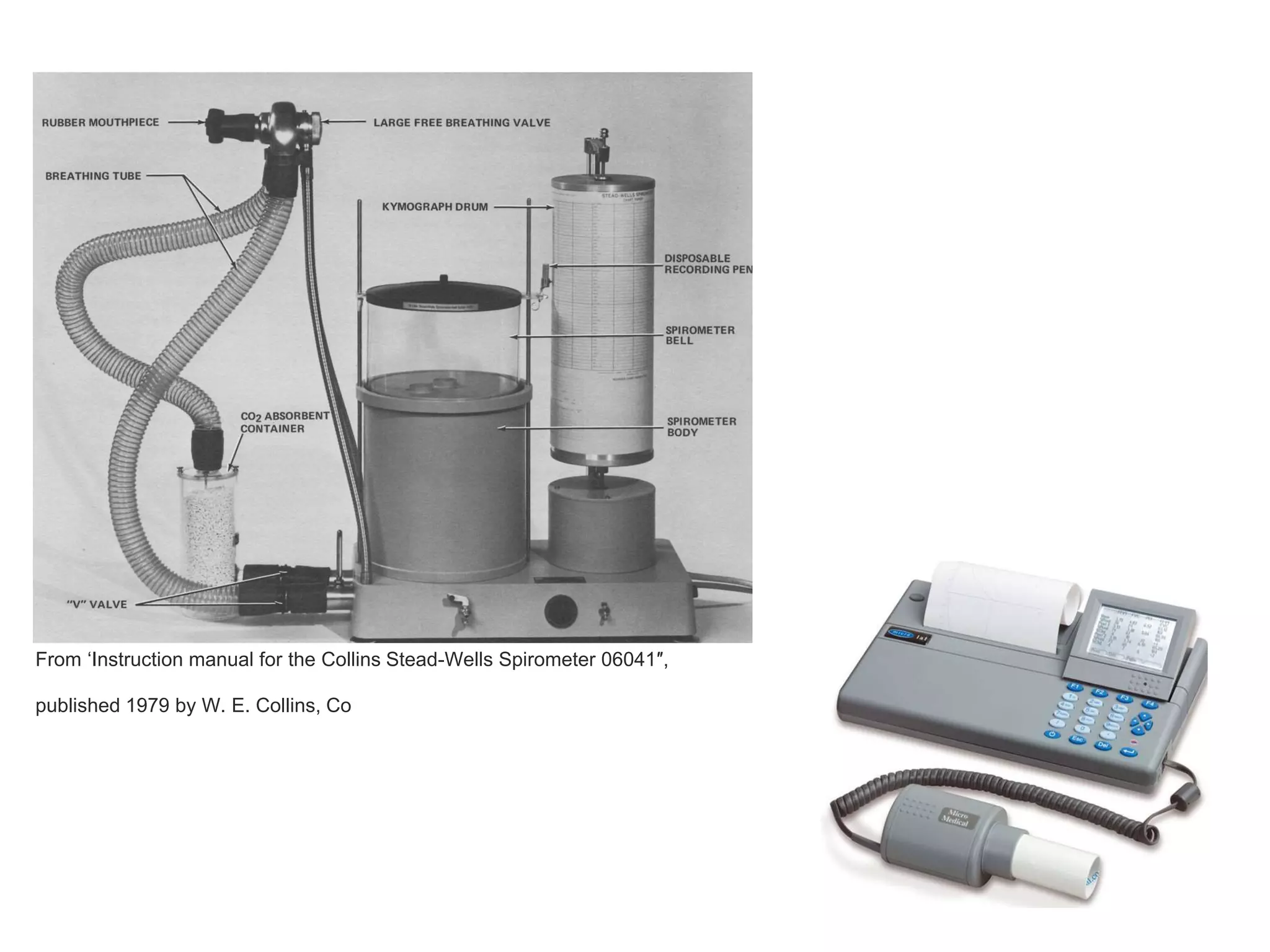
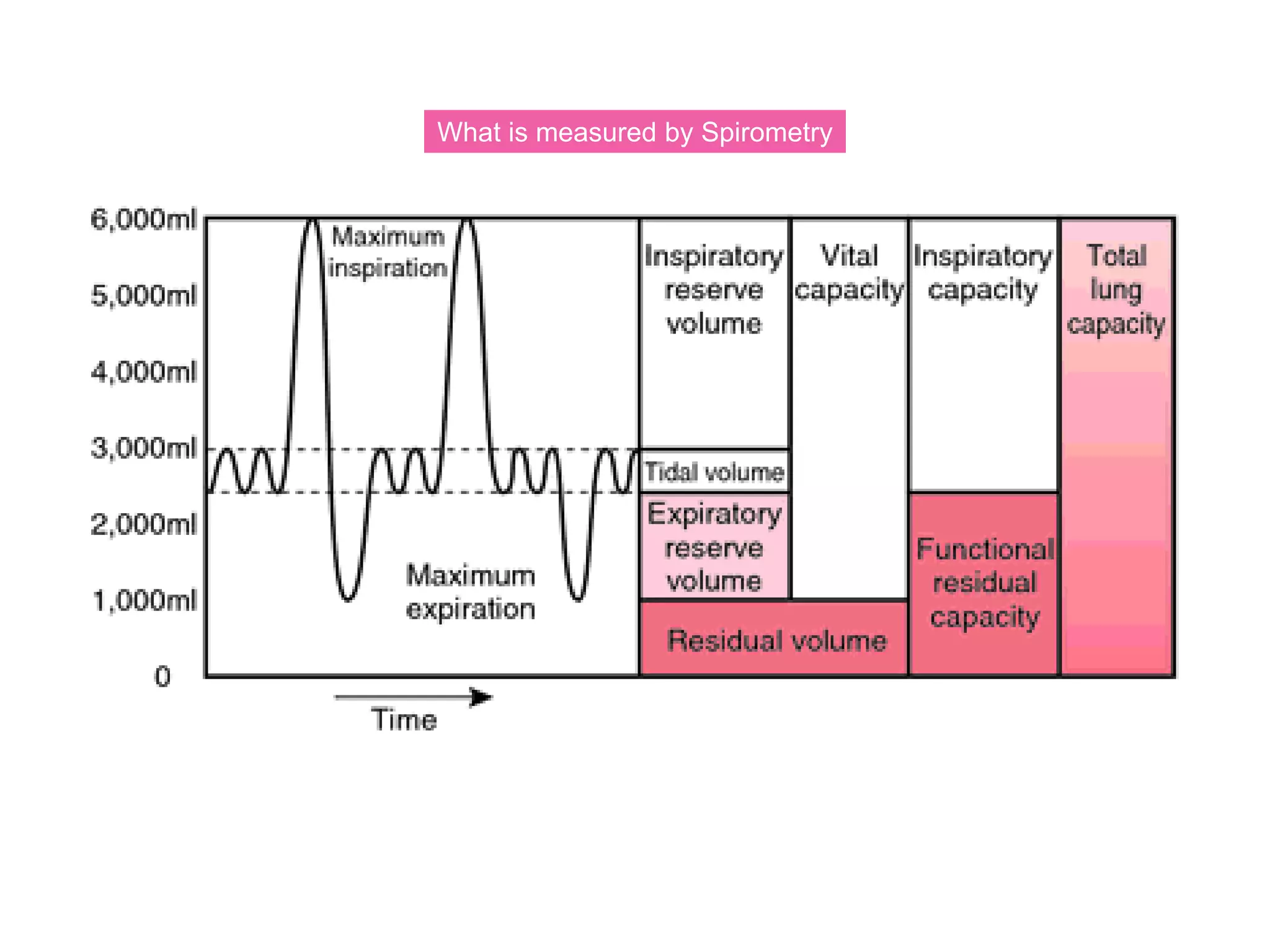
The document provides an overview of spirometry, a key pulmonary function test that assesses lung function by measuring air inhalation and exhalation volumes. It outlines the history, types of spirometers, measurements involved, indications for use, and complications associated with the test. The document also emphasizes the importance of standardized procedures and proper interpretation of spirometry results in various clinical contexts, especially during the COVID-19 pandemic.