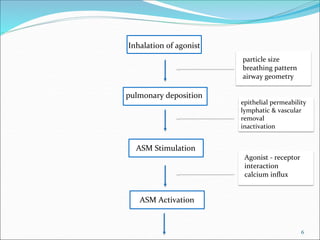
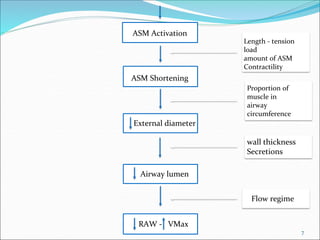
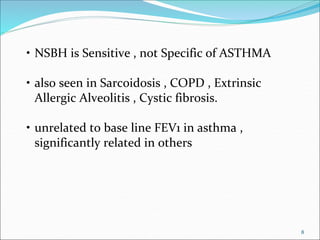
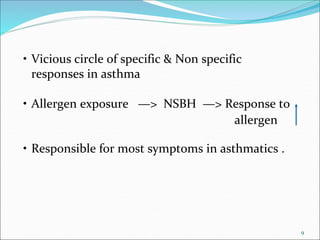
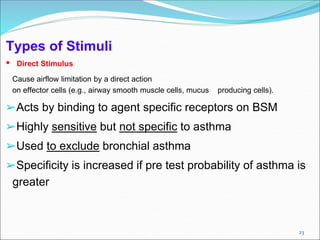
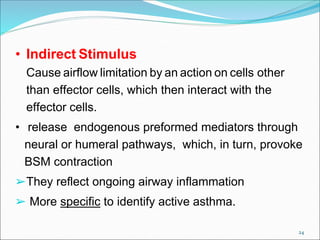
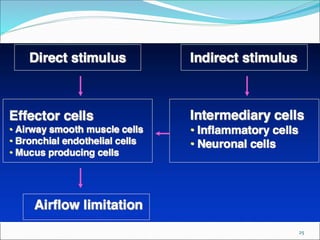
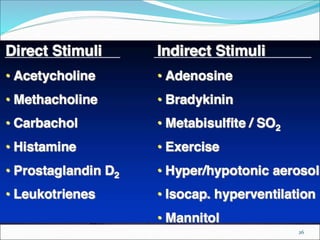
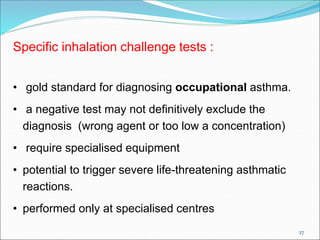
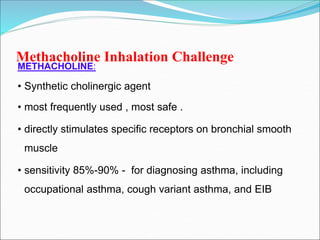
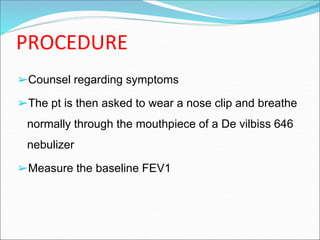
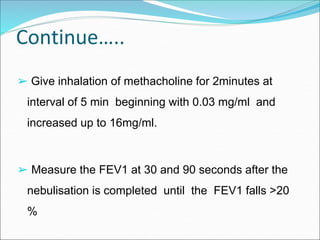
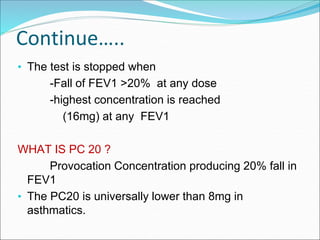
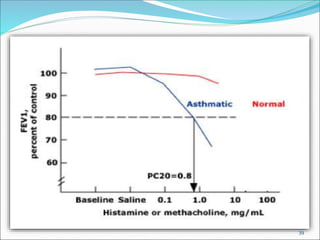
This document discusses bronchial hyperresponsiveness and bronchial provocation tests. It begins by defining asthma as a chronic inflammatory airway disease characterized by variable airflow obstruction and hyperresponsiveness to triggers. Bronchial hyperresponsiveness is an abnormal increase in airflow limitation following exposure to a stimulus and can be quantified using bronchial provocation tests. Several types of direct and indirect stimuli are described for use in bronchial provocation tests, with methacholine challenge being the most commonly used direct stimulus test due to its safety and sensitivity. The document outlines the procedures, interpretations, and indications for various bronchial provocation tests.

![22
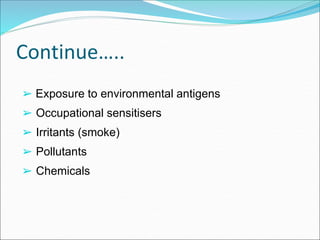
1.Specific airway irritants - Allergen , Aspirin , food
2.“direct” stimuli using nonspecific pharmacologic agents -
Methacholine
Histamine
3.“indirect” stimuli -
exercise,
eucapnic voluntary hyperventilation,
cold air hyperventilation,
hypertonic saline,
mannitol, and
adenosine monophosphate [AMP]](https://image.slidesharecdn.com/bronchoprovocationtestingppt-170511143007/85/Broncho-provocation-testing-ppt-21-320.jpg)

![51
Eucapnic Voluntary Hyperventilation
[ EVH ]
• most sensitive test for diagnosing EIB.
• patient breathes deep and fast a gas mixture of 5%
CO2 and balance room air for 6 to 8 minutes.
• A target minute ventilation is set at 30 × FEV1.
• Spirometry at 5, 10, and 20 minutes.
• A positive test is defined as a 10% reduction in FEV1.](https://image.slidesharecdn.com/bronchoprovocationtestingppt-170511143007/85/Broncho-provocation-testing-ppt-50-320.jpg)
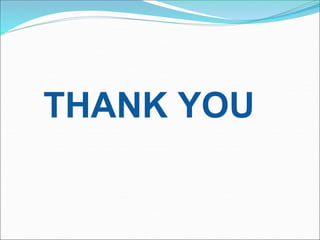
![59
REACTIVE AIRWAYS DYSFUNCTION SYNDROME
[ RADS ]
• Acute exposure to certain Gases / vapours
• producing severe bronchial / bronchiolar injury —> hyper
responsiveness & narrowing
• most cases develop in Work place
• Pathology :
- sloughing of epithelium ,
- replacement by a fibrinohemorrhagic exudate](https://image.slidesharecdn.com/bronchoprovocationtestingppt-170511143007/85/Broncho-provocation-testing-ppt-58-320.jpg)