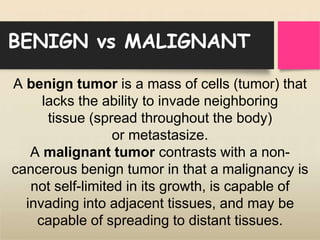
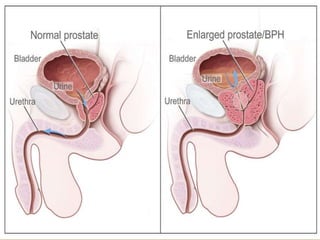
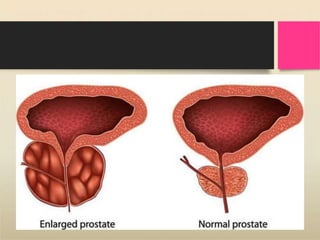
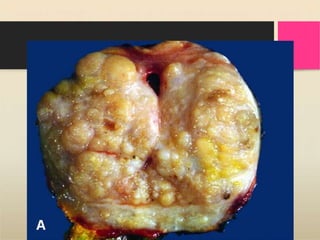
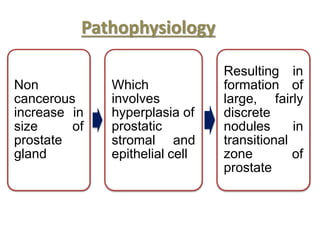
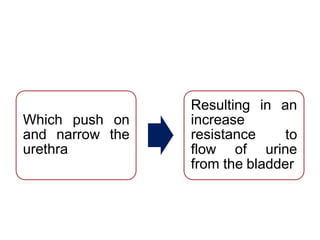
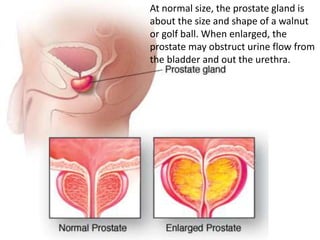
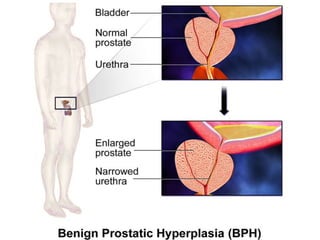
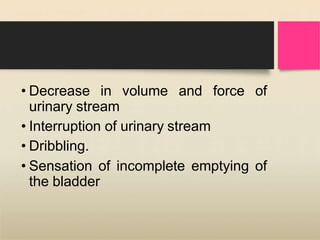
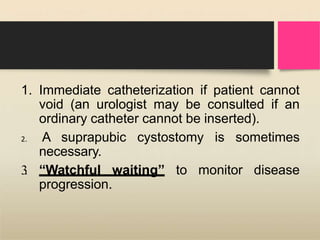
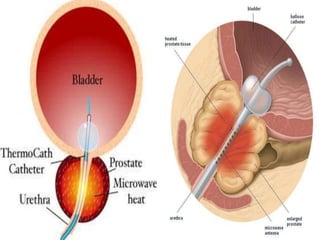
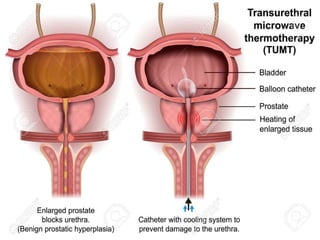
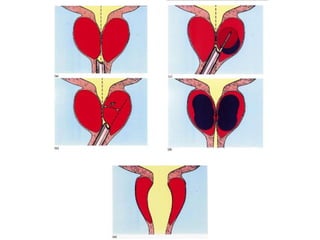
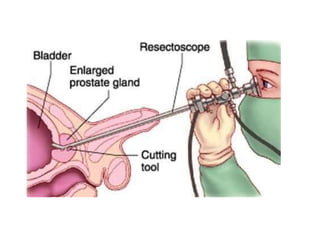
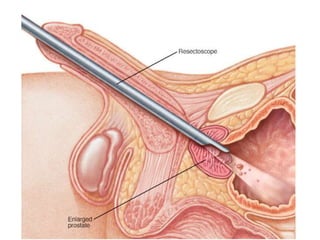
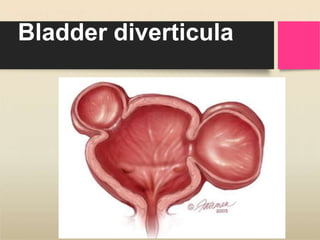
Benign prostatic hyperplasia (BPH) is a common non-cancerous enlargement of the prostate gland, primarily affecting men over 50, which can lead to urinary obstruction and symptoms such as increased frequency and urgency of urination. The cause of BPH is not entirely understood, but factors such as aging, family history, and certain health conditions may increase risk. Treatment options range from watchful waiting and medications to minimally invasive procedures and surgical interventions, depending on severity and patient circumstances.