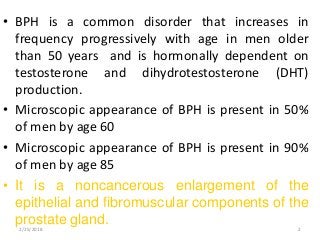
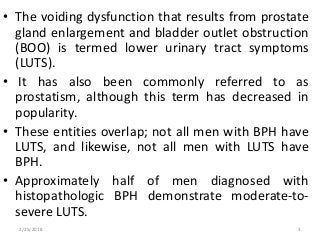
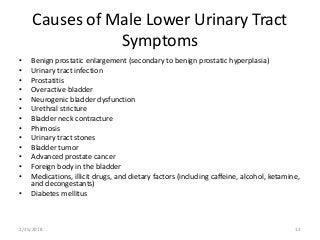
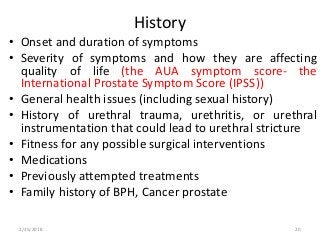
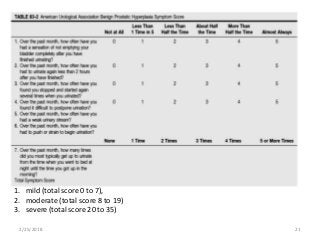
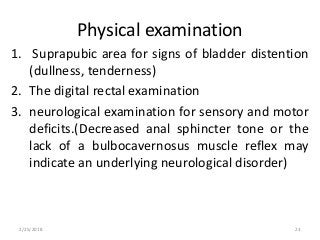
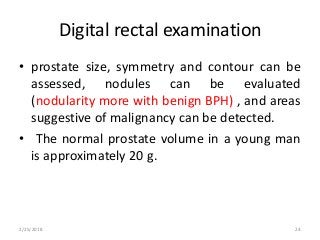
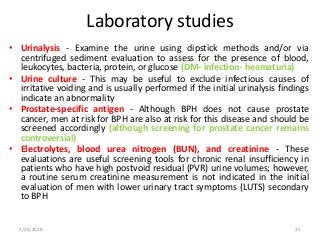
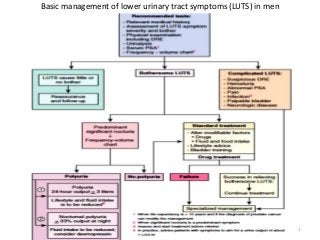
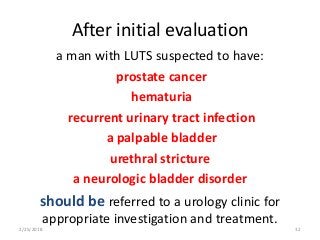
BPH is a common noncancerous enlargement of the prostate gland that increases in frequency with age in men over 50. By age 60, 50% of men will show microscopic signs of BPH, increasing to 90% by age 85. BPH causes lower urinary tract symptoms like frequent urination, weak urine stream, and incomplete emptying due to static obstruction from an enlarged prostate and dynamic obstruction from prostate smooth muscle contraction. Diagnosis involves evaluating symptoms, digital rectal exam to assess prostate size and consistency, urinalysis to rule out infection, and tests like uroflowmetry and post-void residual urine measurement to assess bladder function.
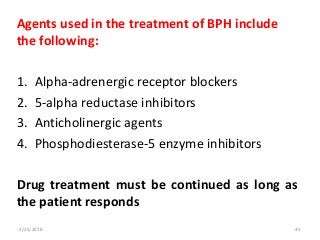
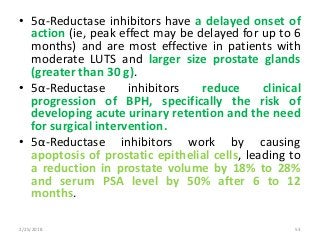
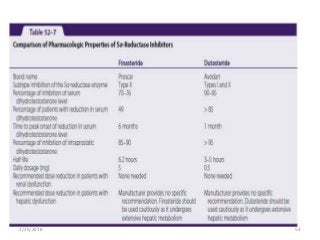
![• A minimum of 6 months is required to evaluate
the effectiveness of treatment.
• This is a disadvantage in patients with moderate
to severe symptoms, as it will take that long to
determine whether the drug is or is not effective.
• Unlike α-adrenergic antagonists, 5α-reductase
inhibitors are used to prevent BPH related
complications and disease progression.
Finasteride has been shown to reduce both the
incidence of acute urinary retention by 57% and
the need for prostate surgery by 55% in patients
with significantly enlarged prostate glands
(greater than 40 g)]
2/25/2018 55](https://image.slidesharecdn.com/bph-180224221729/85/BENIGN-PROSTATIC-HYPERPLASIA-55-320.jpg?cb=1676624639)