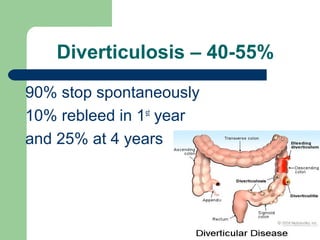
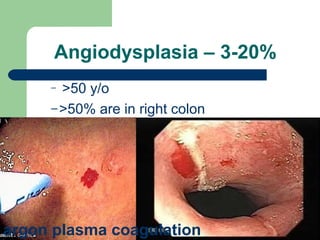
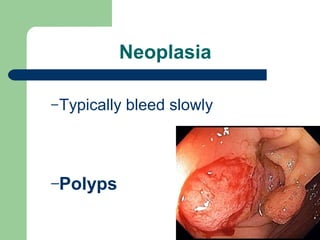
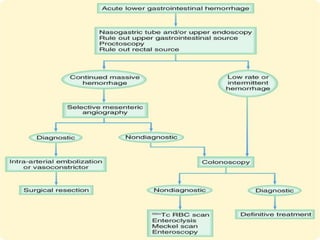
Lower GI hemorrhage can originate from the colon or small bowel. Common causes include bleeding diverticulosis, colonic angiodysplasia, and neoplasms. Evaluation involves laboratory tests, colonoscopy, video capsule endoscopy, or angiography to locate the bleeding site. Treatment options depend on the cause but may include endoscopic therapies, angiographic embolization, or surgery.