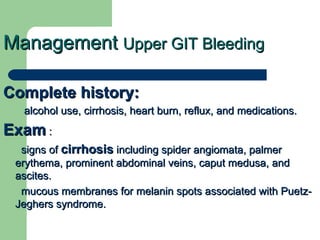
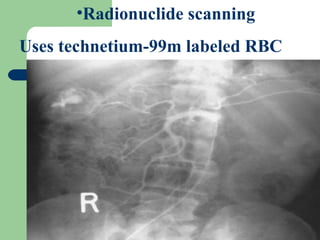
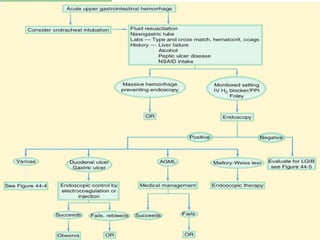
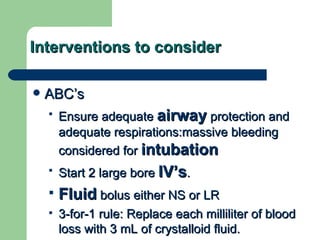
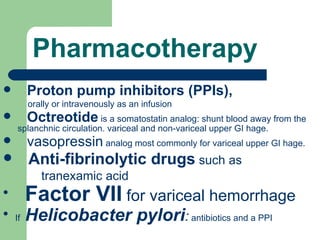
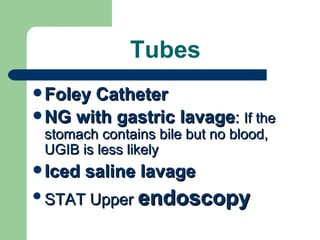
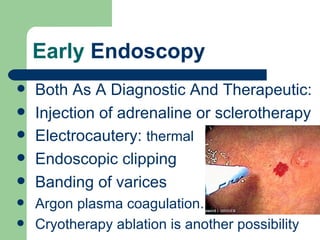
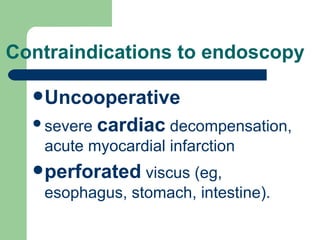
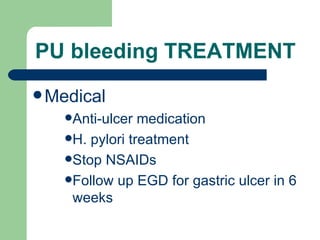
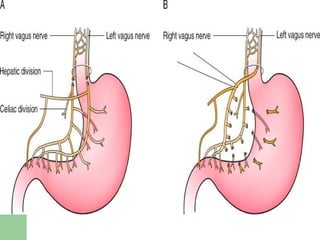
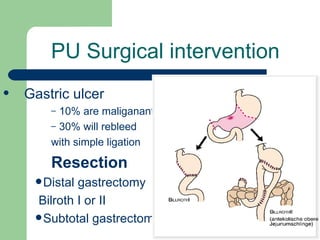
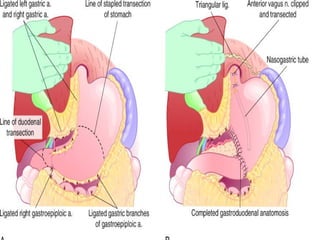
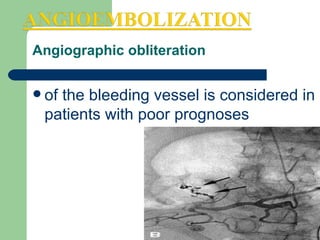
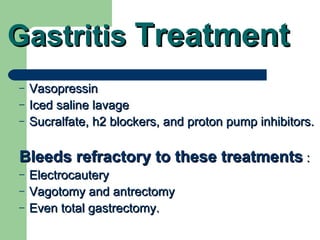
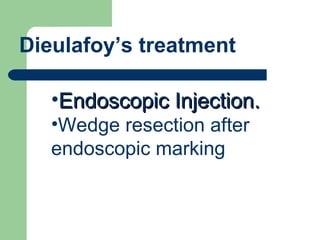
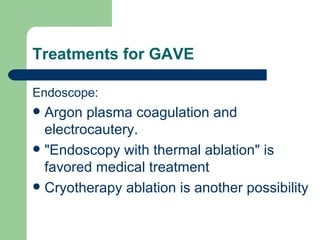
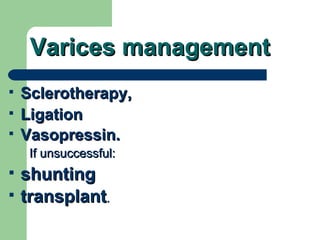
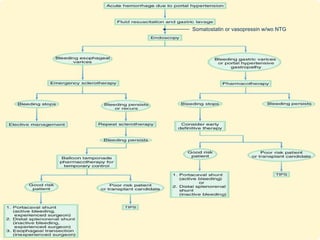
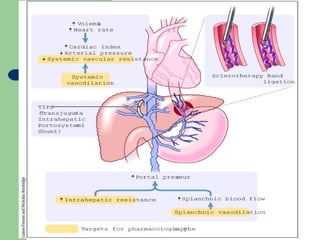
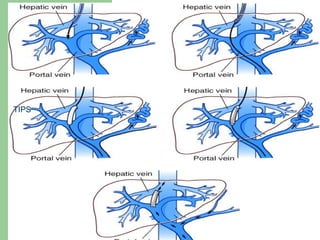
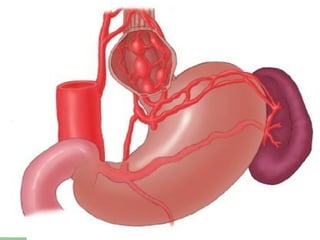
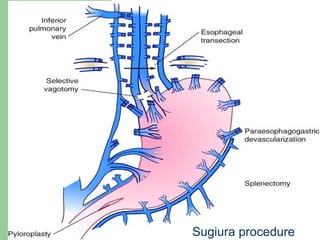
This document summarizes the management of upper GI hemorrhage. It outlines the steps to take which include obtaining a complete history and physical exam, performing laboratory tests, considering radiological scans, stabilizing the patient, identifying the source of bleeding through endoscopy, and various pharmacological and endoscopic interventions depending on the underlying cause of bleeding such as PPIs, octreotide, angiography, embolization, surgery, or TIPS procedure. Refractory cases may require repeat endoscopy, angiography, embolization or surgery.