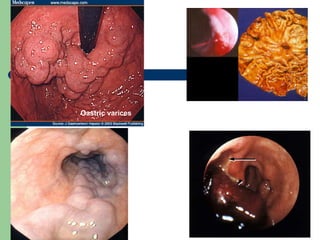
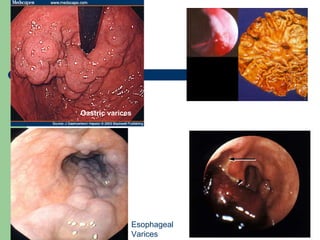
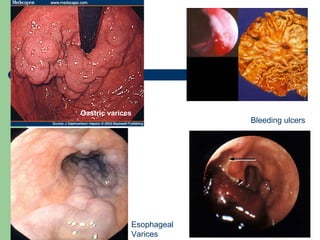
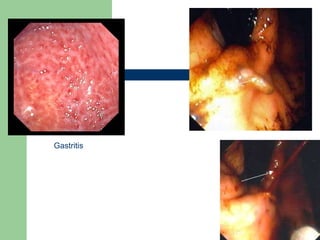
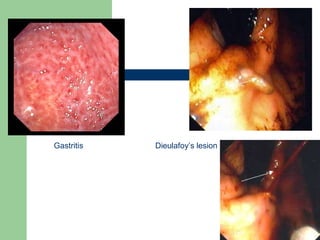
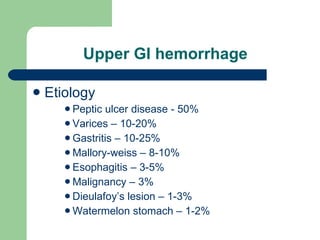
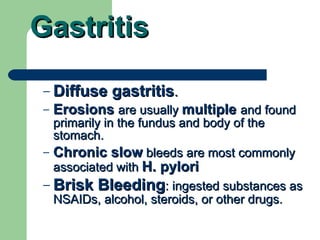
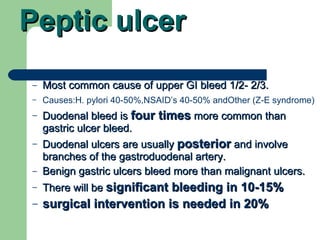
- Gastrointestinal hemorrhage is a common medical problem, accounting for 1-2% of hospital admissions. The most common causes are peptic ulcer disease (50%), esophageal varices (10-20%), and gastritis (10-25%).
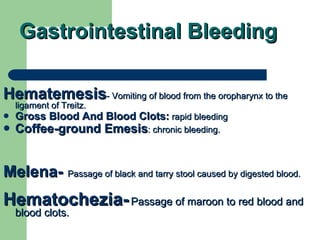
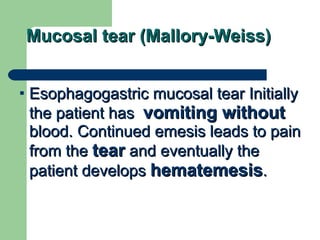
- Symptoms depend on the location of bleeding in the GI tract. Upper GI bleeding causes vomiting blood (hematemesis) or black tarry stools (melena), while lower GI bleeding causes maroon or red blood in stool (hematochezia).
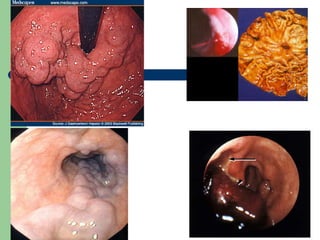
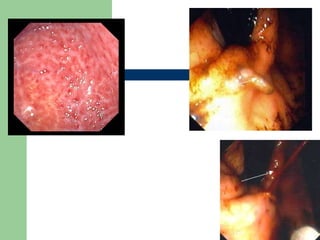
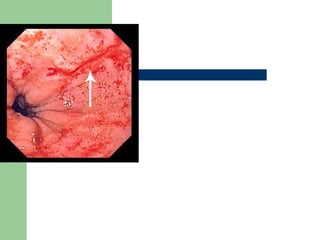
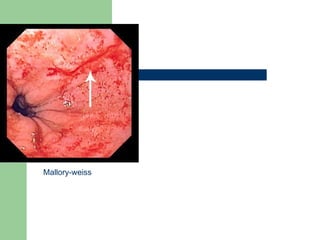
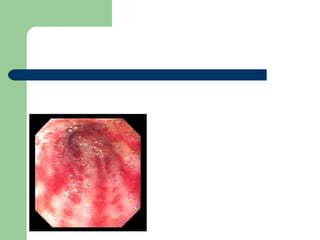
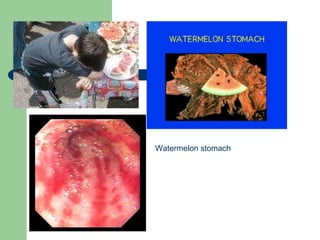
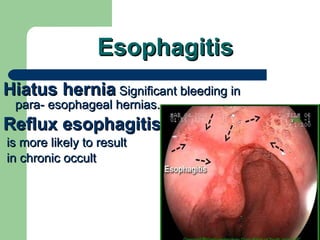
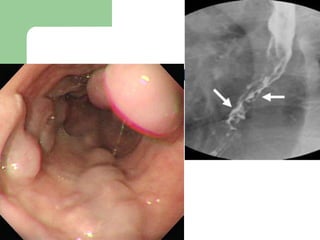
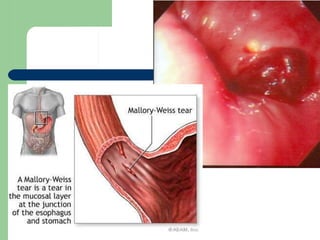
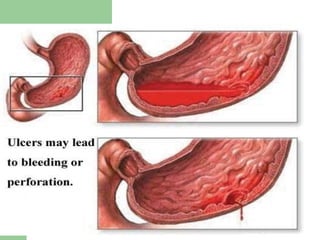
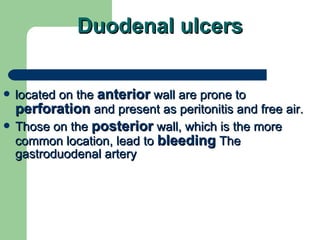
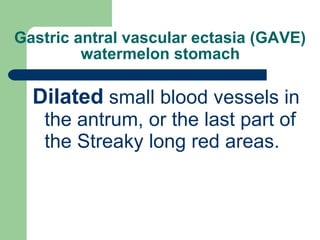
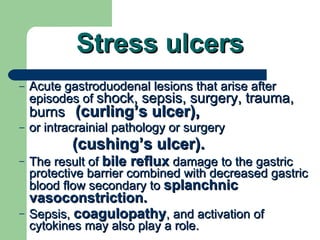
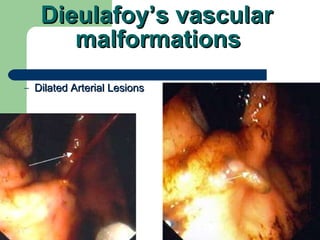
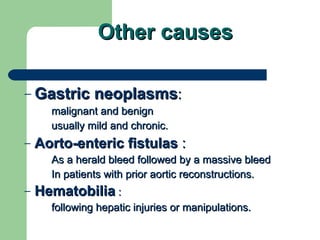
- Common etiologies include peptic ulcers, esophageal/gastric varices, gastritis, Mallory-Weiss tears, watermelon stomach, and Die