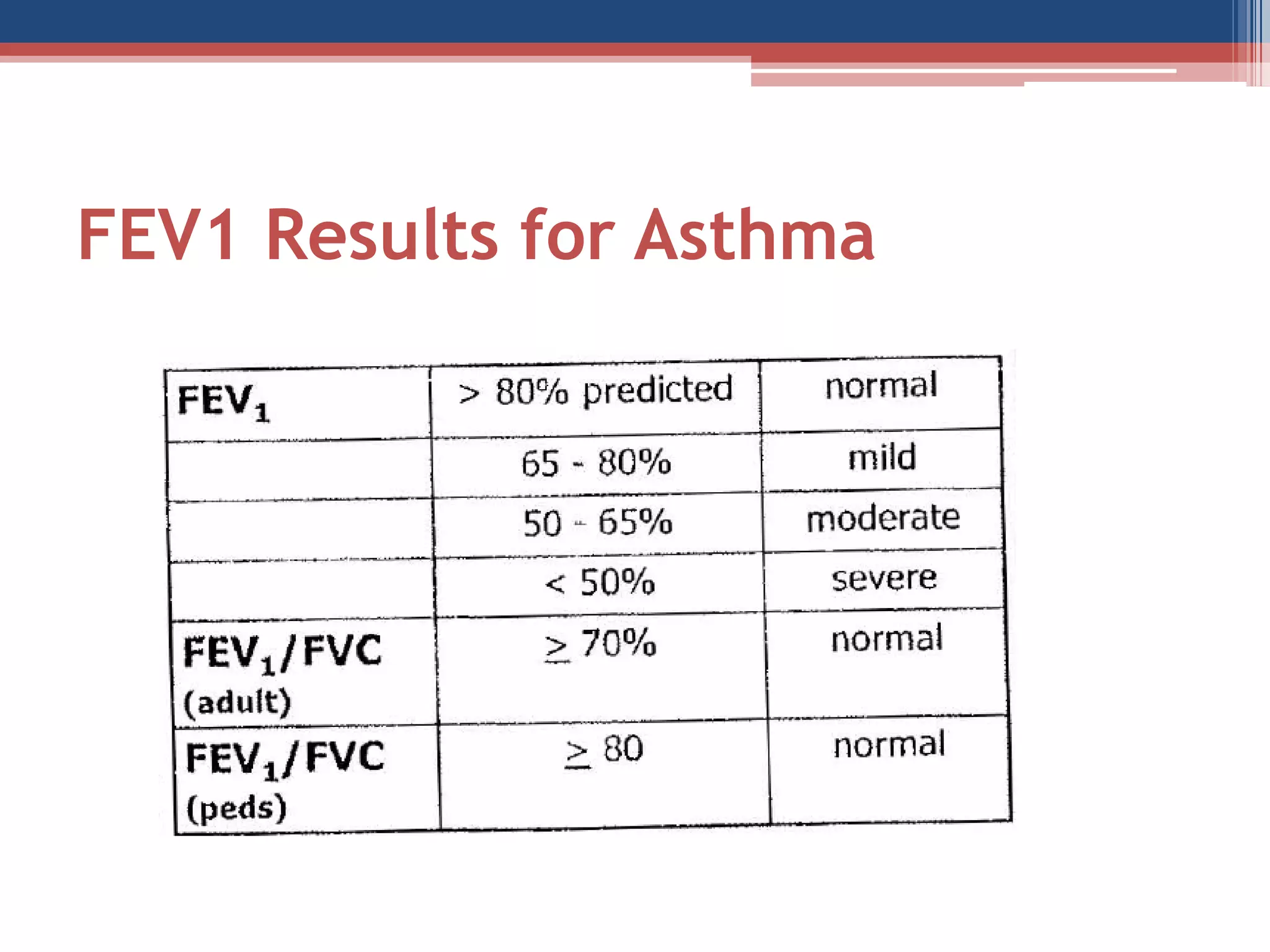
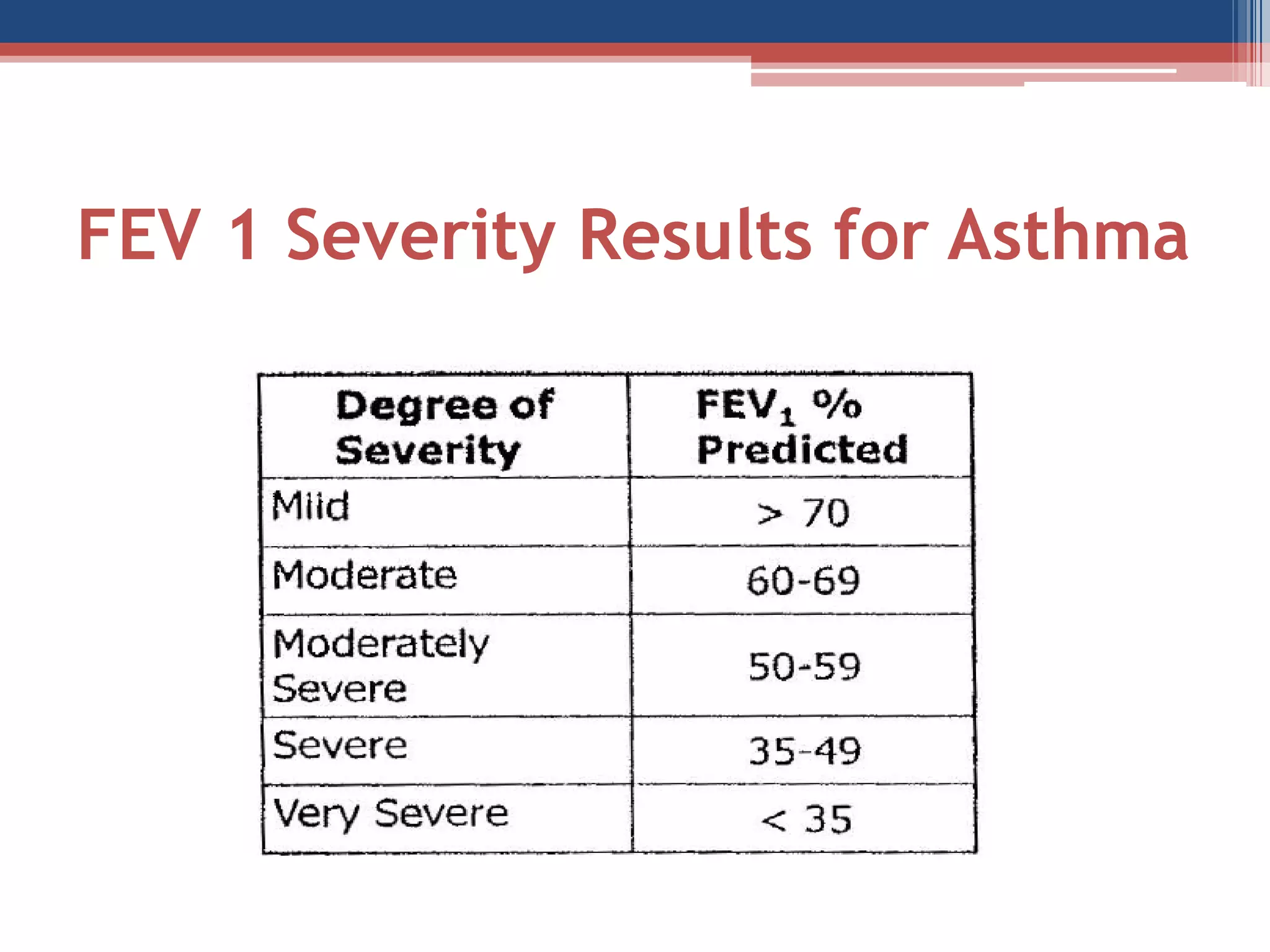
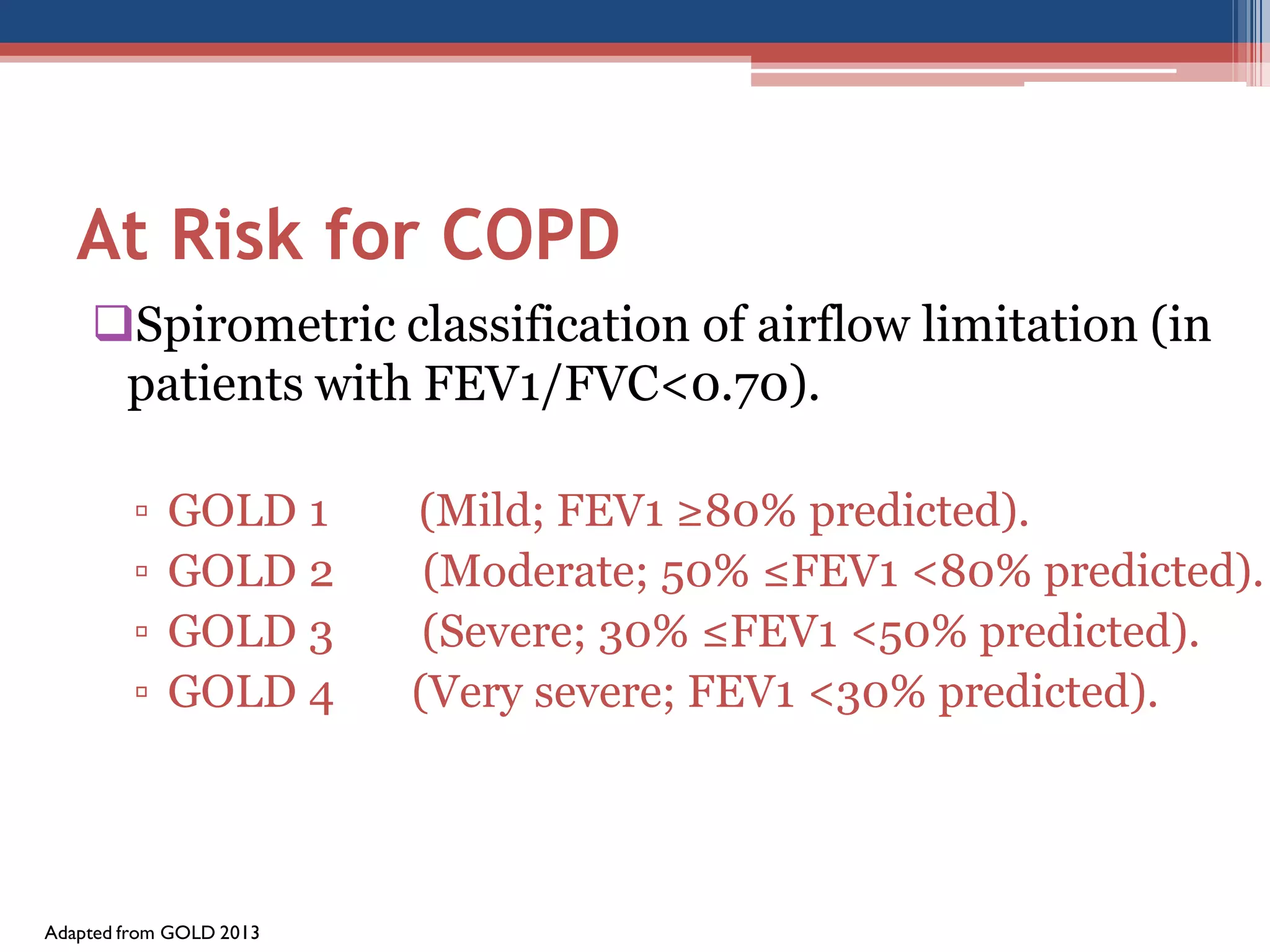
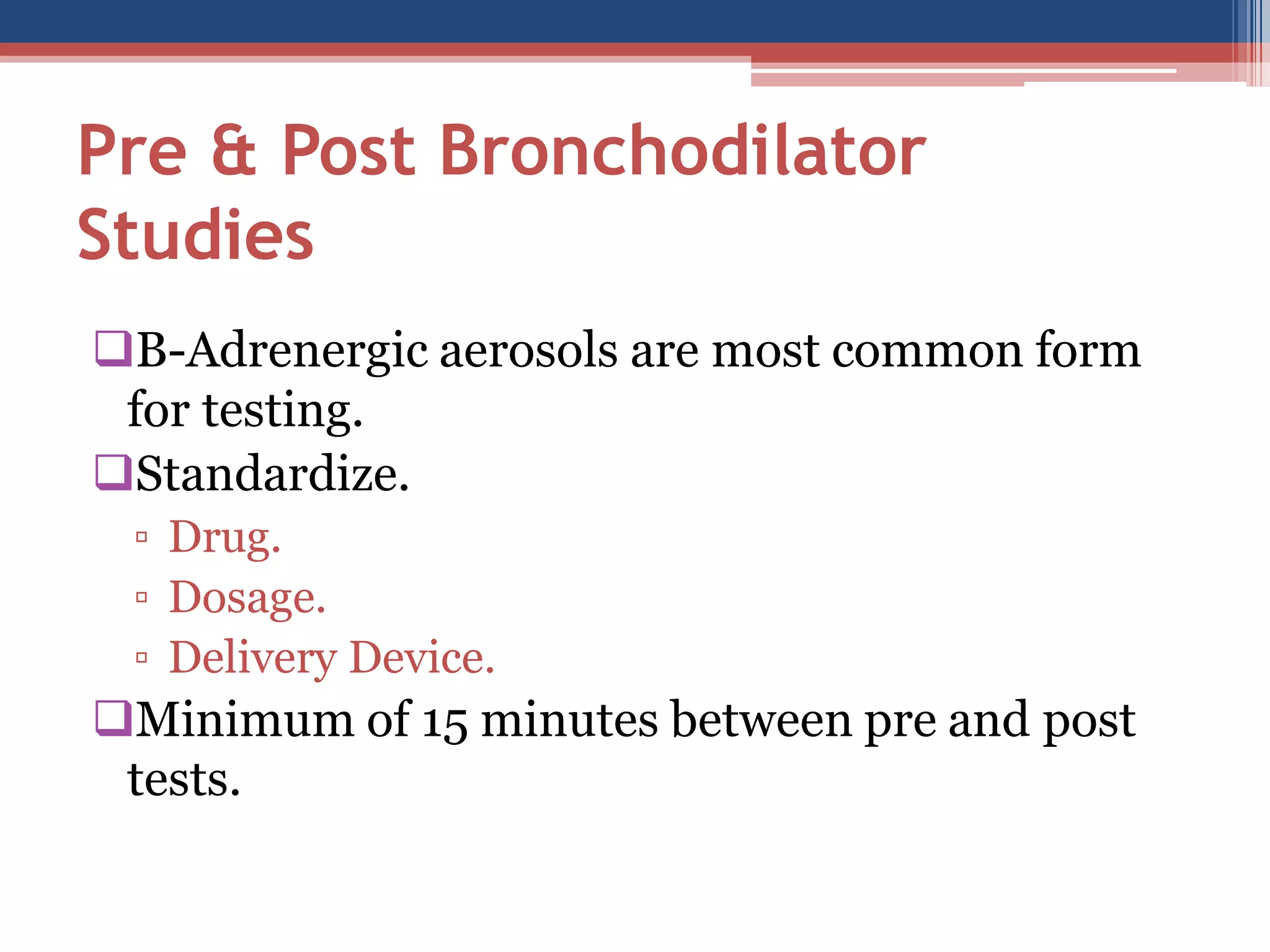
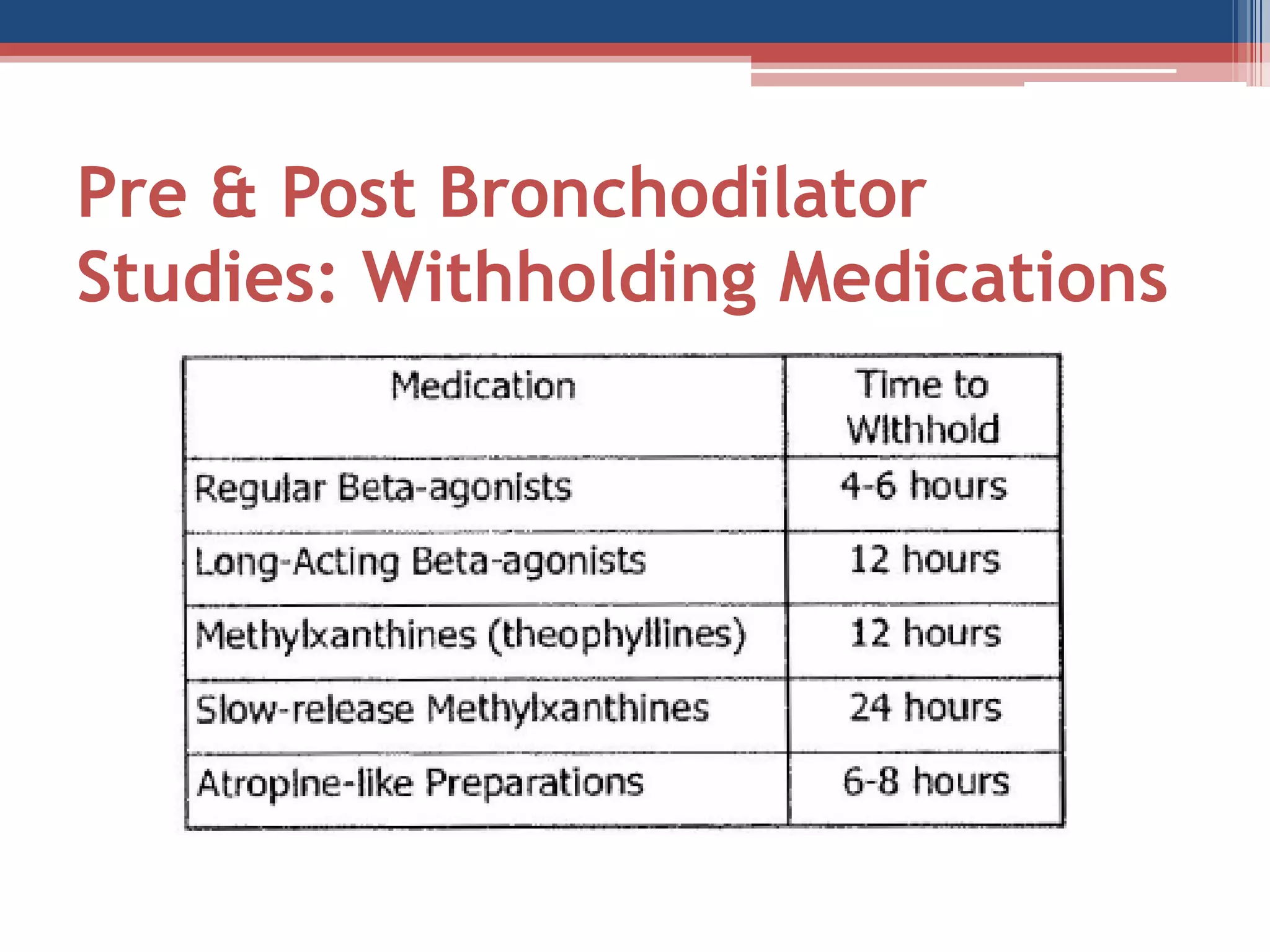
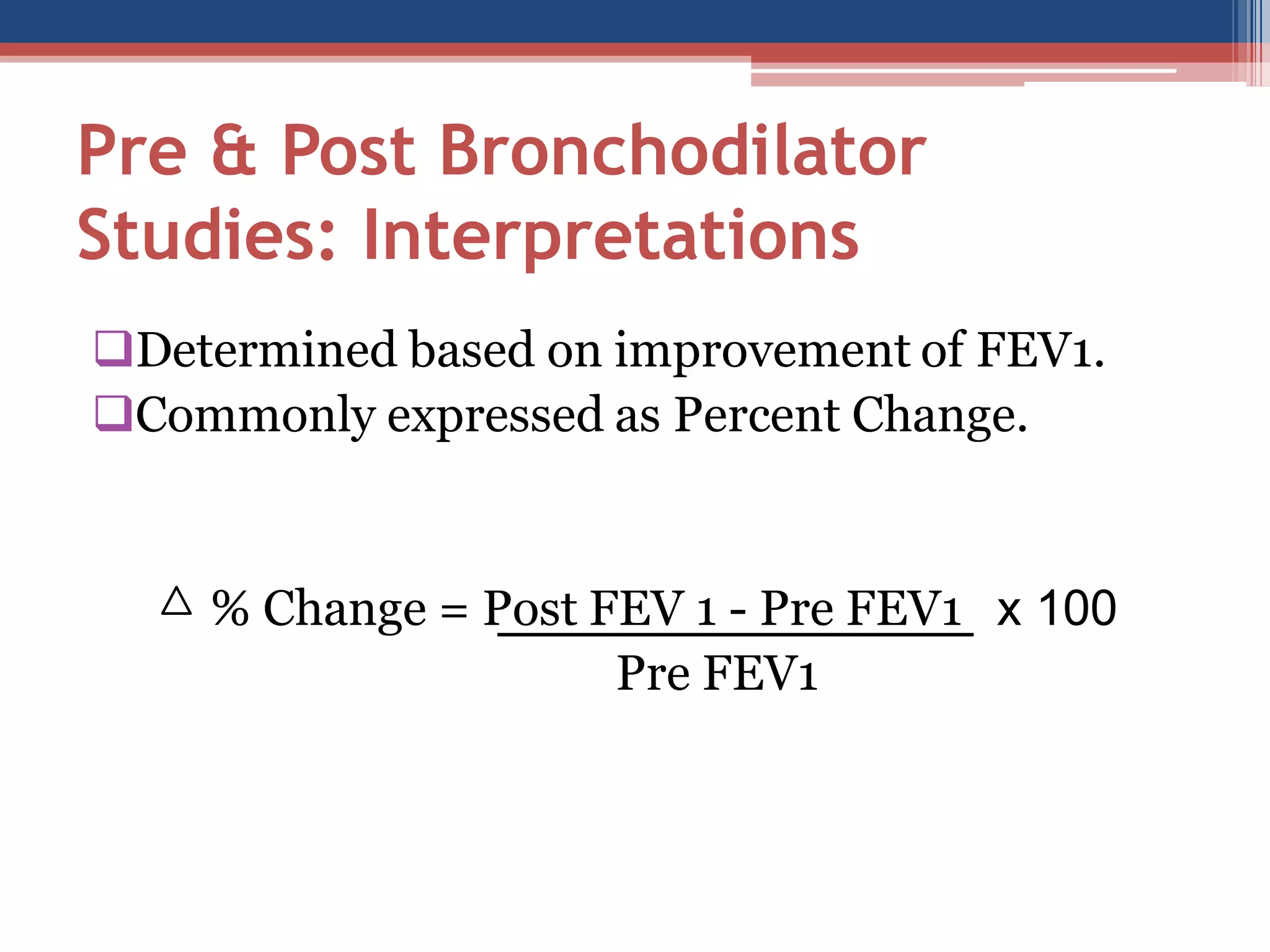
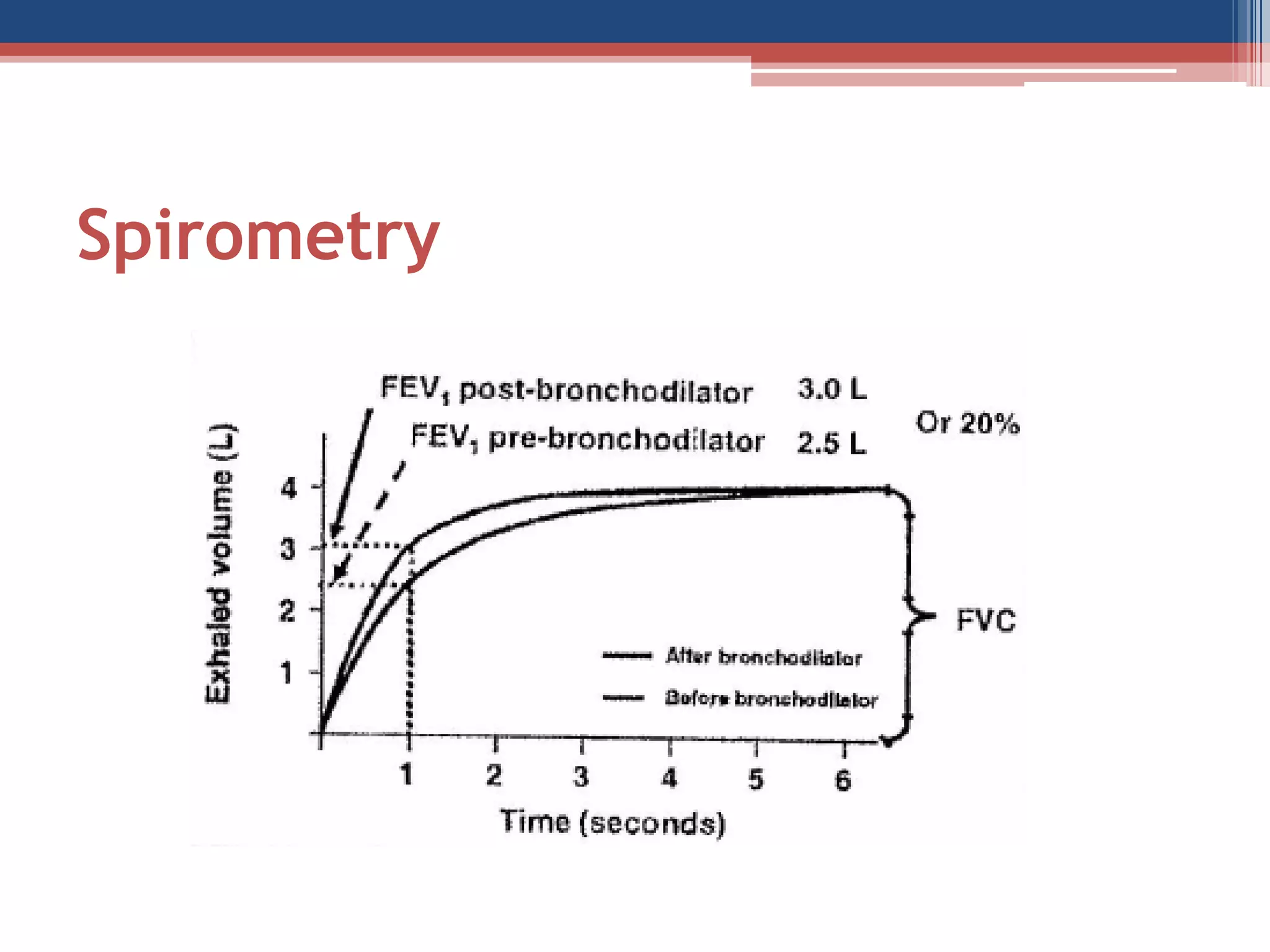
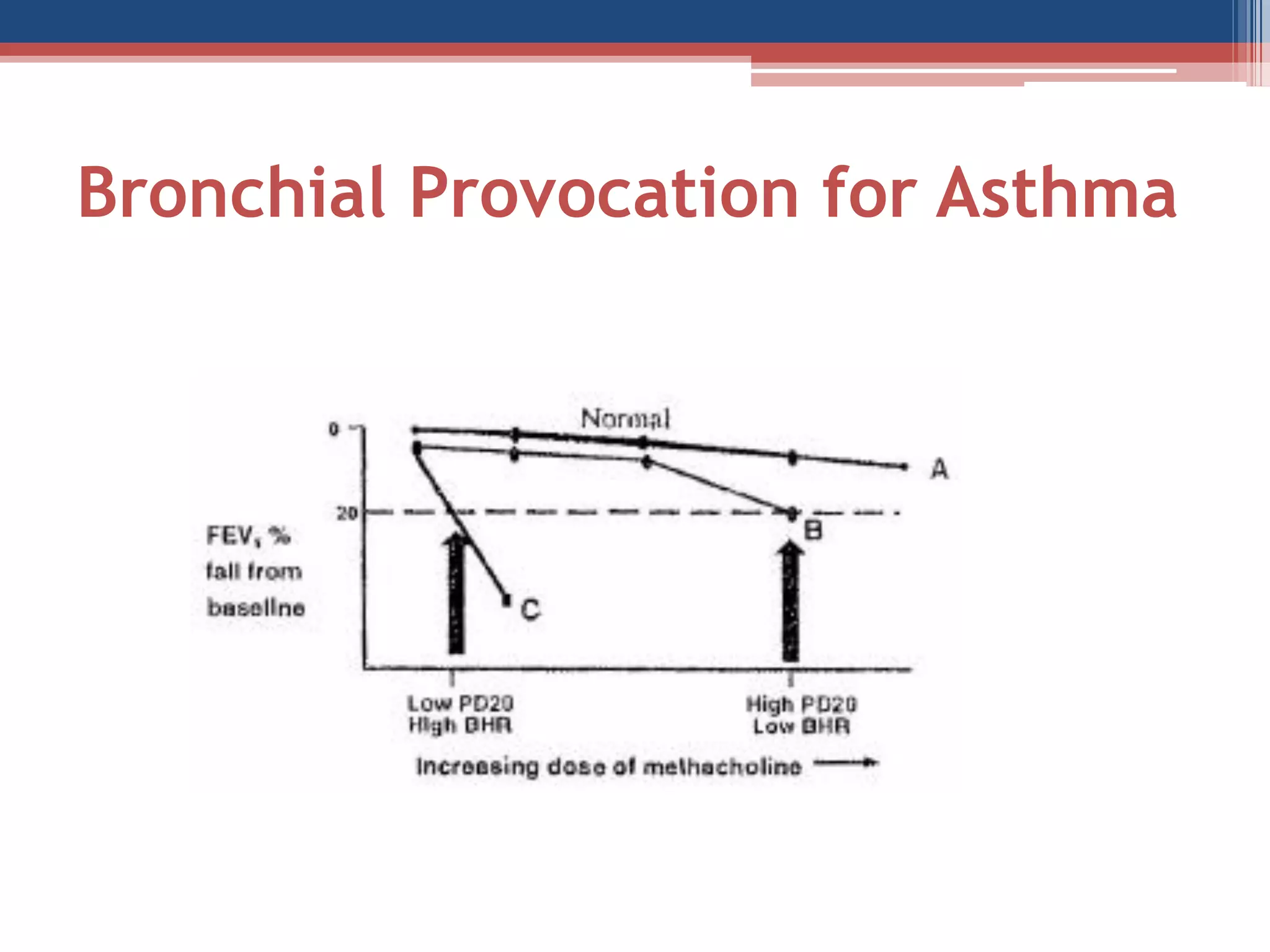
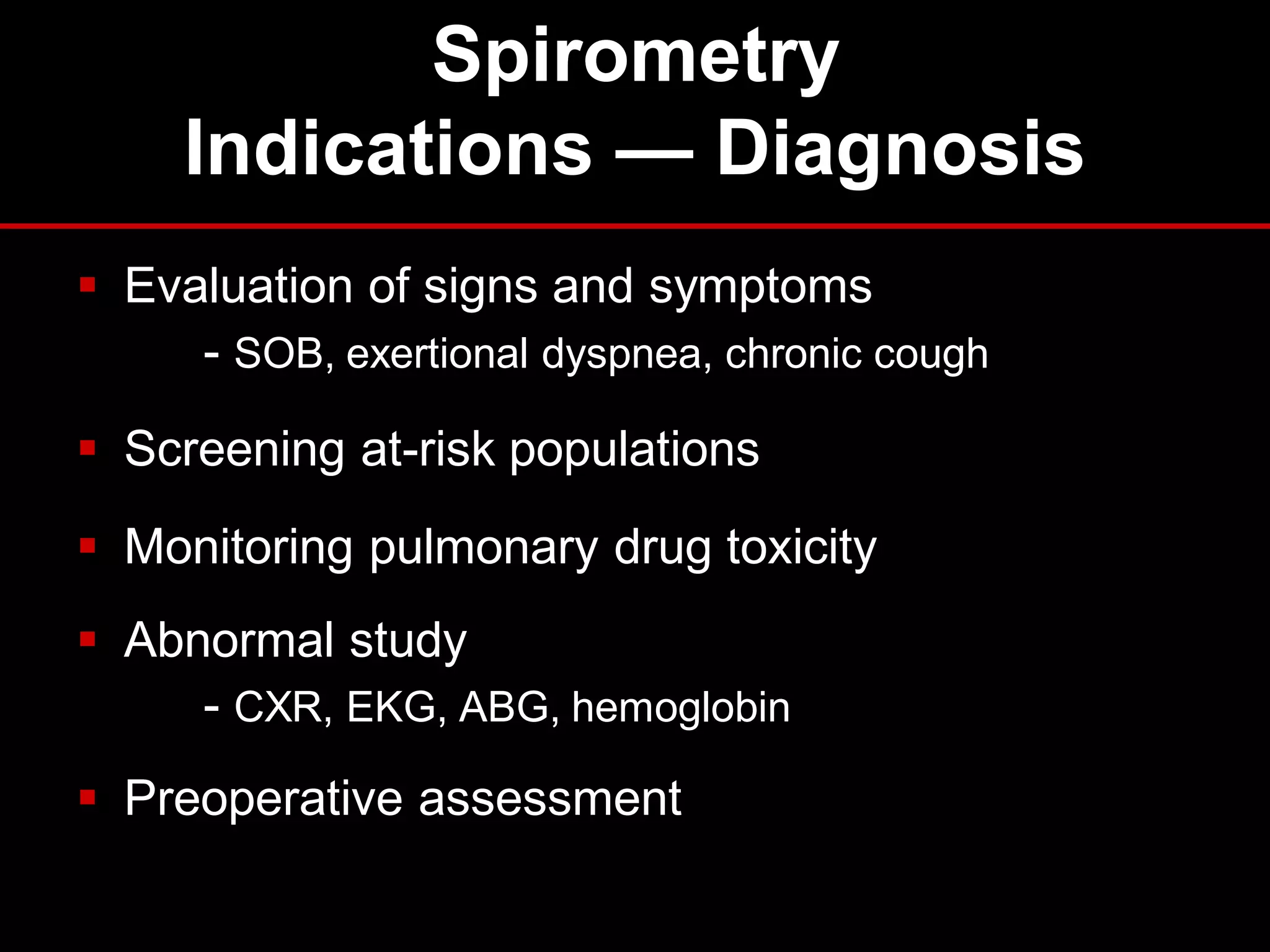
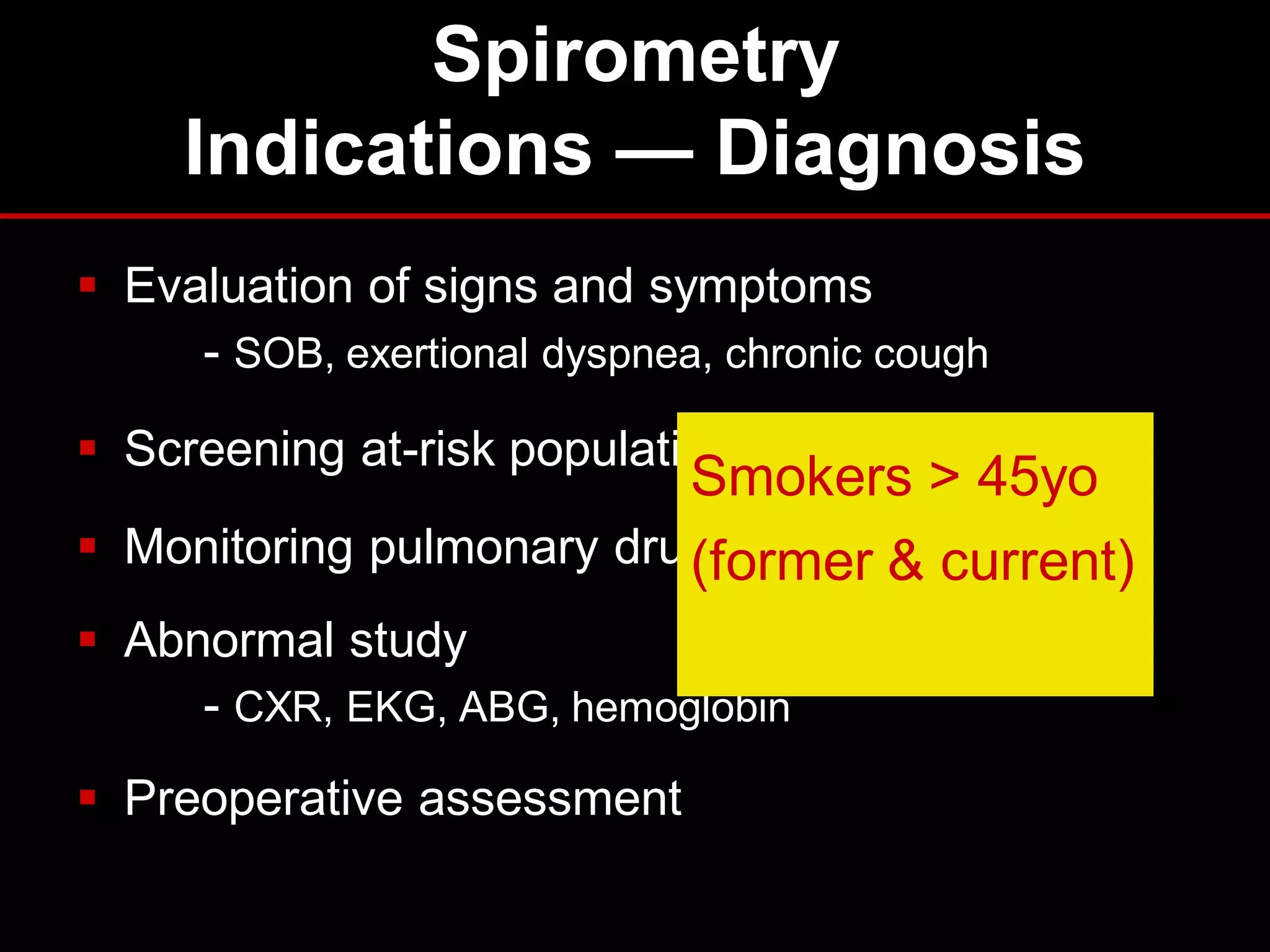
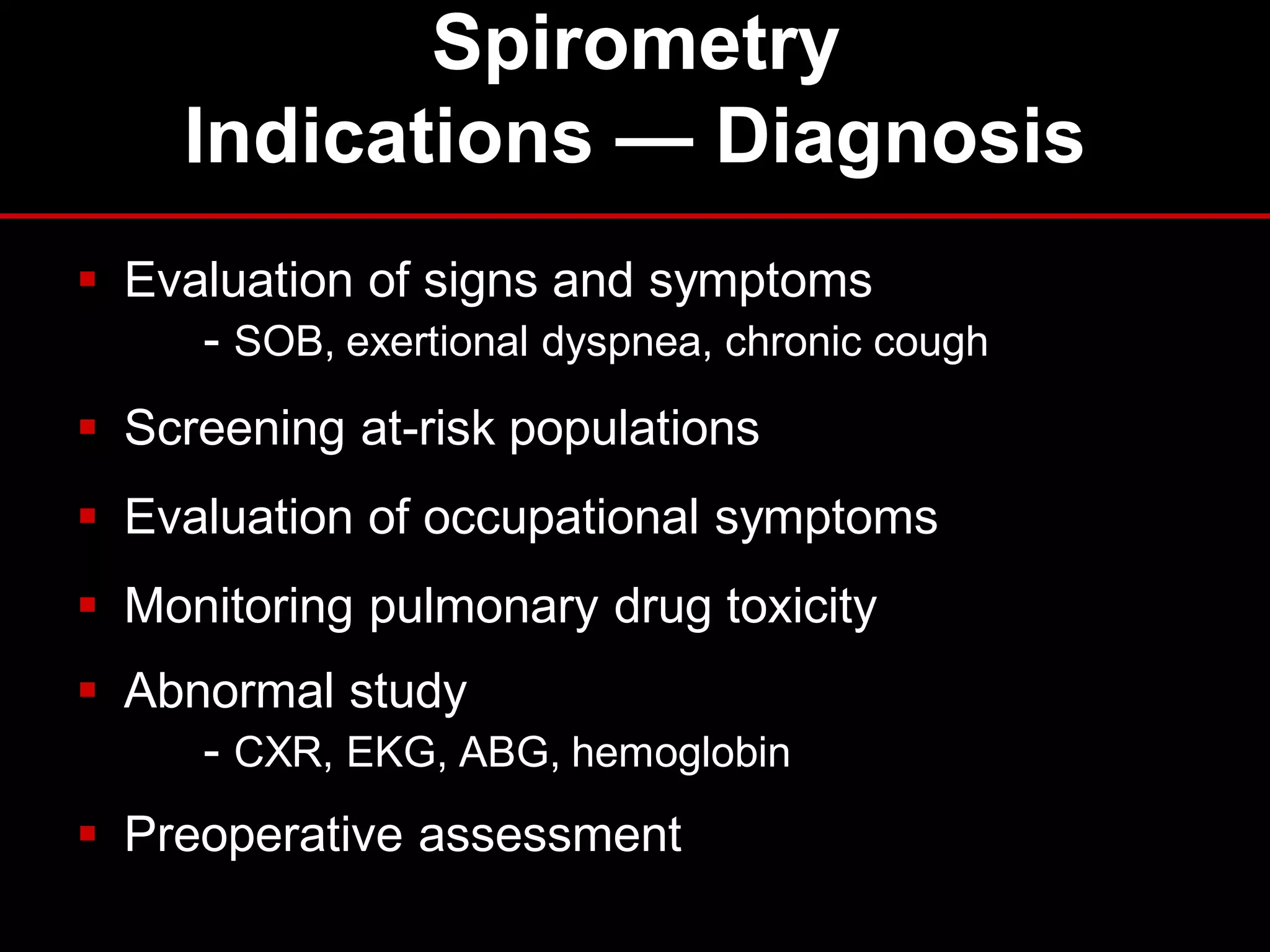
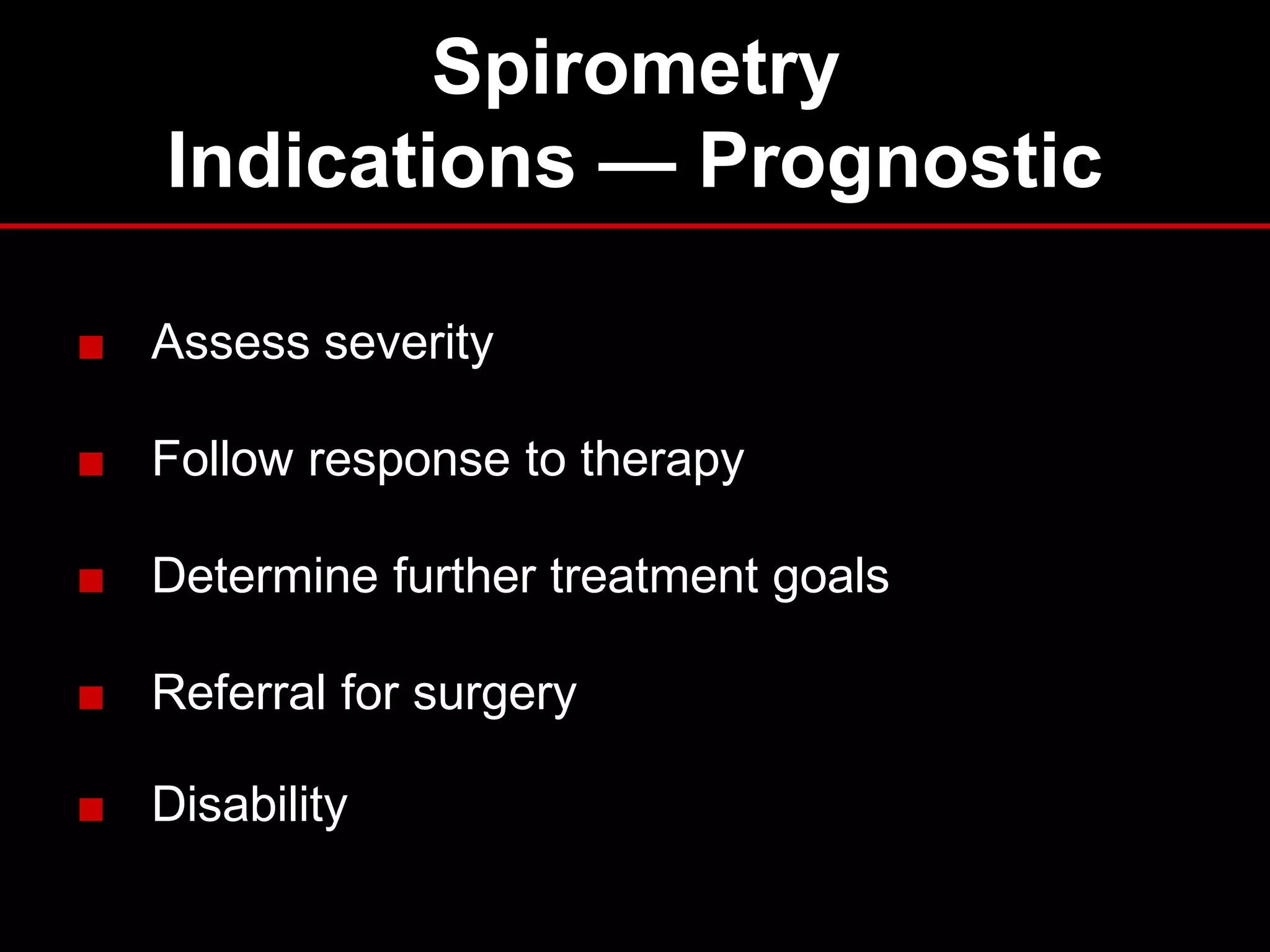
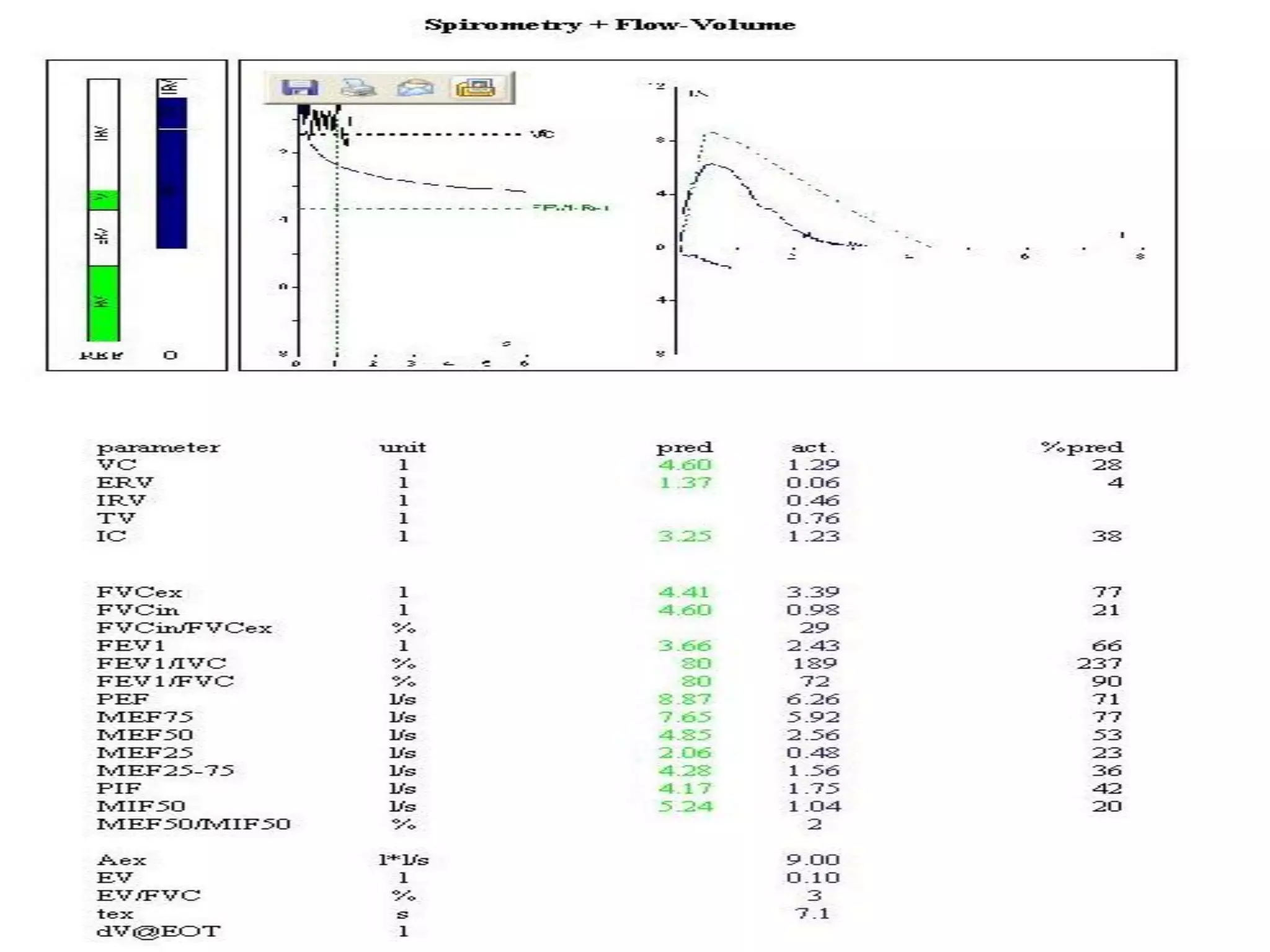
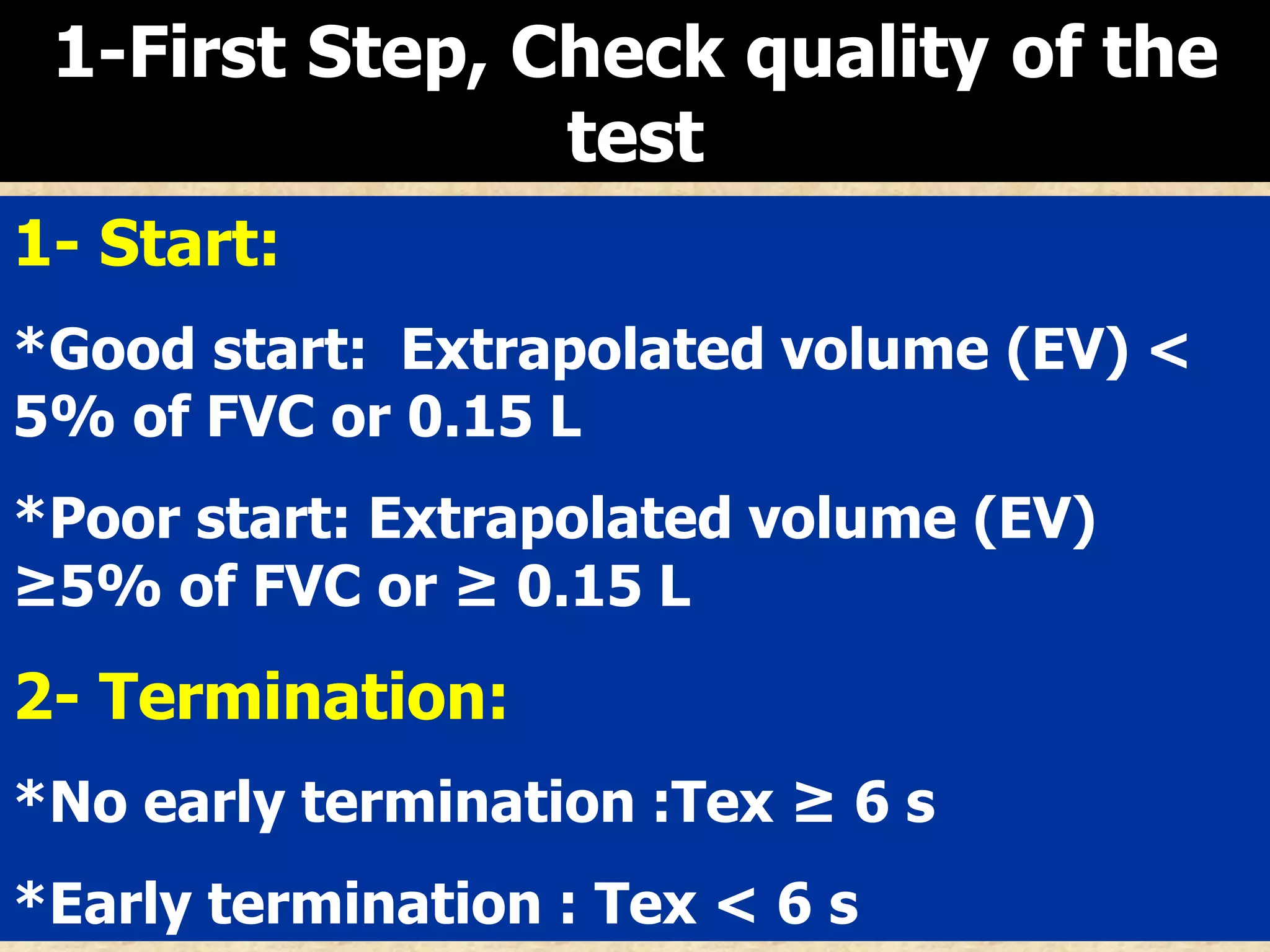
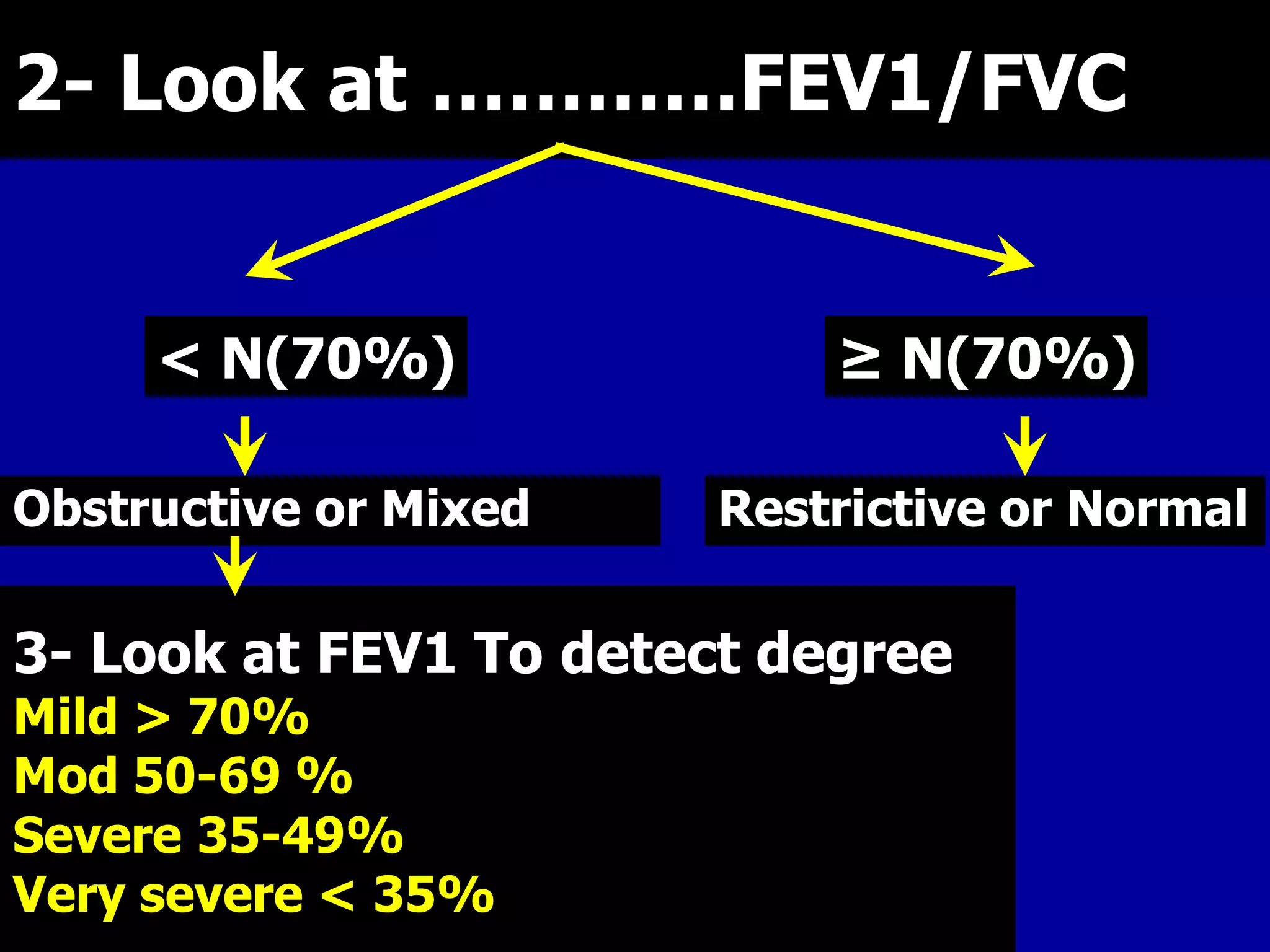
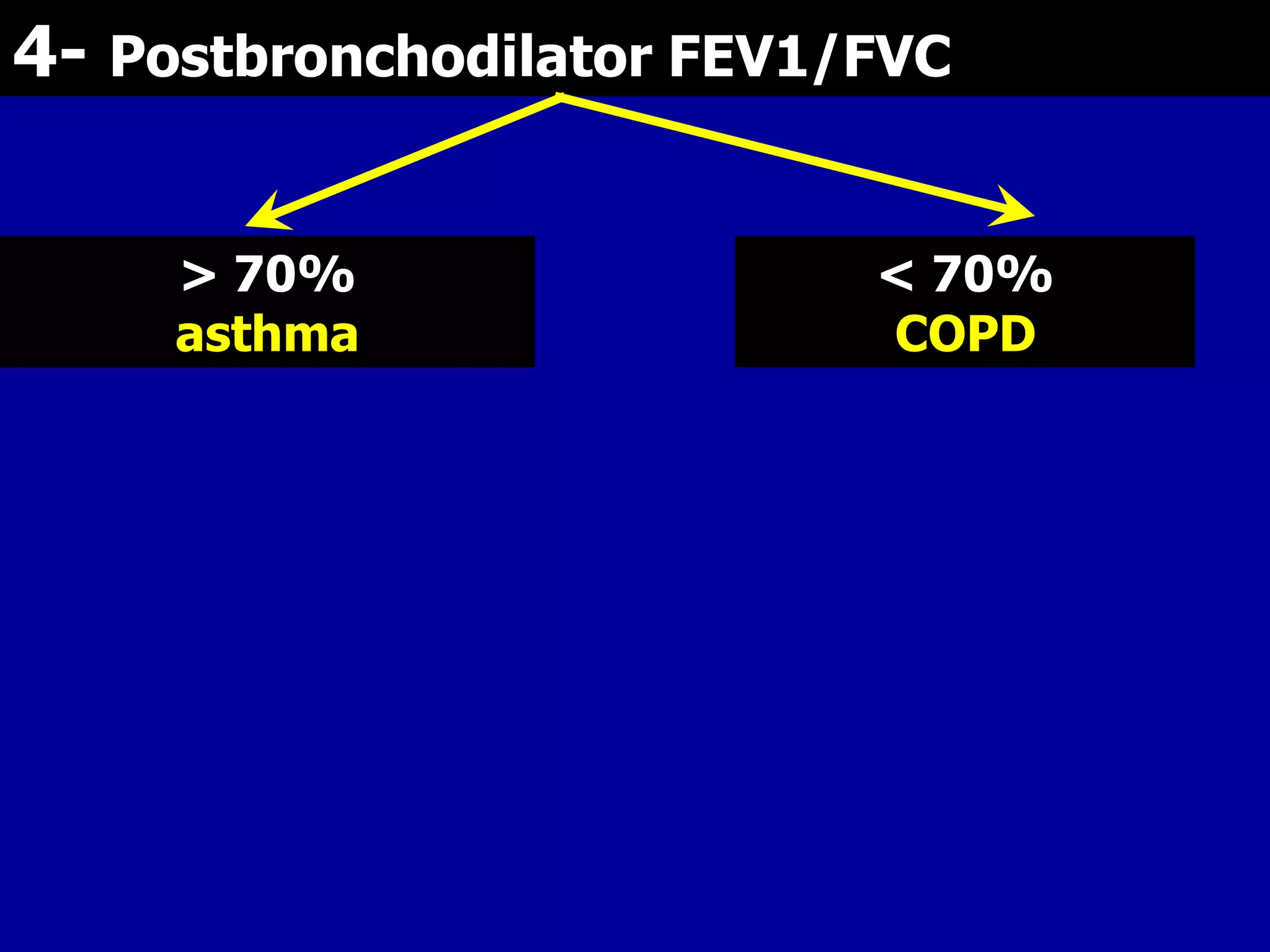
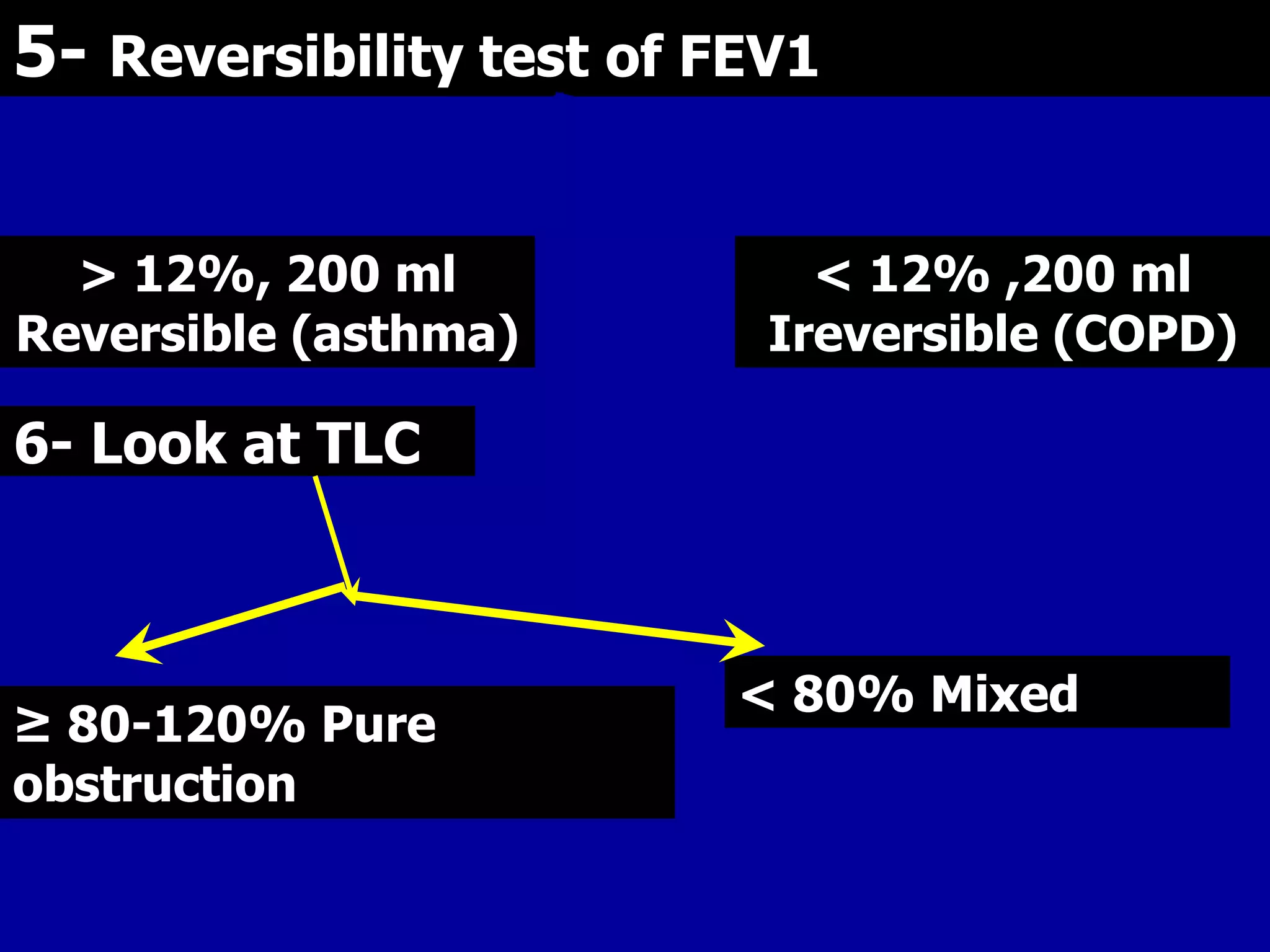
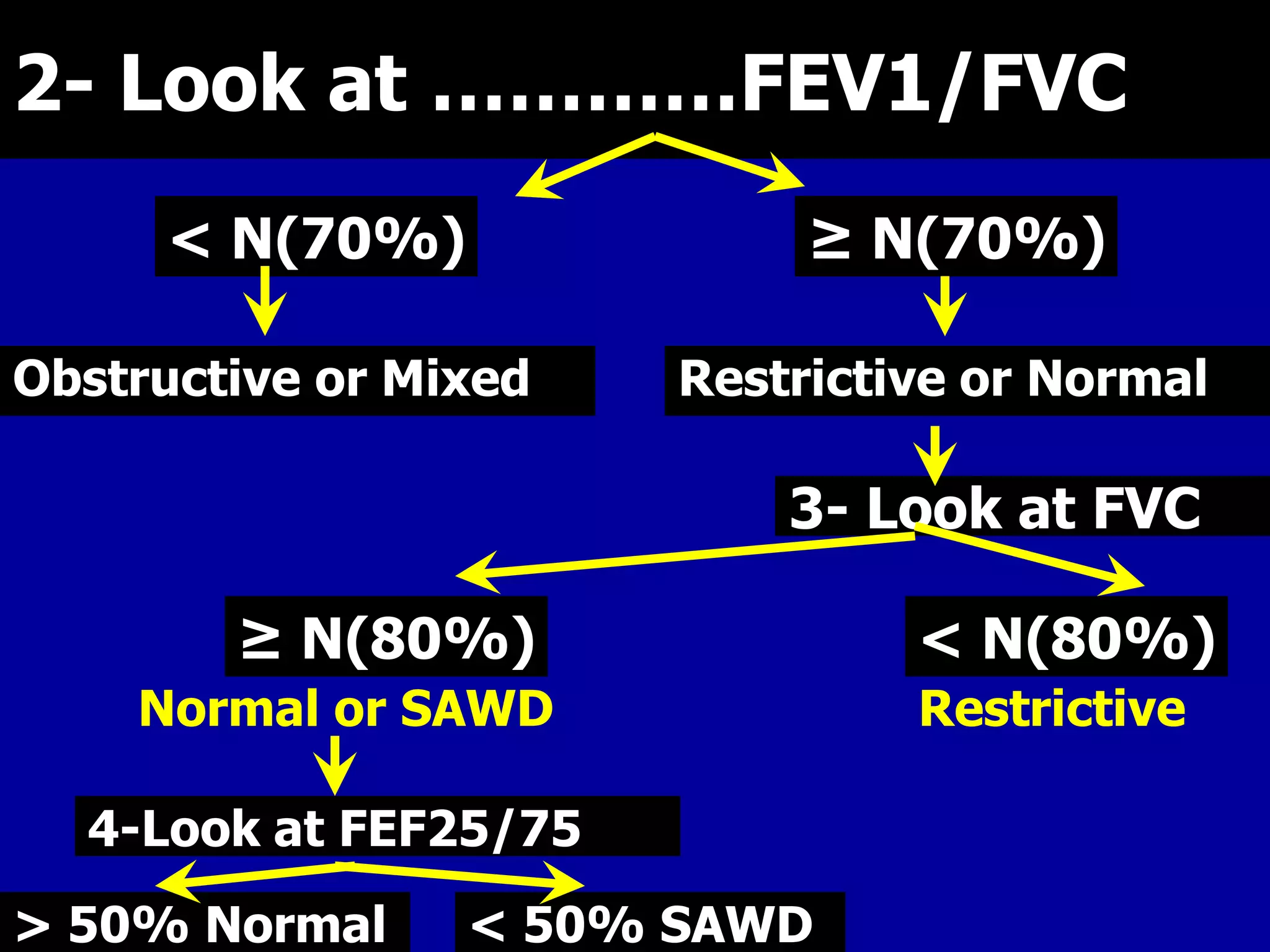
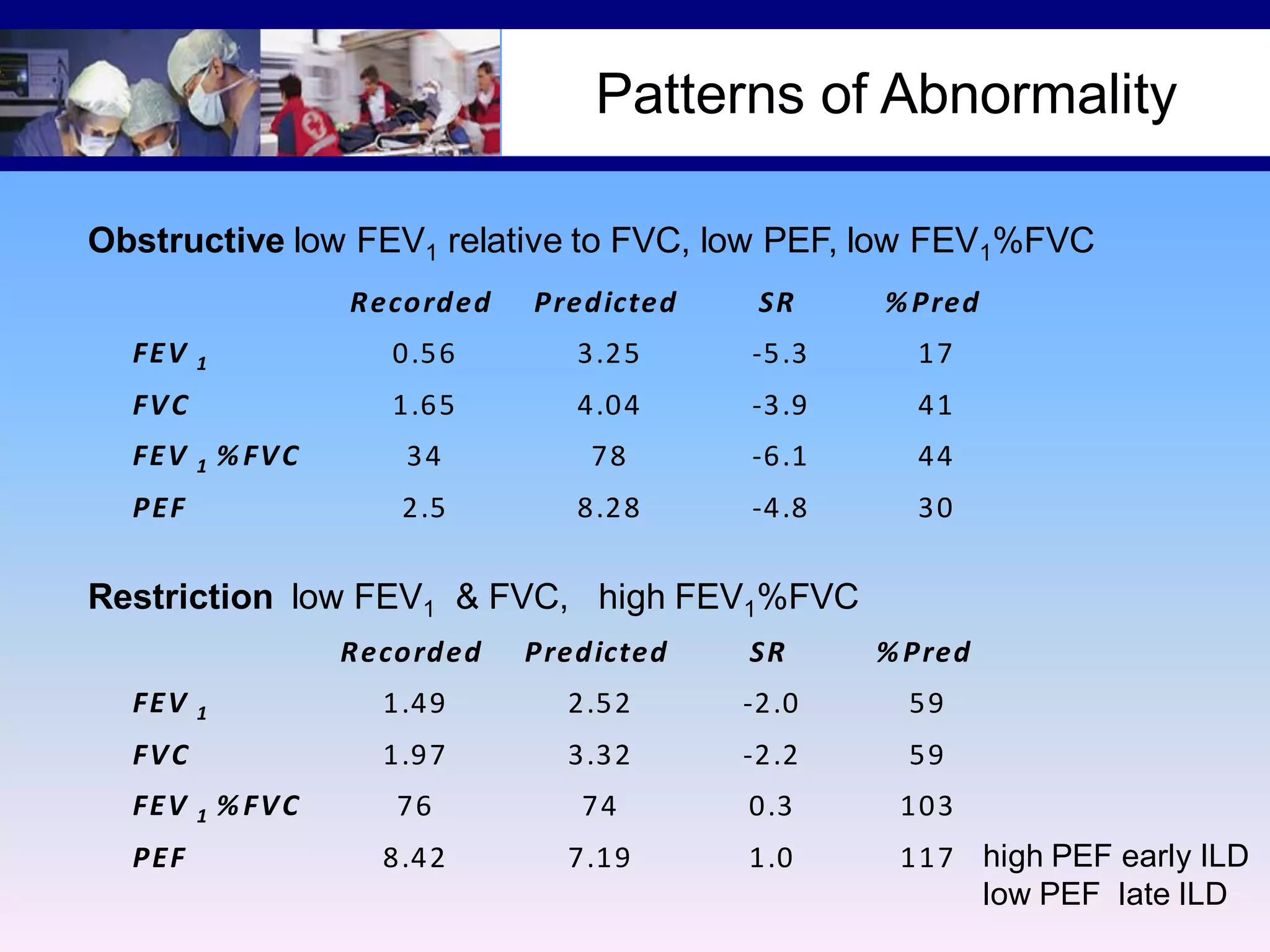
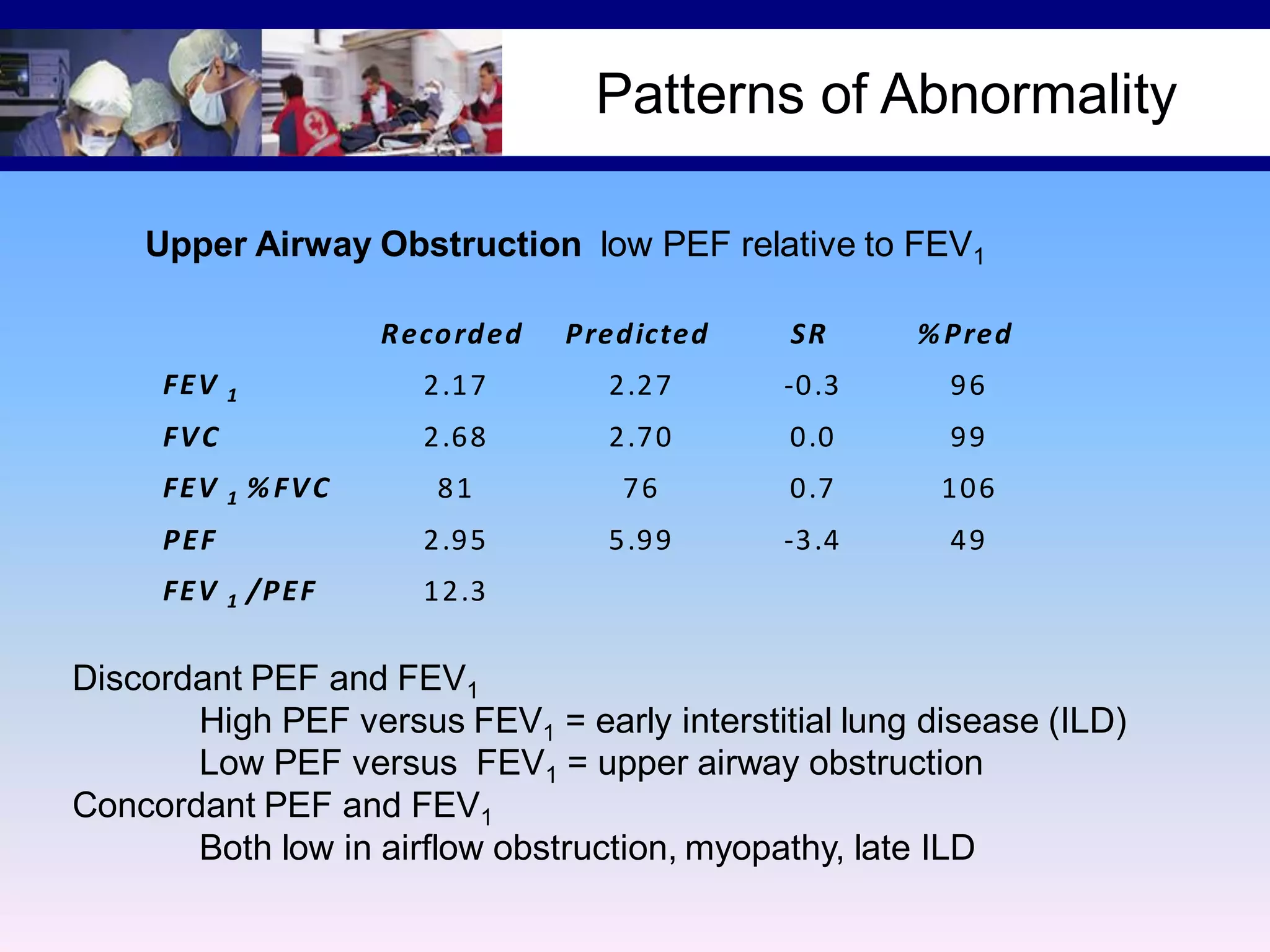
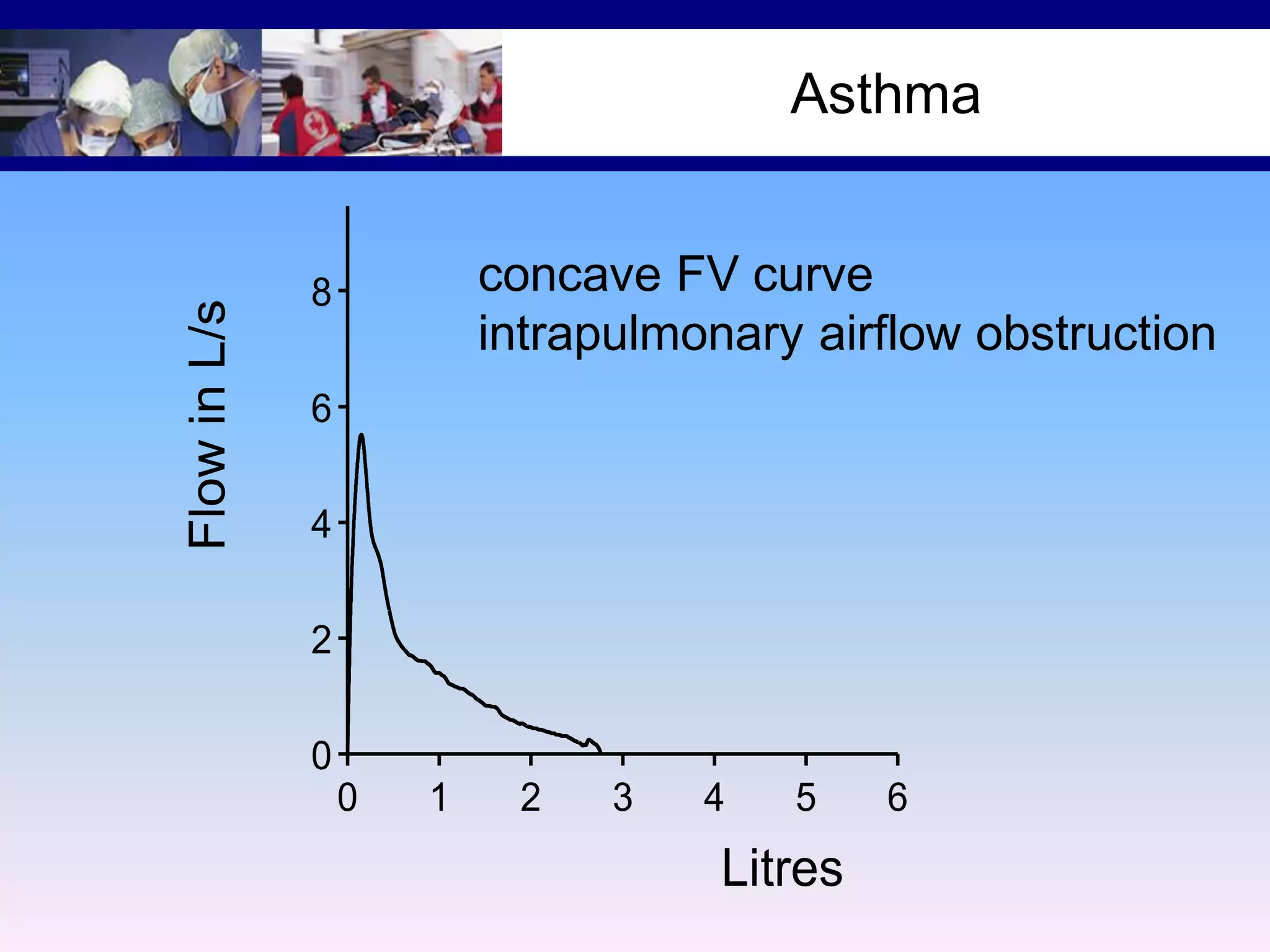
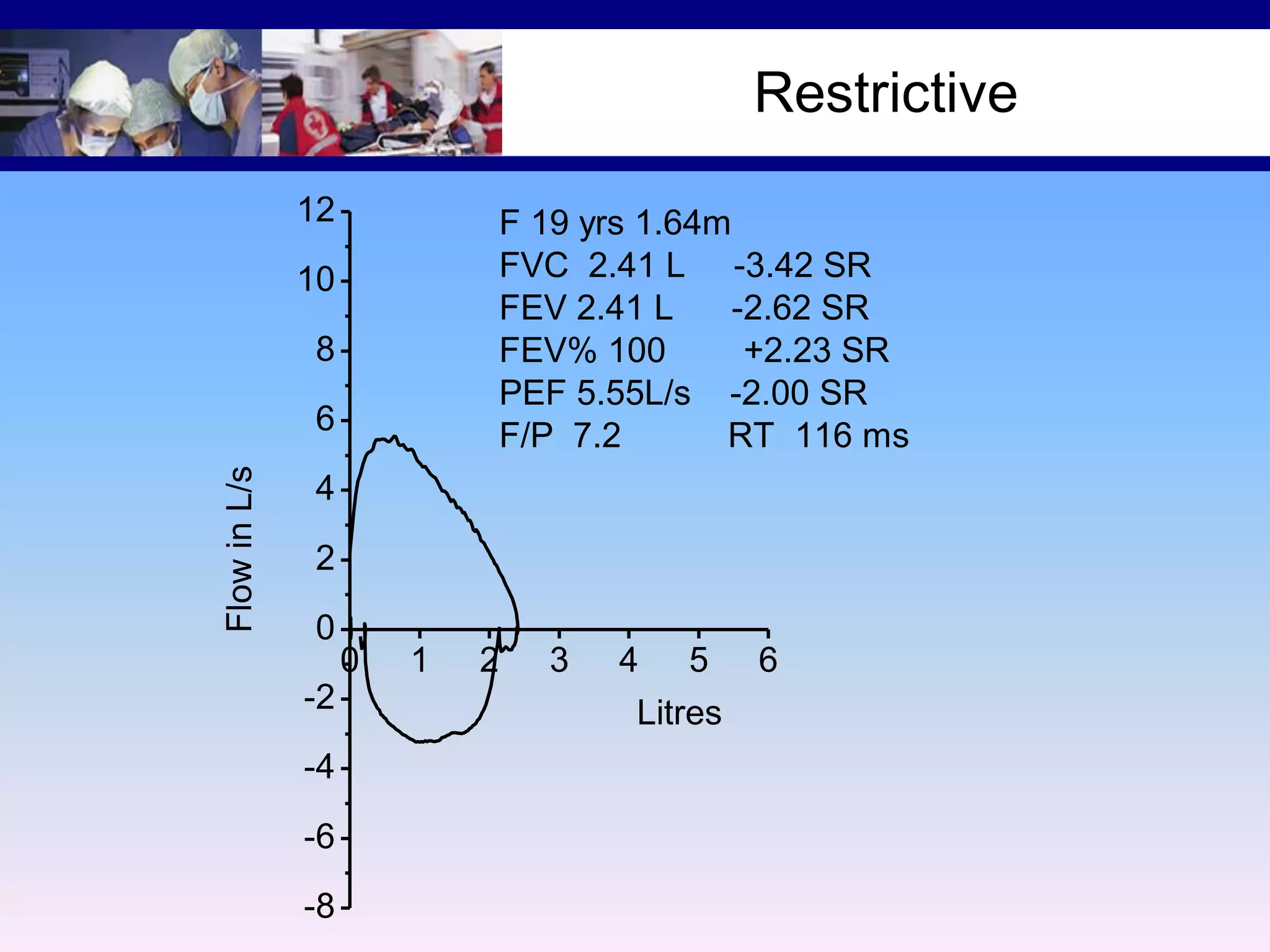
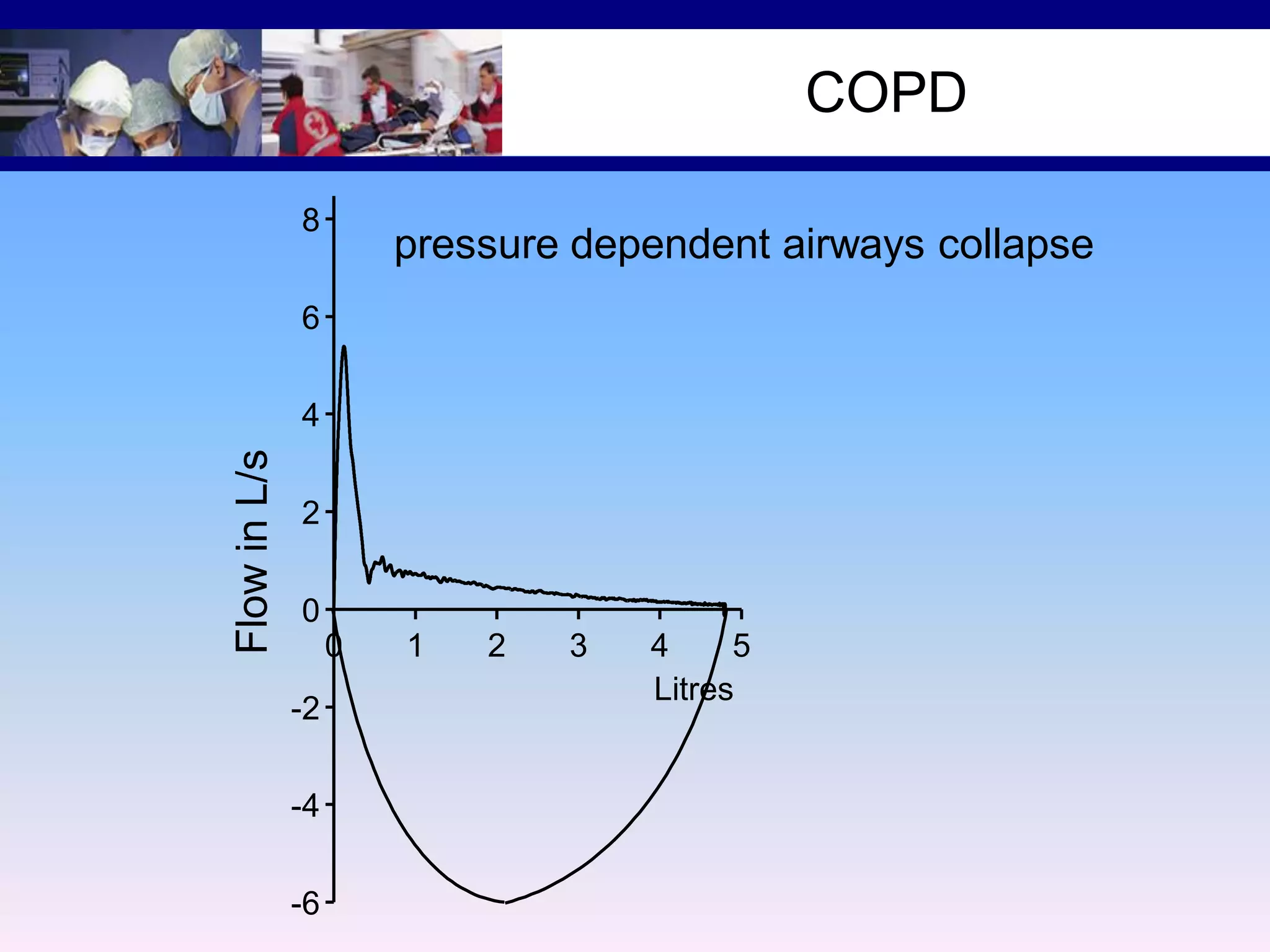
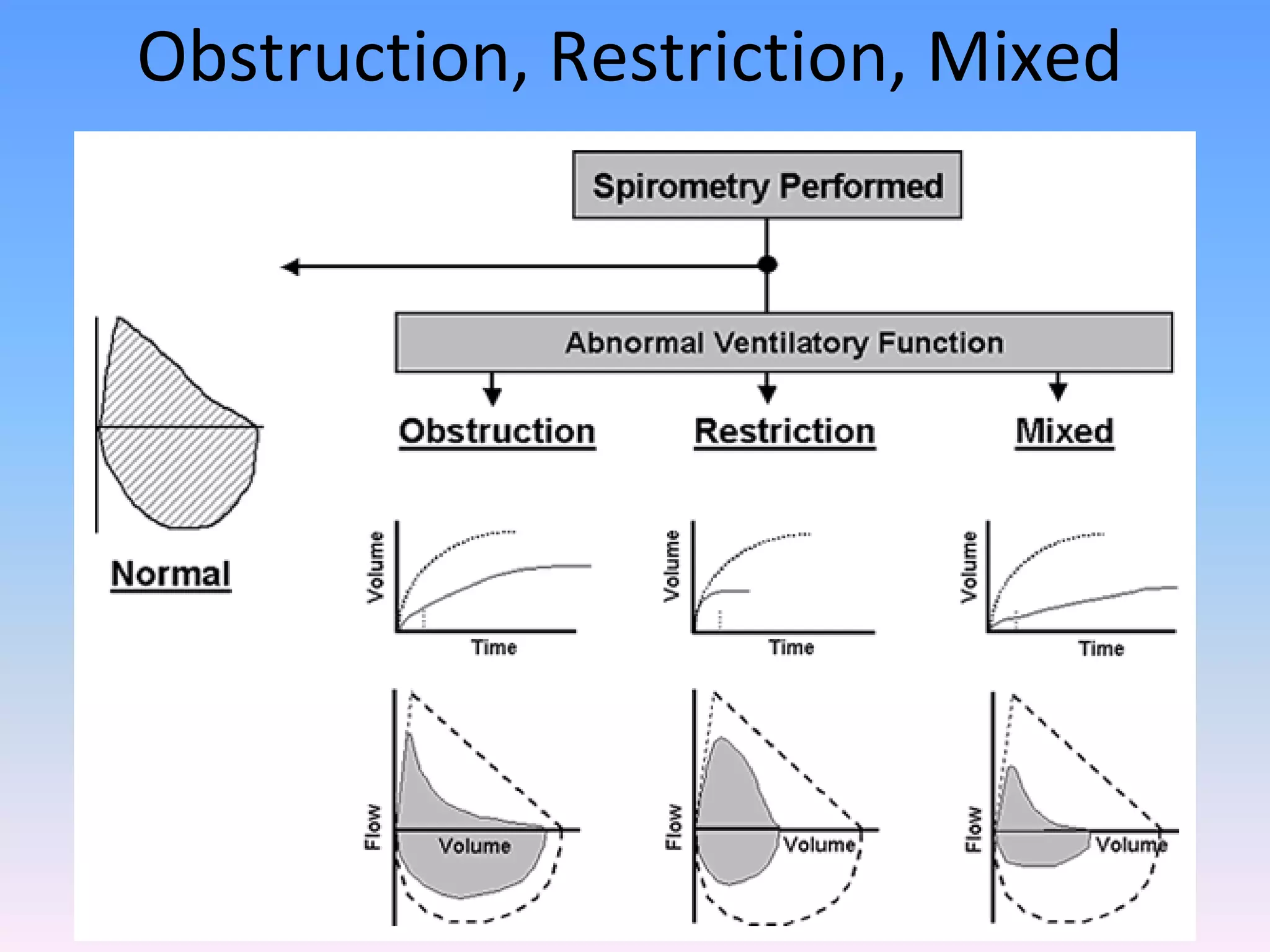
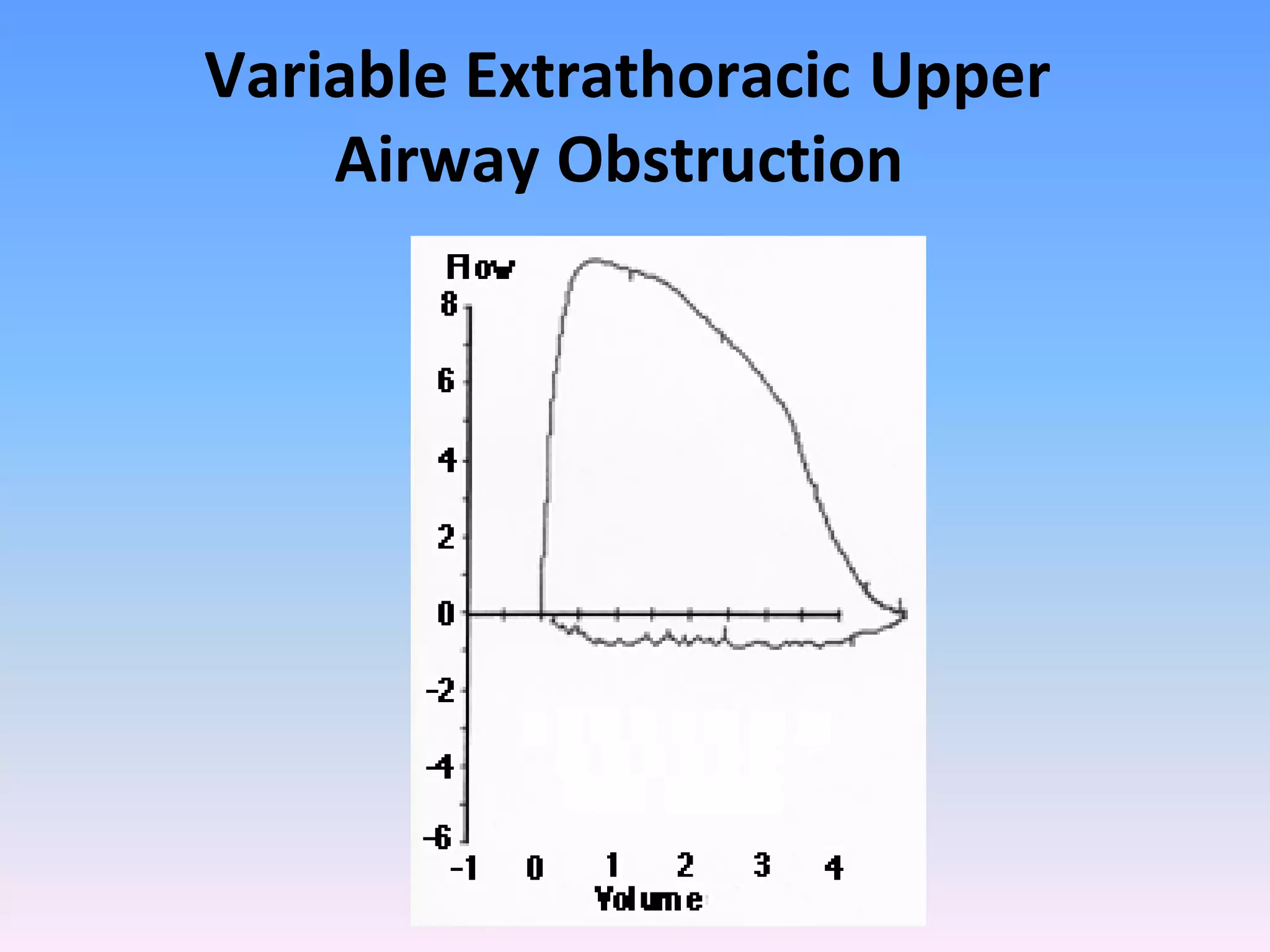
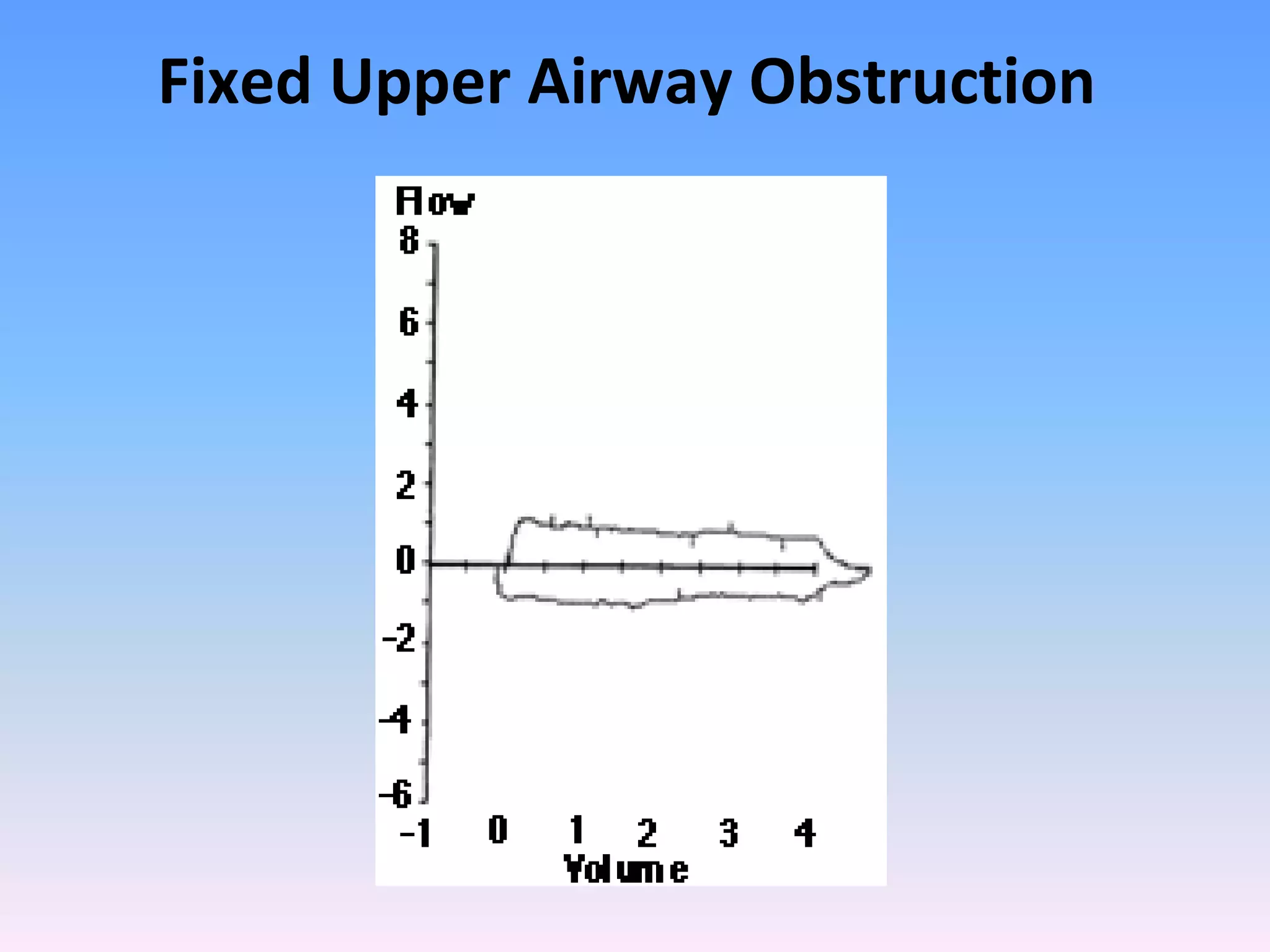
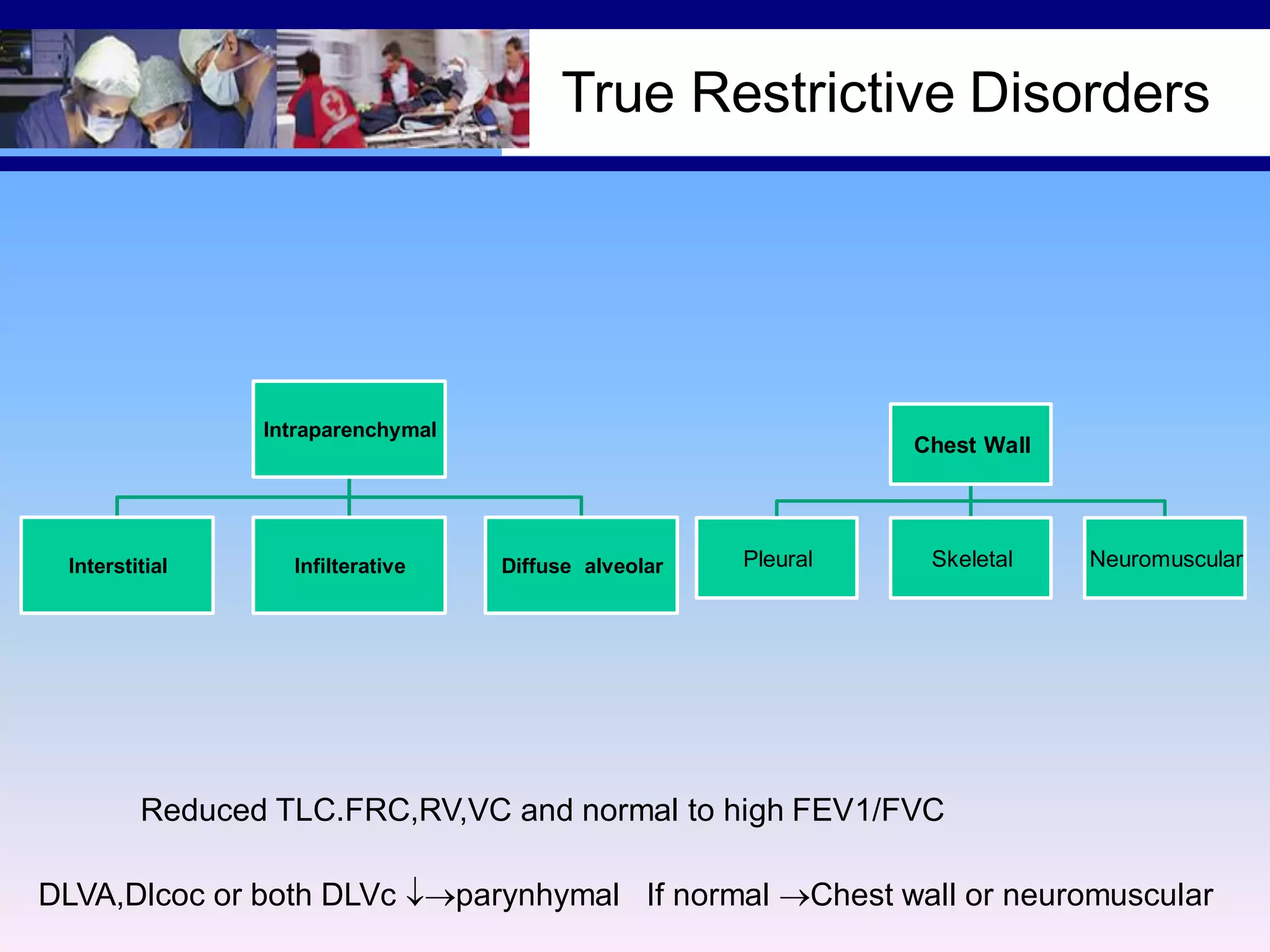
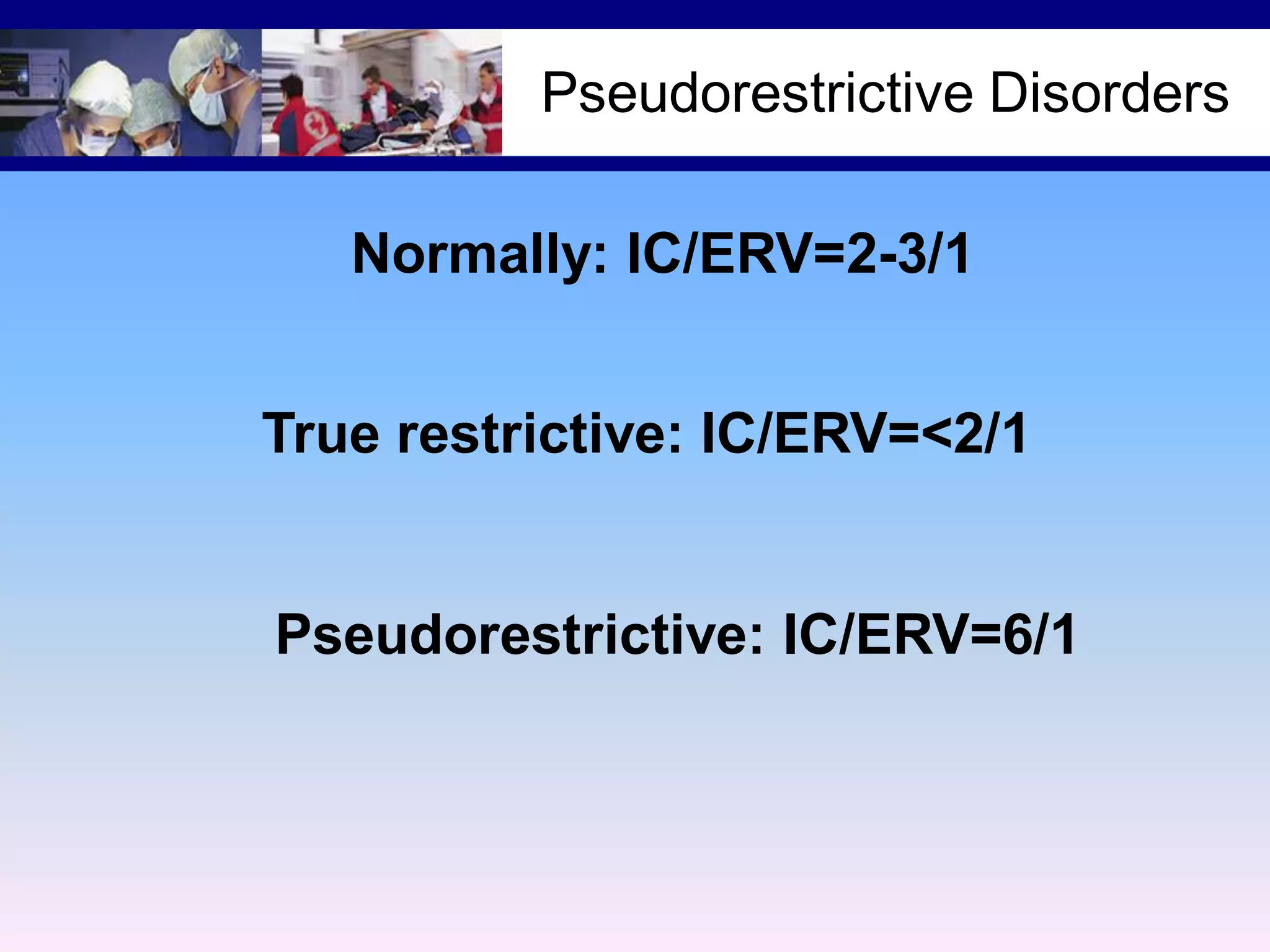
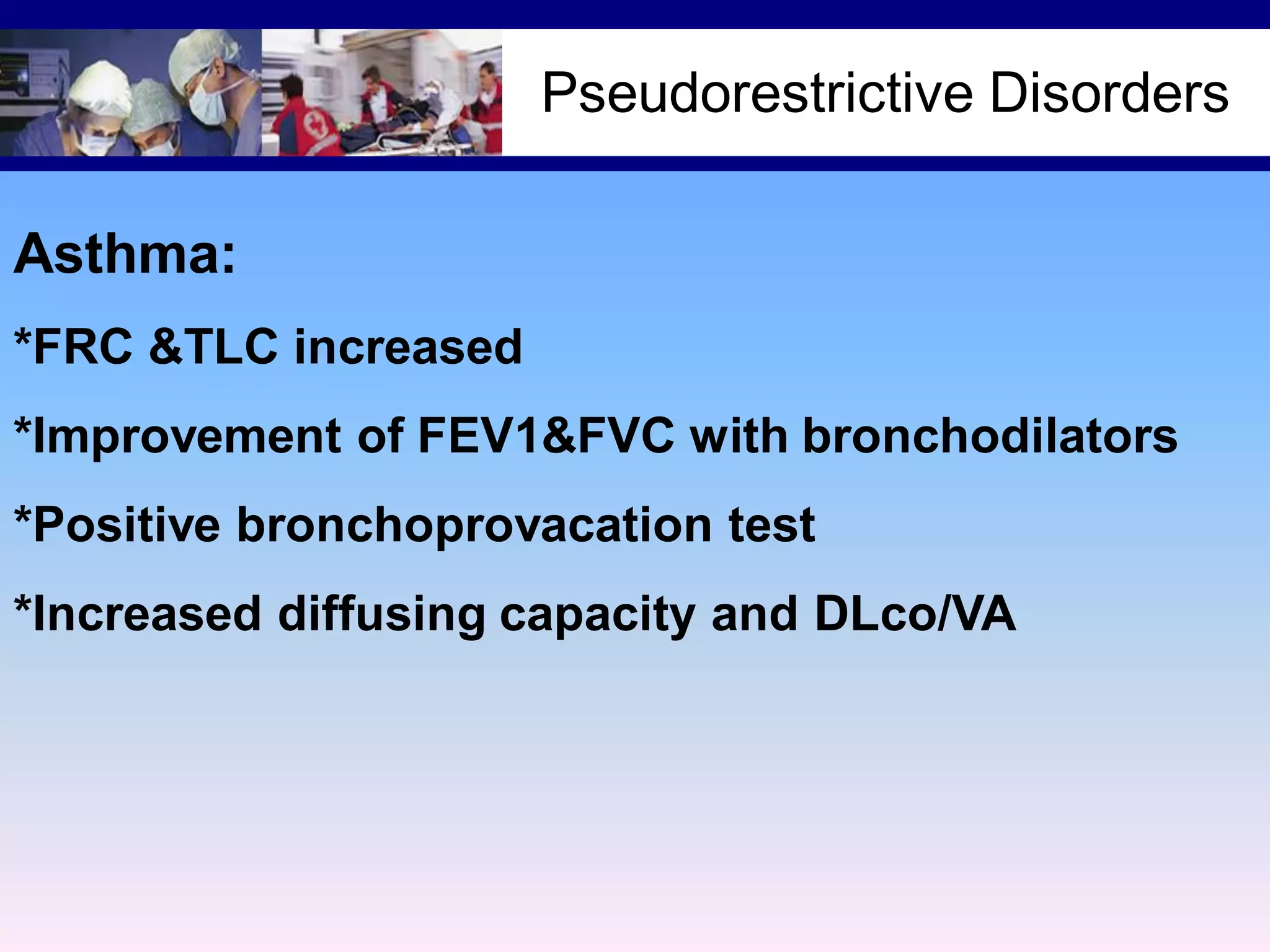
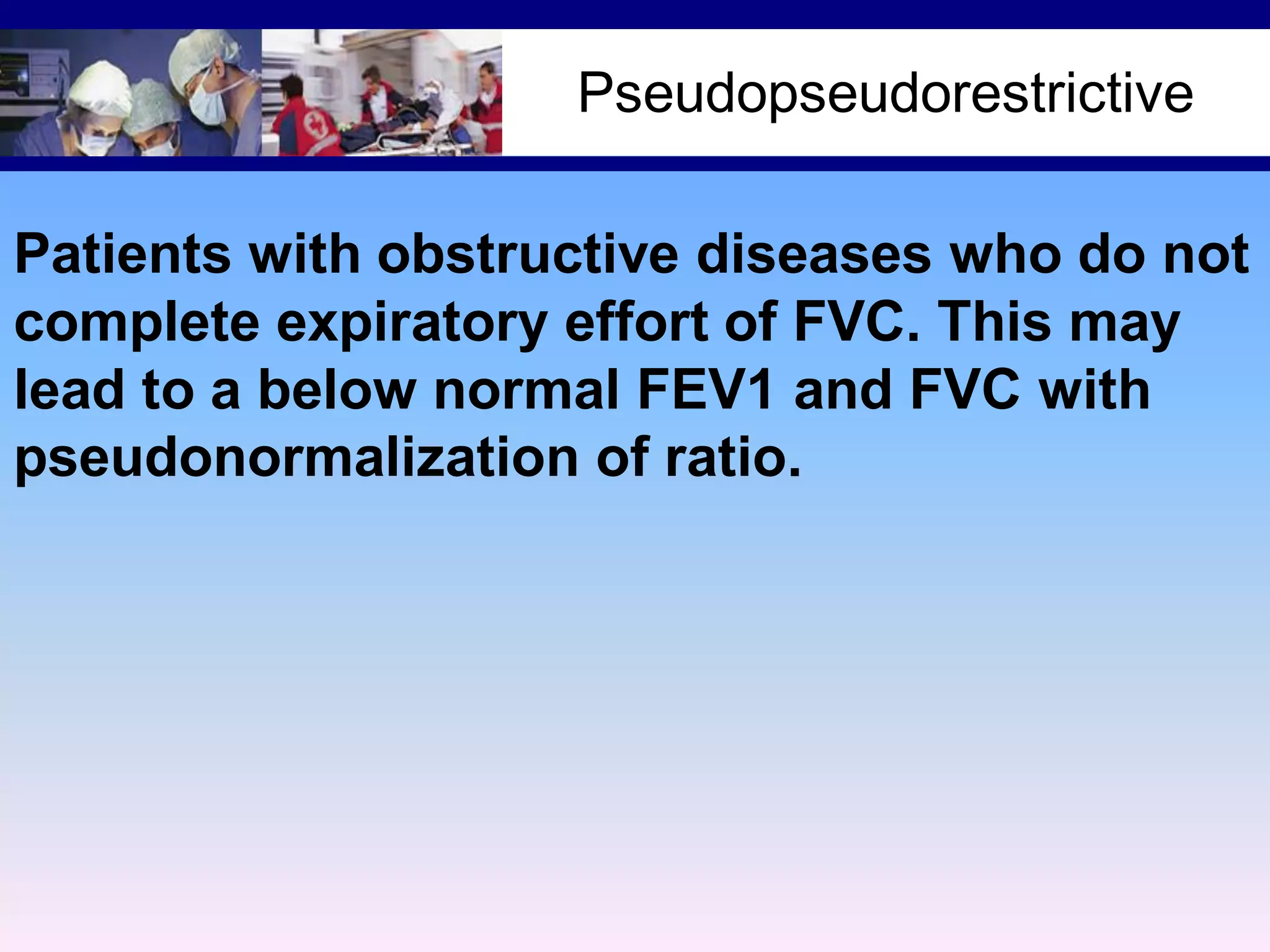
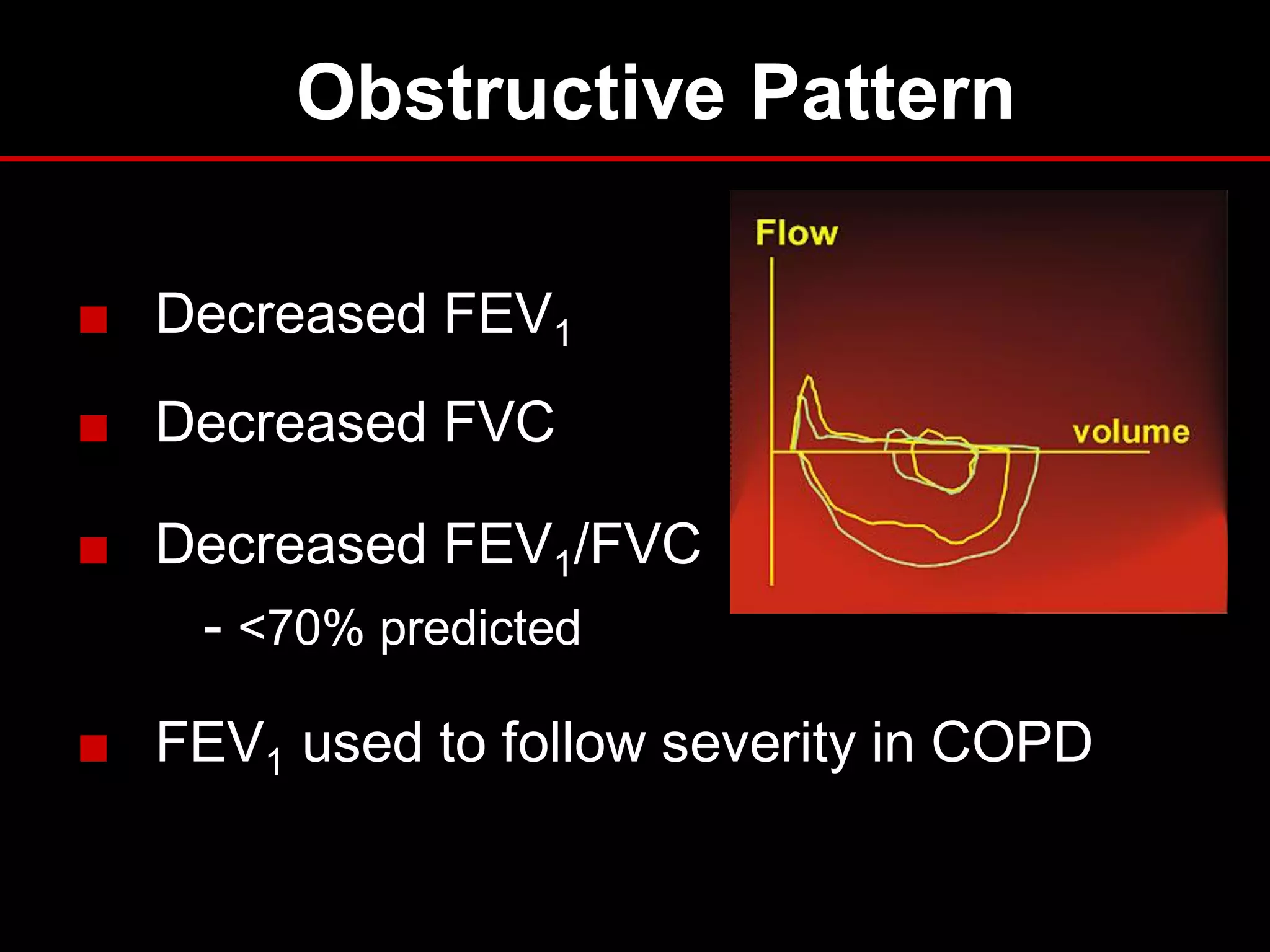
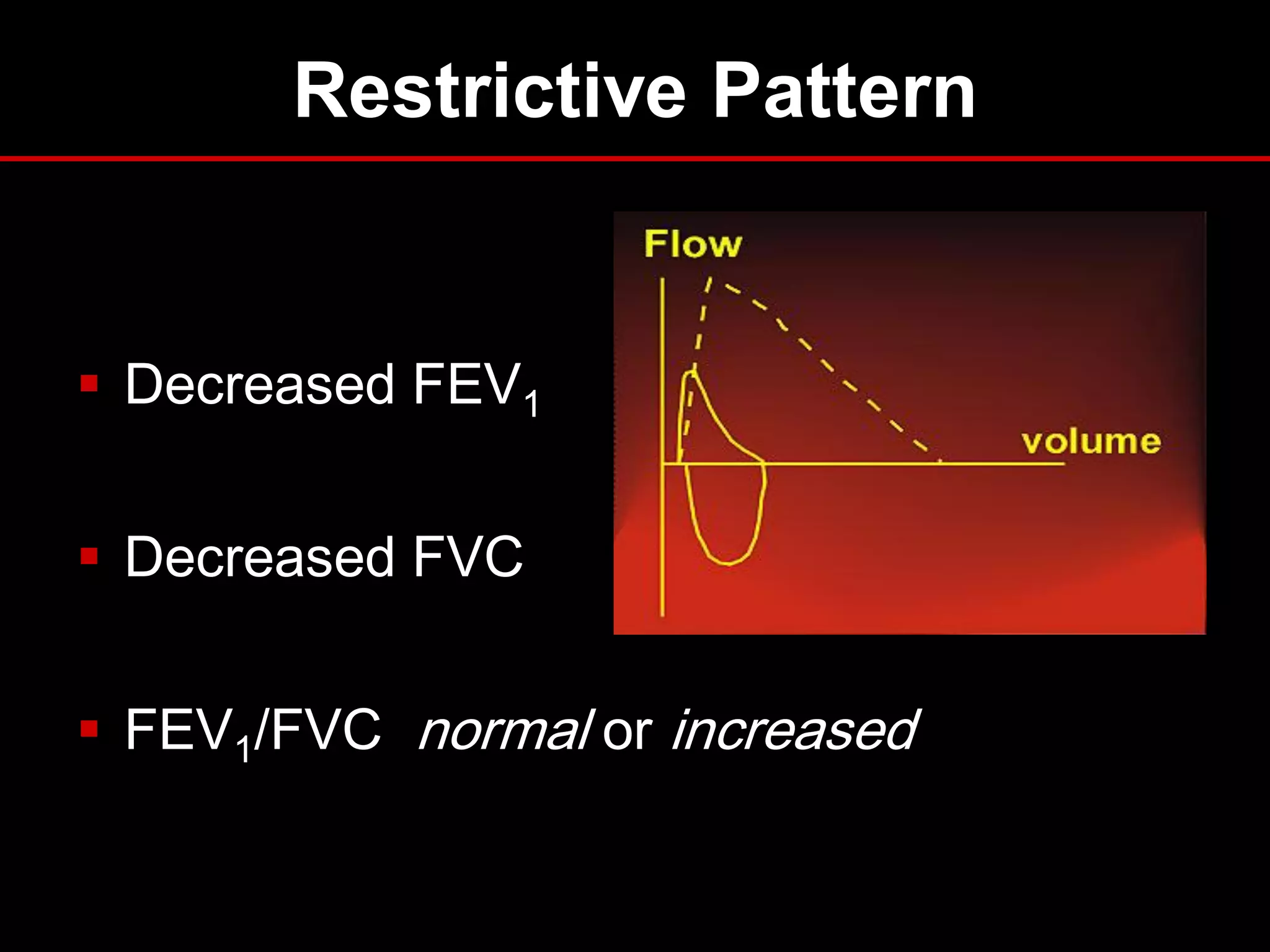
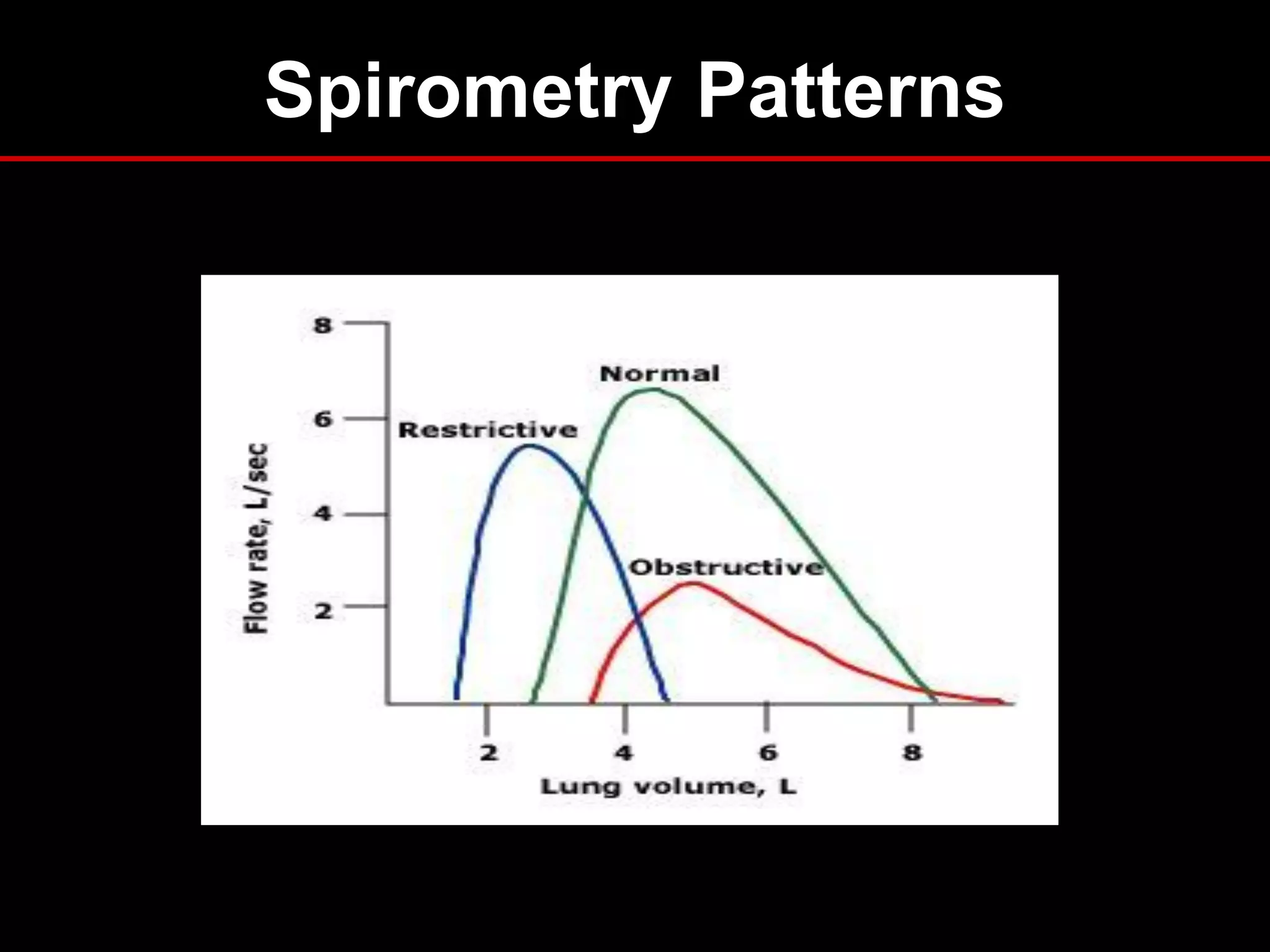
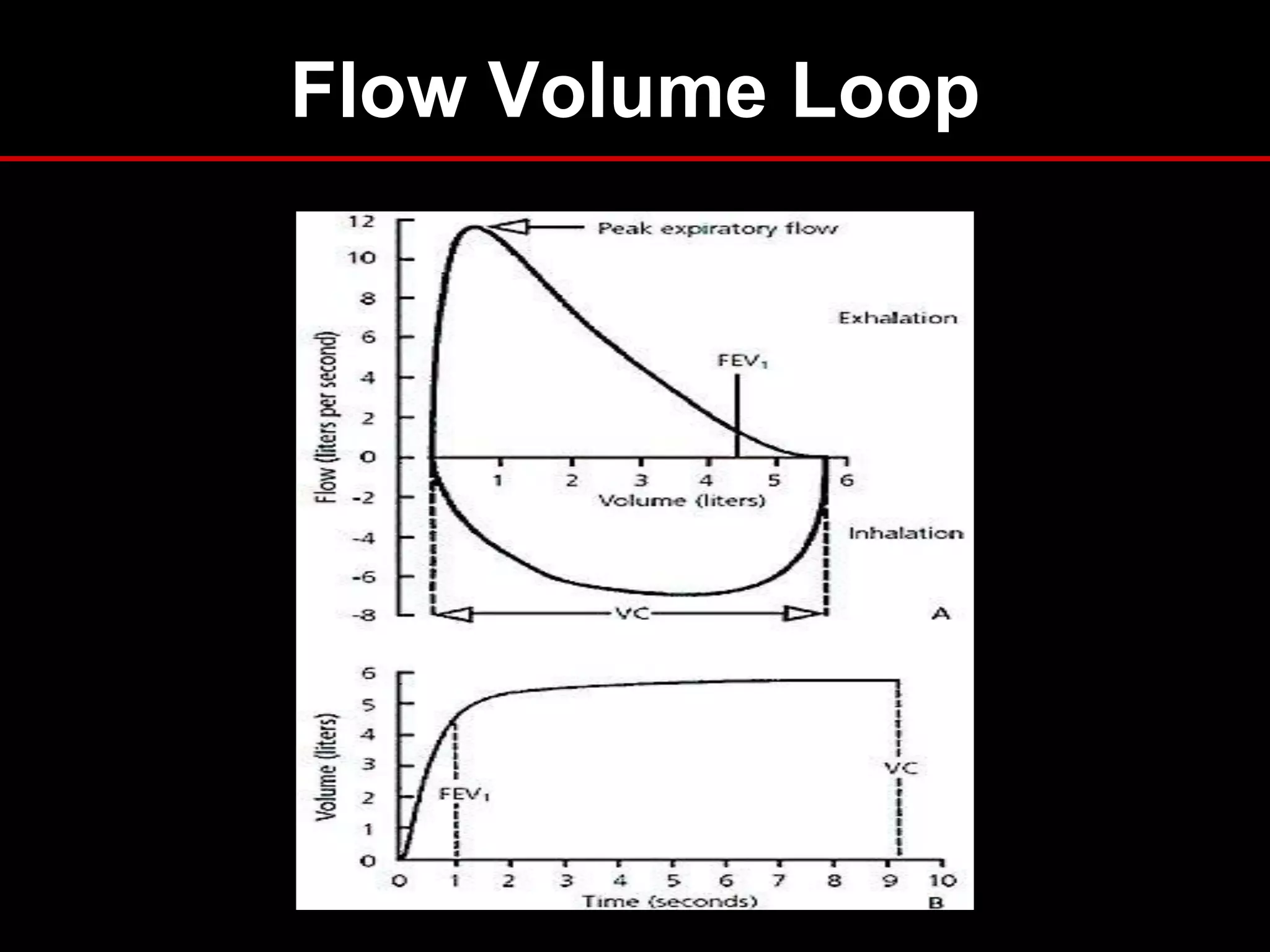
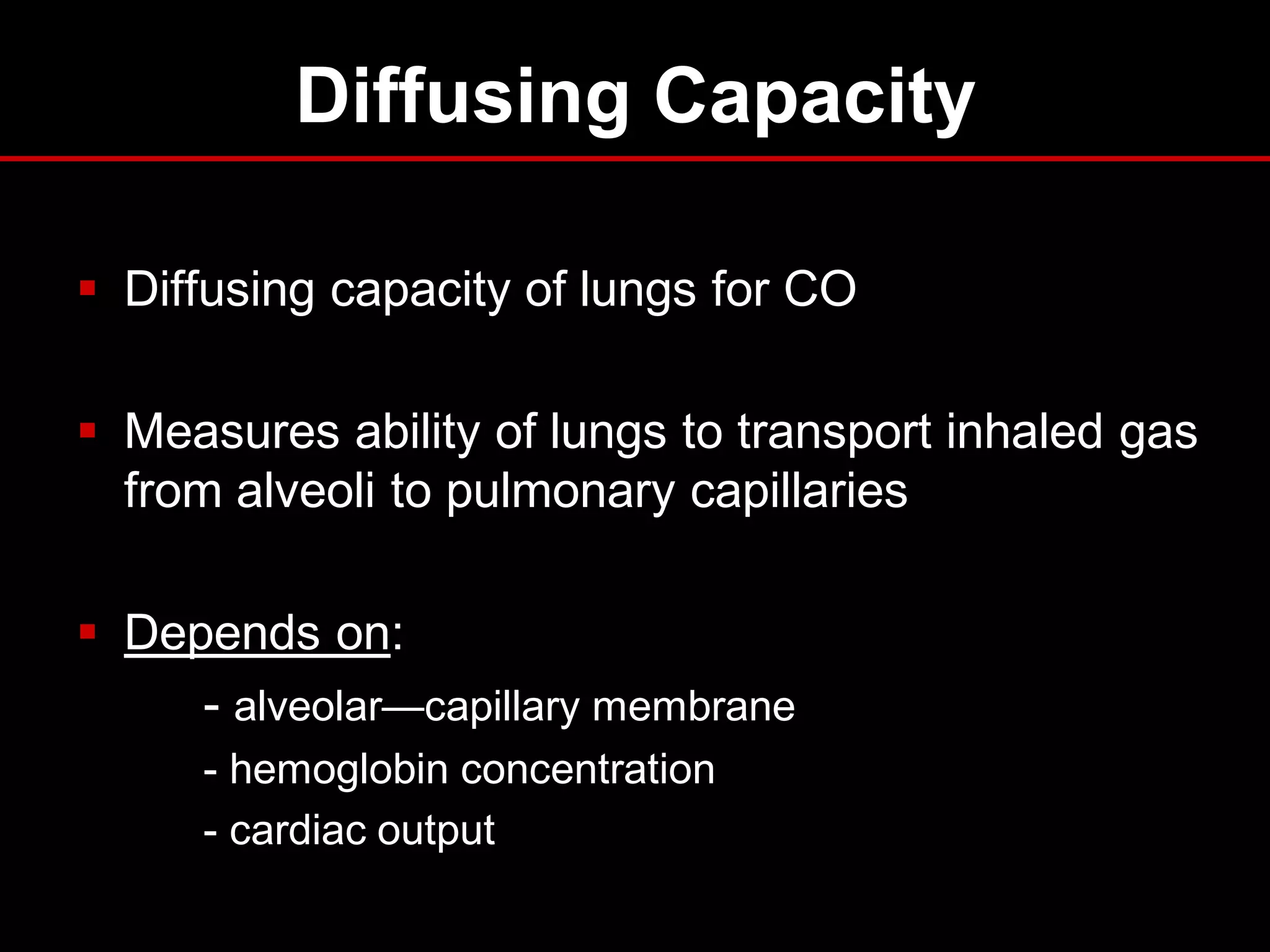
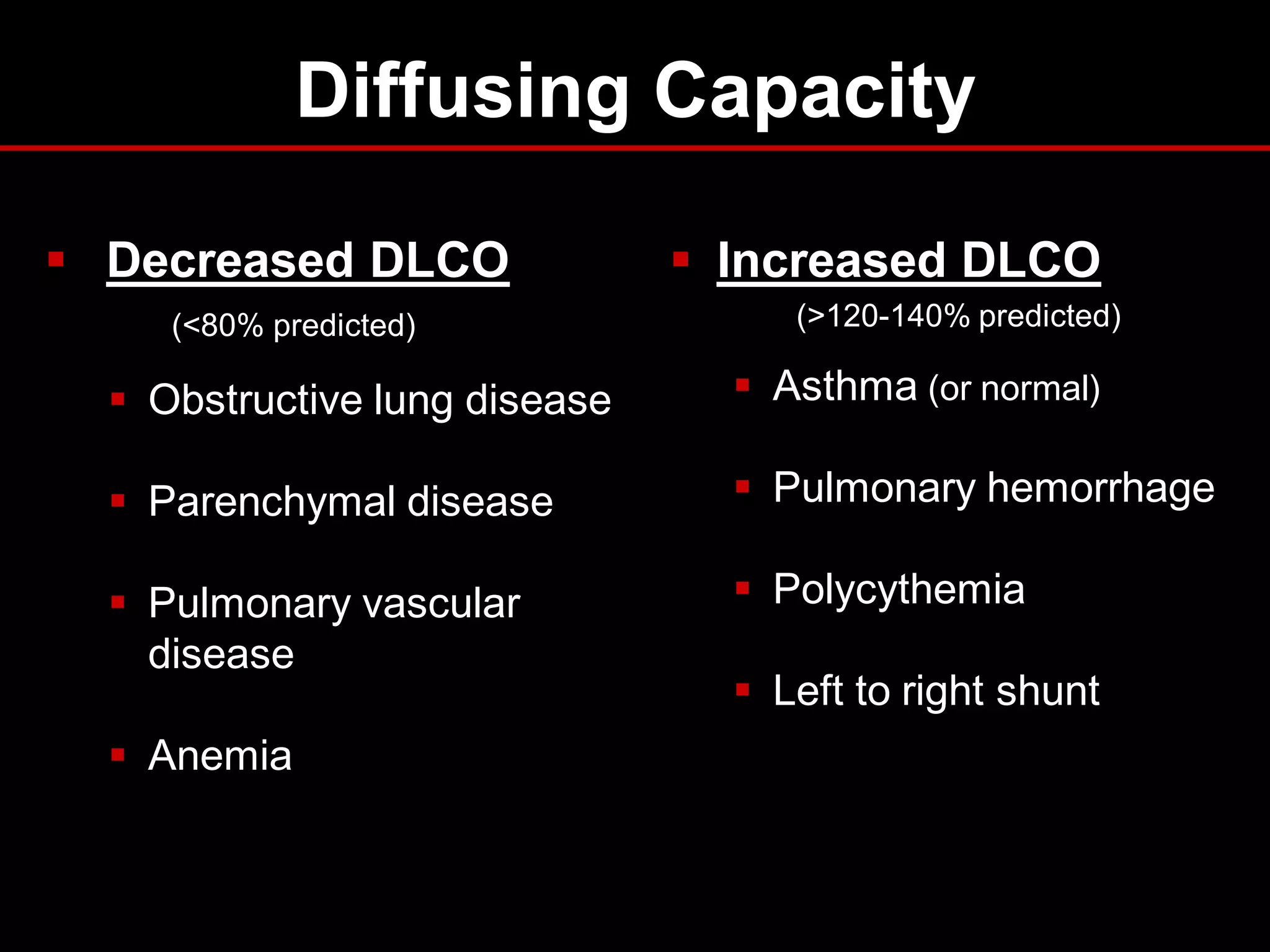
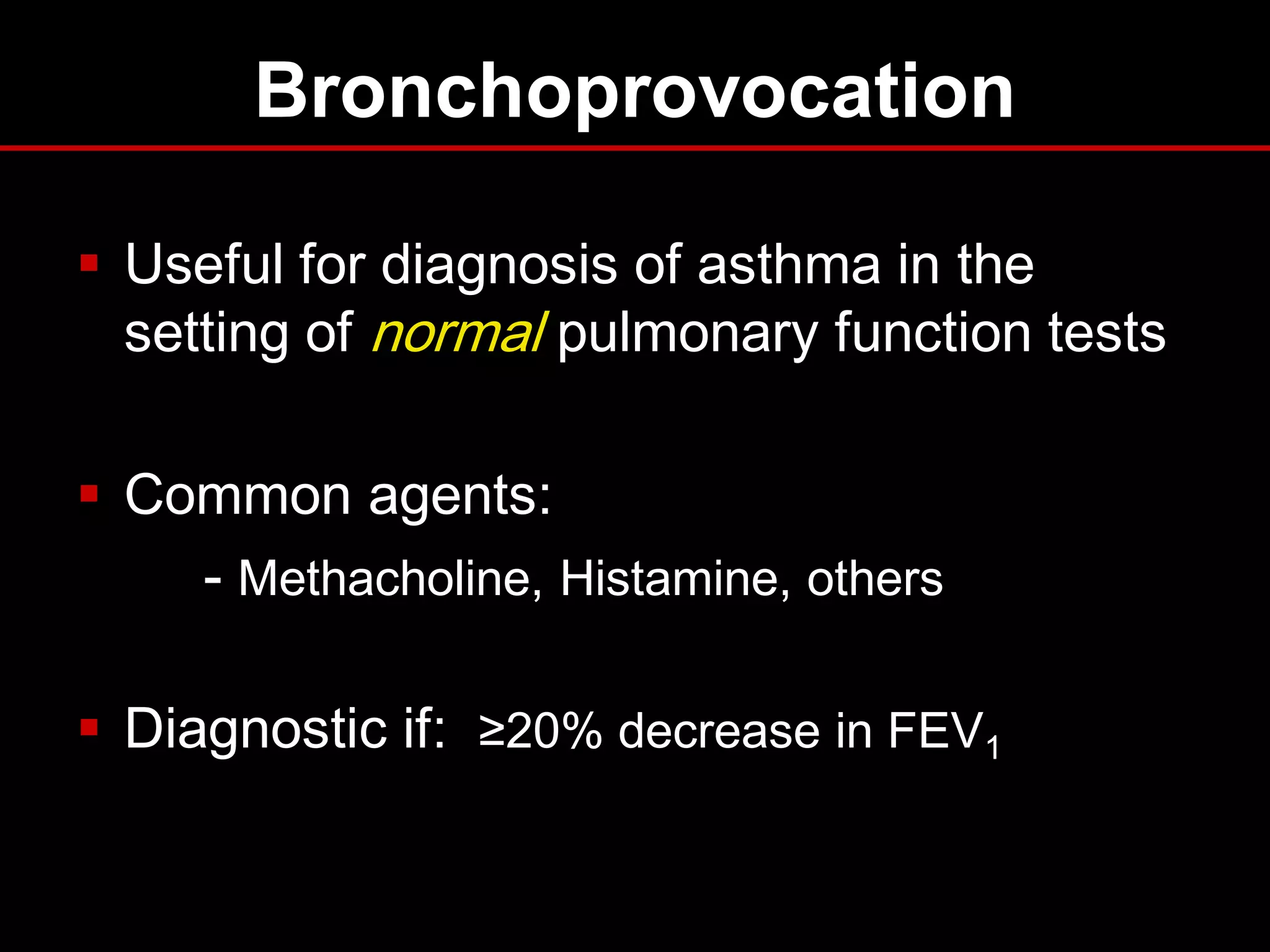
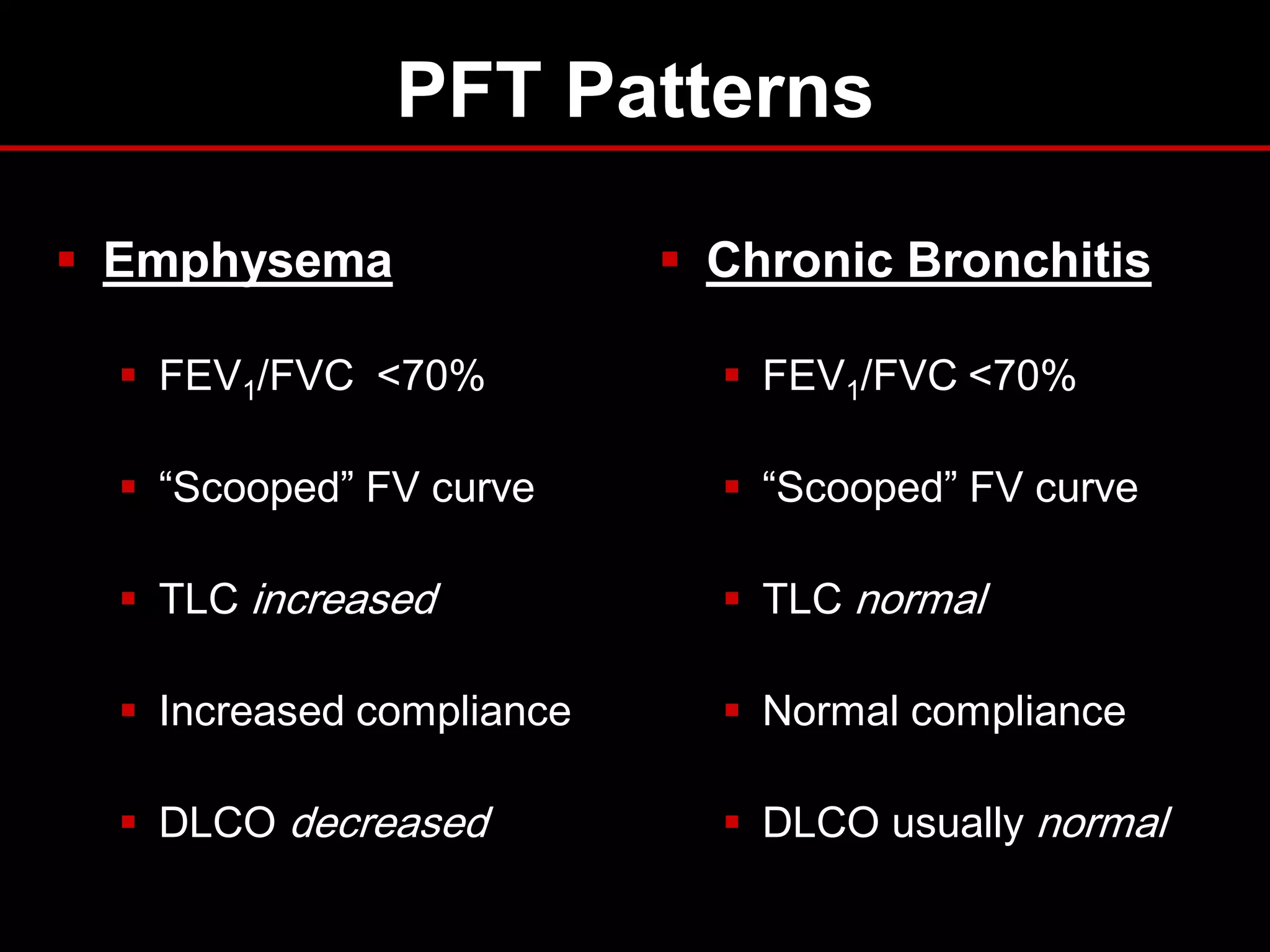
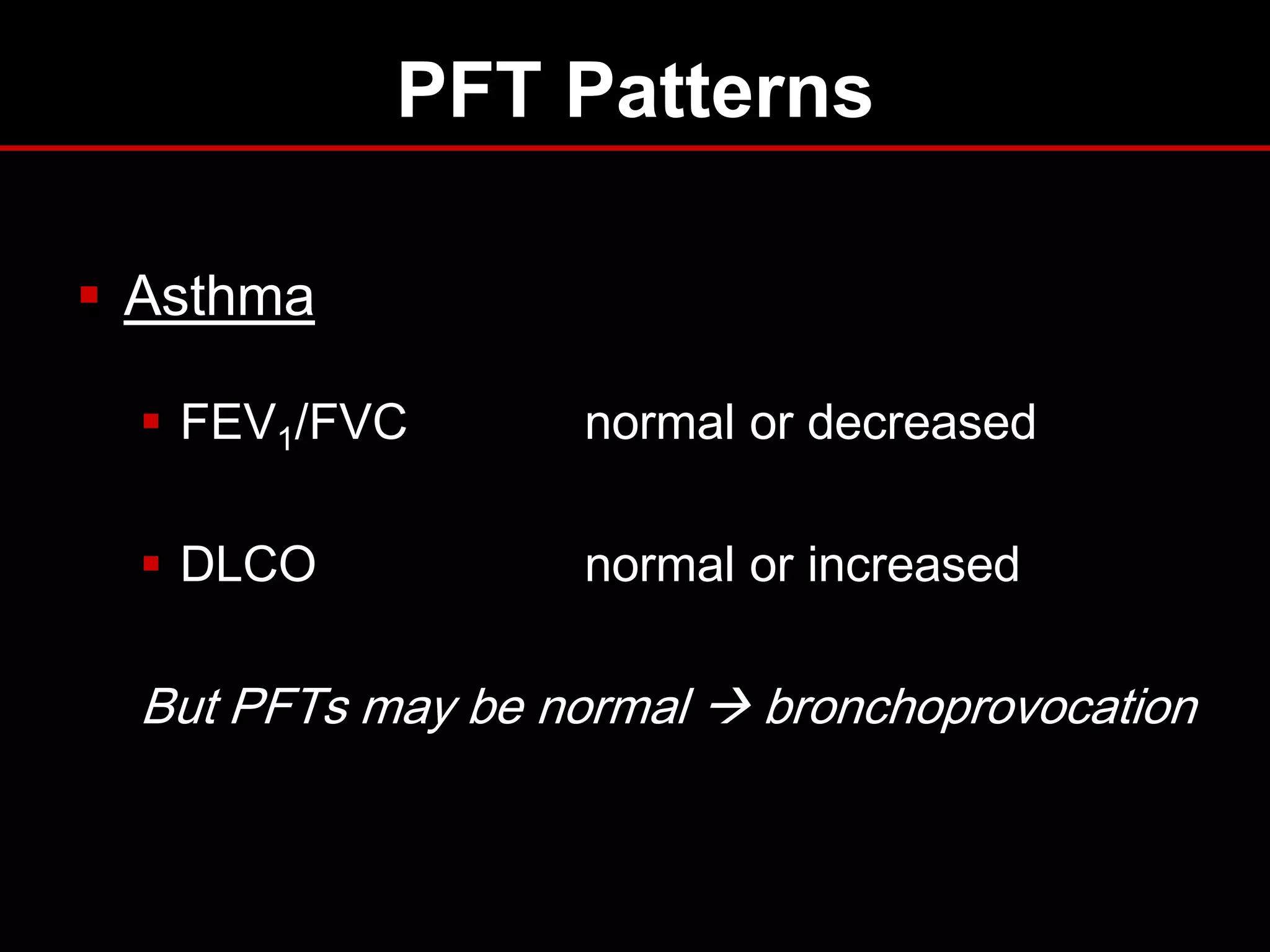
This document discusses spirometry testing for obstructive lung diseases such as COPD and asthma. It provides information on the different measures assessed during spirometry including FEV1, FVC, and FEF25-75. It describes how to interpret the results and what values indicate restrictive versus obstructive lung disease. Guidelines for pre- and post-bronchodilator spirometry are covered as well as how to assess for reversibility and bronchial hyperresponsiveness. The importance of spirometry for diagnosing and monitoring lung diseases like COPD and asthma is emphasized.