1) Surgery for hilar cholangiocarcinoma requires complex hepatic resection to obtain clear margins and provides the only chance for cure, though it is associated with significant morbidity and mortality risks.
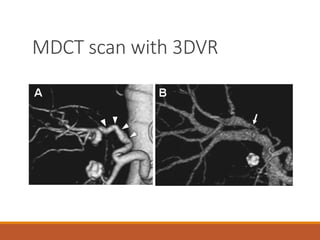
2) Pre-operative investigations including CT and MRCP are needed to determine the extent of tumor involvement and plan the appropriate type of hepatic resection.
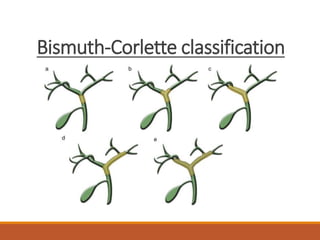
3) The extent of resection is based on the Bismuth-Corlette classification of tumor involvement and may require right, extended right, left, or extended left hepatectomy with possible arterial or portal vein resection.
4) Surgical techniques including inflow control, bile duct division, and vascular reconstruction aim to achieve an R0 resection while preserving adequate