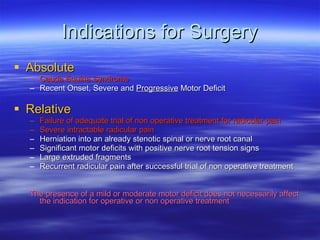
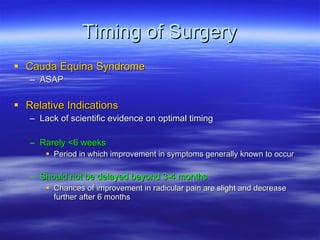
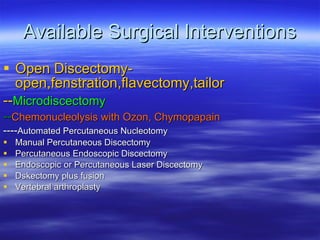
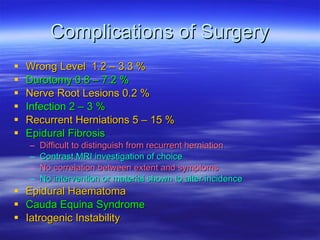
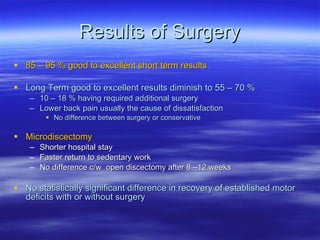
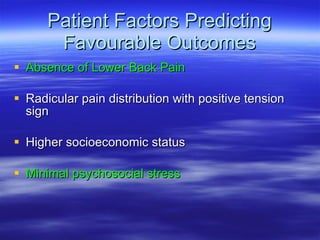
This document summarizes the surgical management of lumbar disc herniation. It outlines the absolute and relative indications for surgery, as well as the optimal timing. The available surgical interventions are listed, along with their common complications and results. Cauda equina syndrome is the absolute indication for surgery and requires immediate treatment. Relative indications include failure of conservative treatments and severe, intractable radicular pain. Open discectomy is considered the gold standard, while microdiscectomy has shorter recovery times. Patient selection influences surgical outcomes.