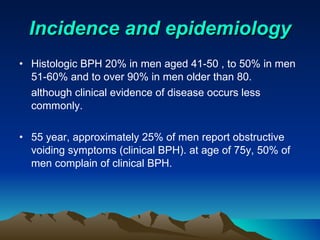
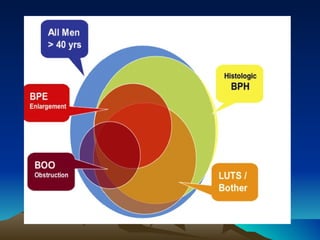
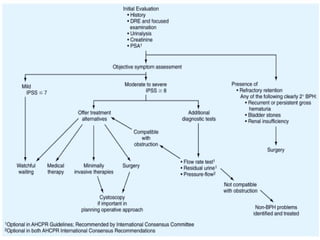
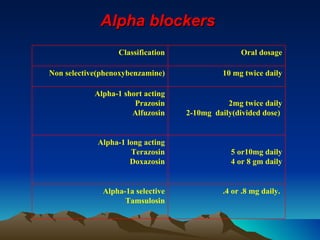
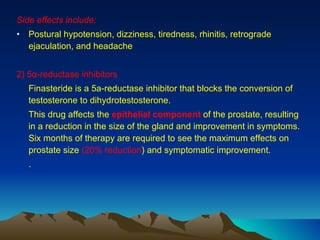
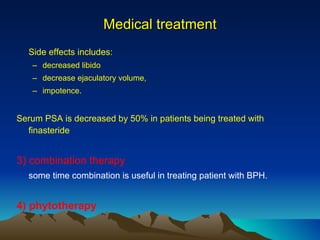
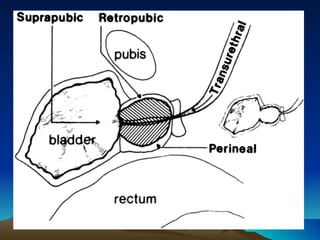
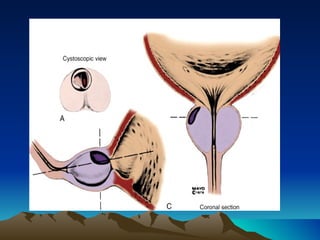
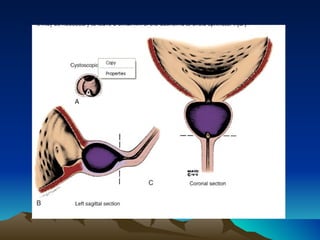
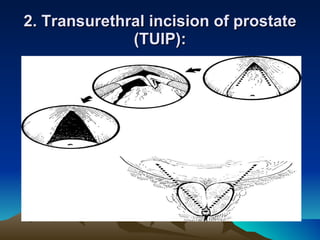
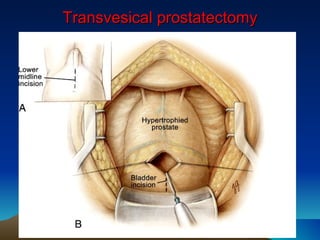
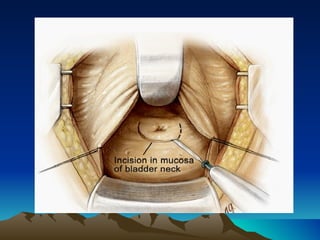
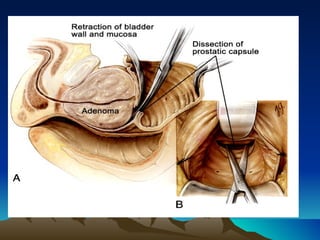
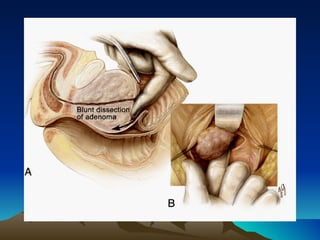
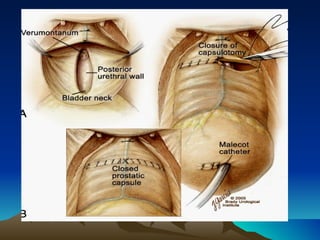
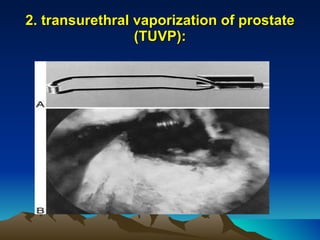
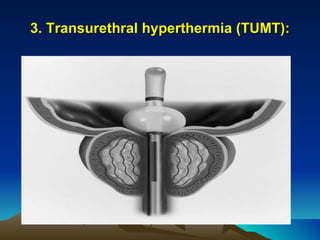
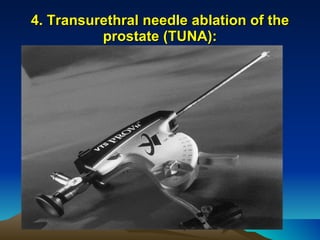
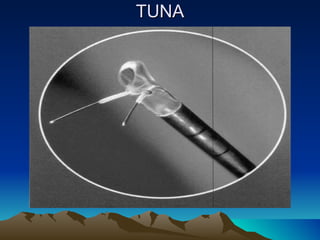
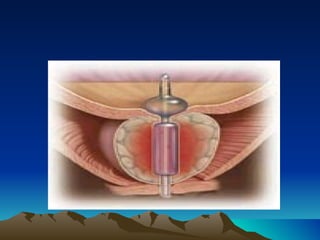
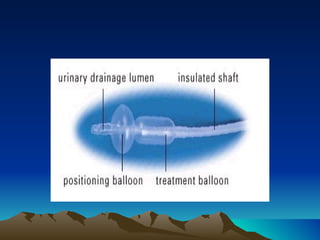
This document summarizes benign prostatic hyperplasia (BPH). It finds that the incidence of BPH increases with age, affecting 20% of men aged 41-50 and over 90% of men over 80. Risk factors include genetics and race. BPH causes both obstructive symptoms like weak urinary stream and irritative symptoms like frequent urination. Treatment options range from watchful waiting for mild cases to drug therapies like alpha blockers and 5-alpha reductase inhibitors to surgical procedures like transurethral resection of the prostate. Minimally invasive procedures also exist like laser therapy, transurethral vaporization of the prostate, and transurethral needle ablation of the prostate.