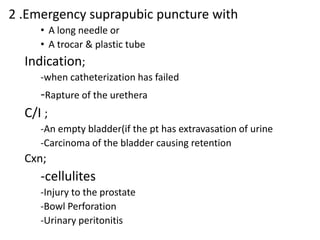
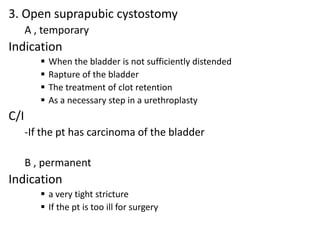
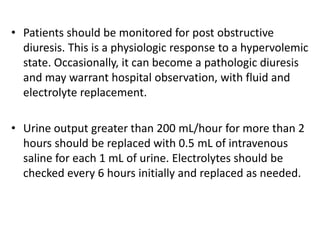
Acute urinary retention is a urologic emergency most common in older men due to benign prostatic hyperplasia. Common causes include BPH, medications, infections, and neurological disorders. Patients present with inability to pass urine and lower abdominal discomfort. Evaluation involves history, physical exam including bladder palpation, and rectal exam. Management is bladder decompression initially with Foley catheter, or emergency suprapubic puncture if catheterization fails. Patients require monitoring after decompression to watch for post-obstructive diuresis.