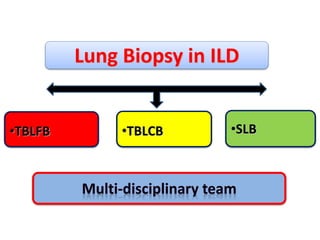
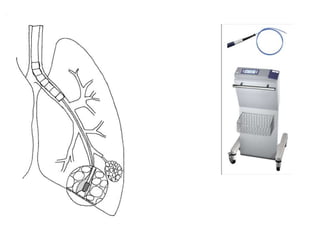
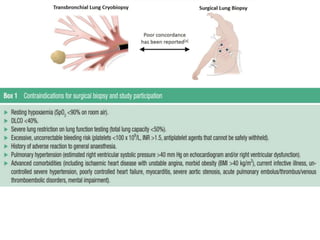
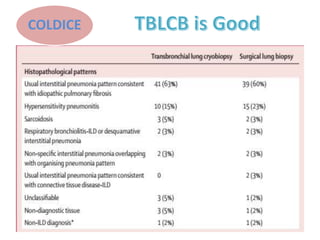
1) Transbronchial cryobiopsy is a bronchoscopic technique that uses extreme cold to obtain biopsy samples and has potential as a safer alternative to surgical lung biopsy for diagnosing interstitial lung diseases.
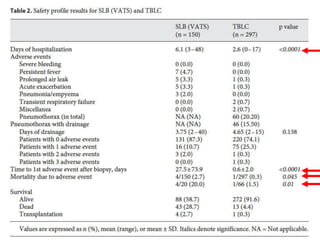
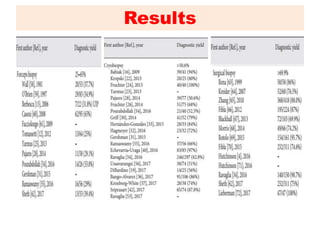
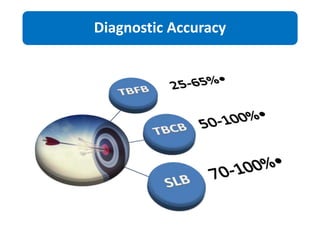
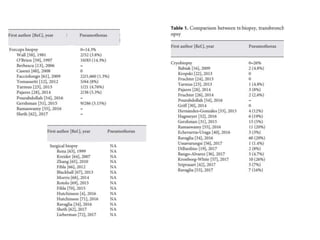
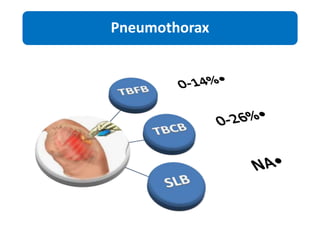
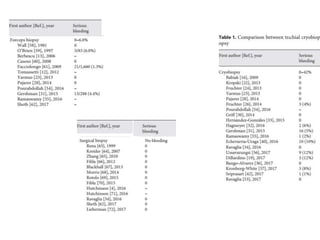
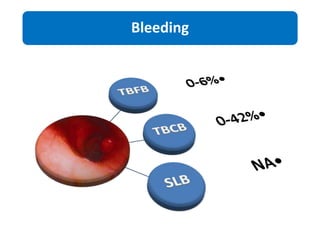
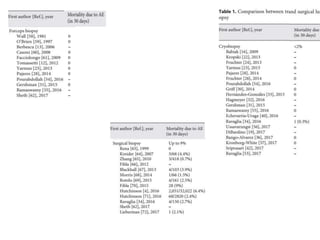
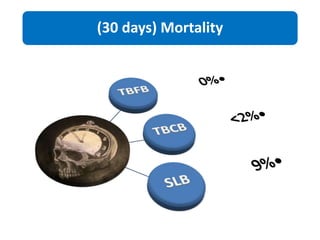
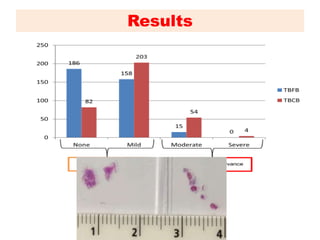
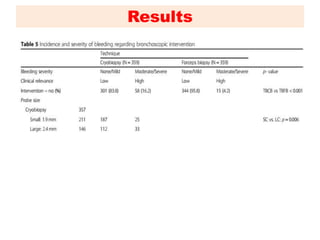
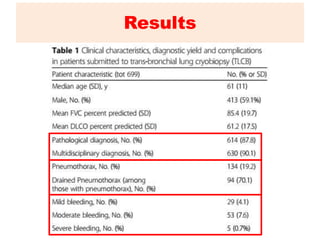
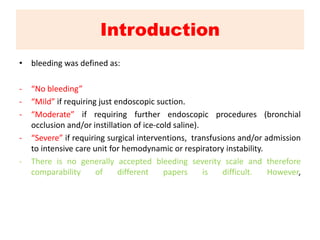
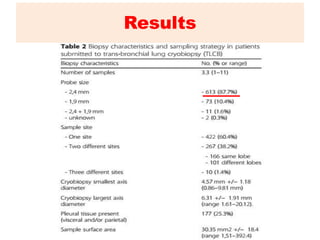
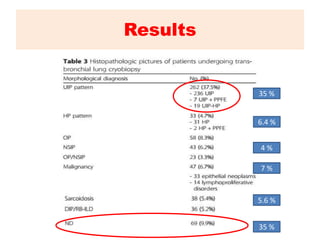
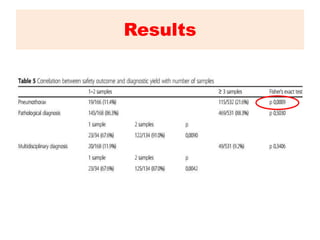
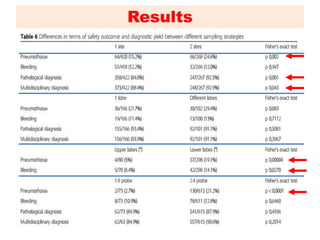
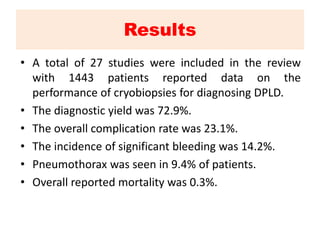
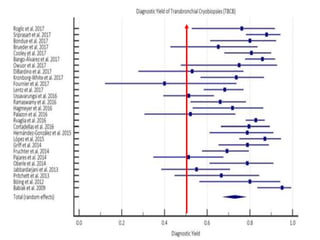
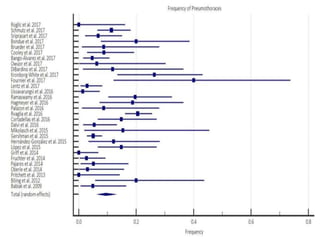
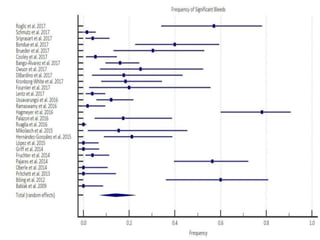
2) Results from studies show the diagnostic yield of cryobiopsy is around 73% with an overall complication rate of 23%, including pneumothorax in 9.4% of patients and significant bleeding in 14.2%.
3) Guidelines now recommend considering cryobiopsy for suspected idiopathic pulmonary fibrosis when a multidisciplinary team reviews clinical, radiological, and pathological findings.