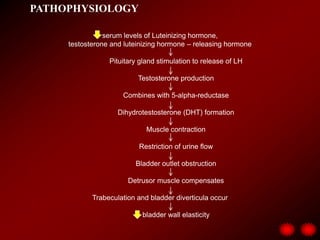
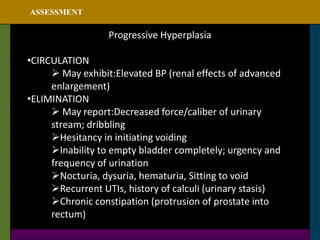
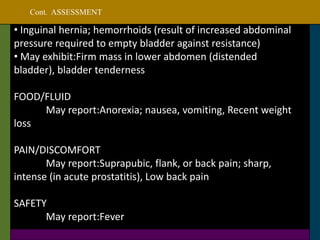
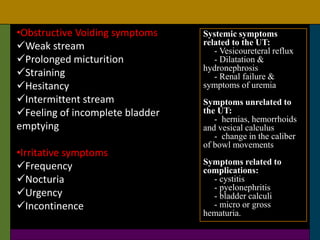
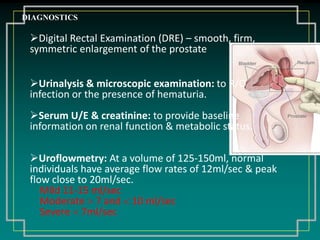
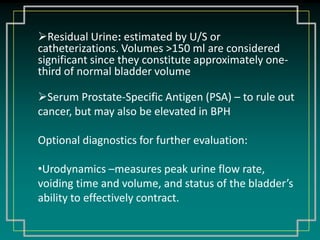
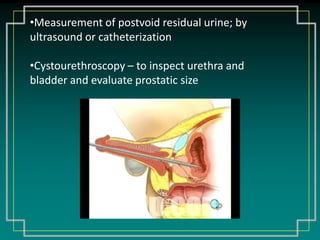
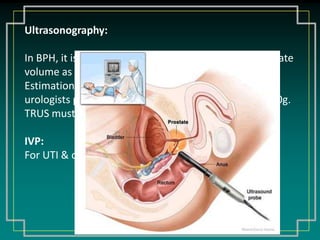
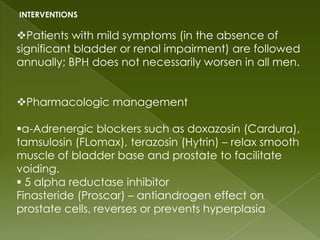
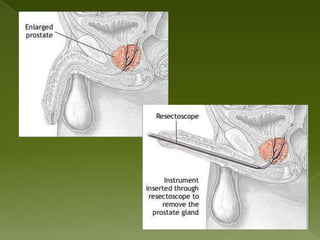
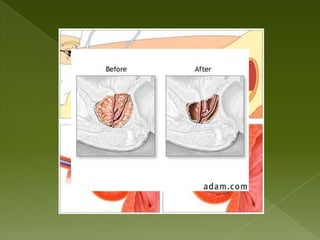
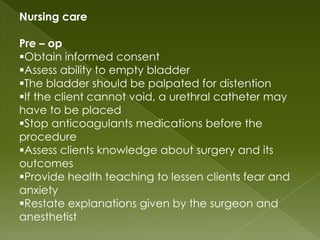
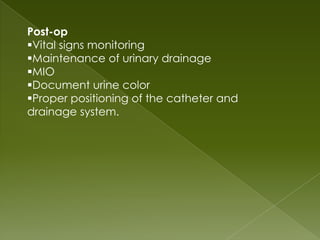
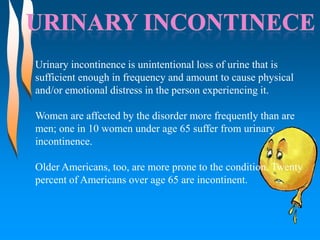
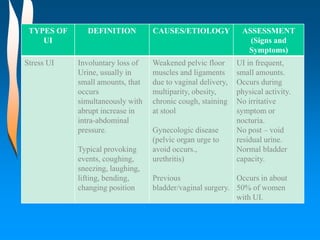
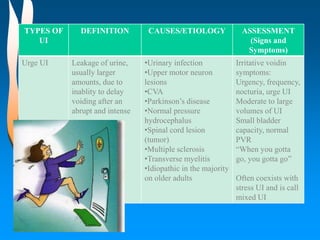
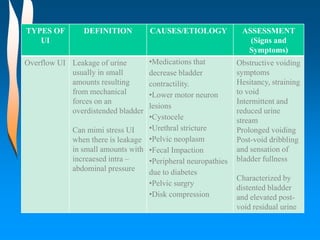
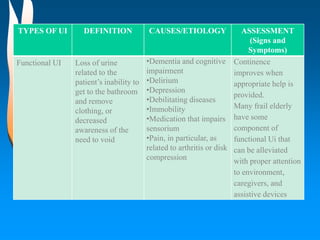
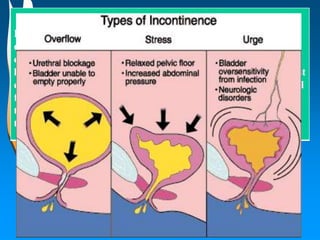
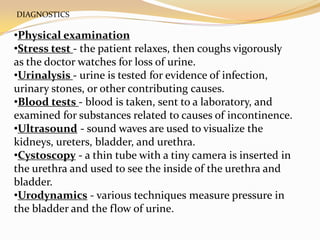
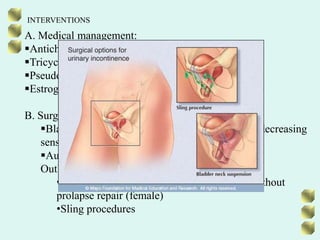
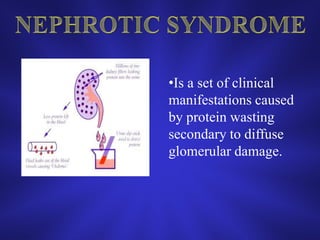
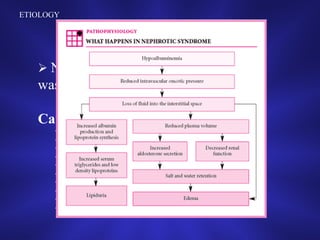
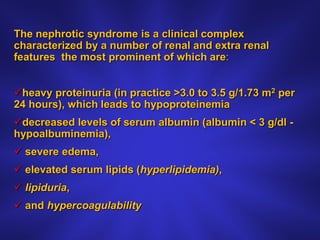
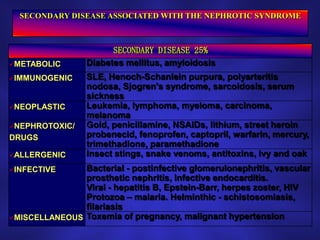
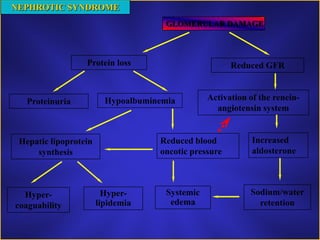
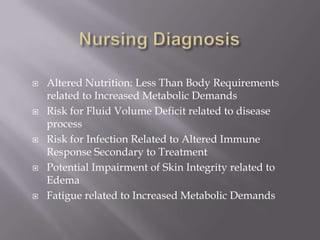
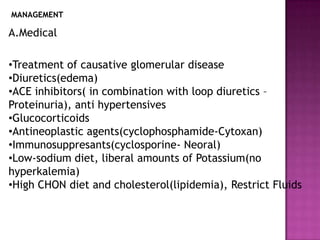
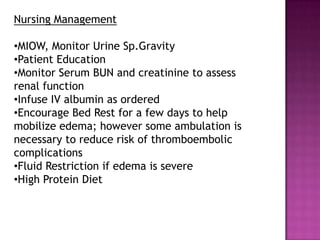
The document summarizes topics related to the renal and urinary system, including benign prostatic hypertrophy (BPH), urinary incontinence, and nephrotic syndrome. It provides details on the pathophysiology, signs and symptoms, diagnostic tests, nursing care, and interventions for BPH. Urinary incontinence is defined and its prevalence among older populations is noted. Various diagnostic tests for incontinence are also listed.