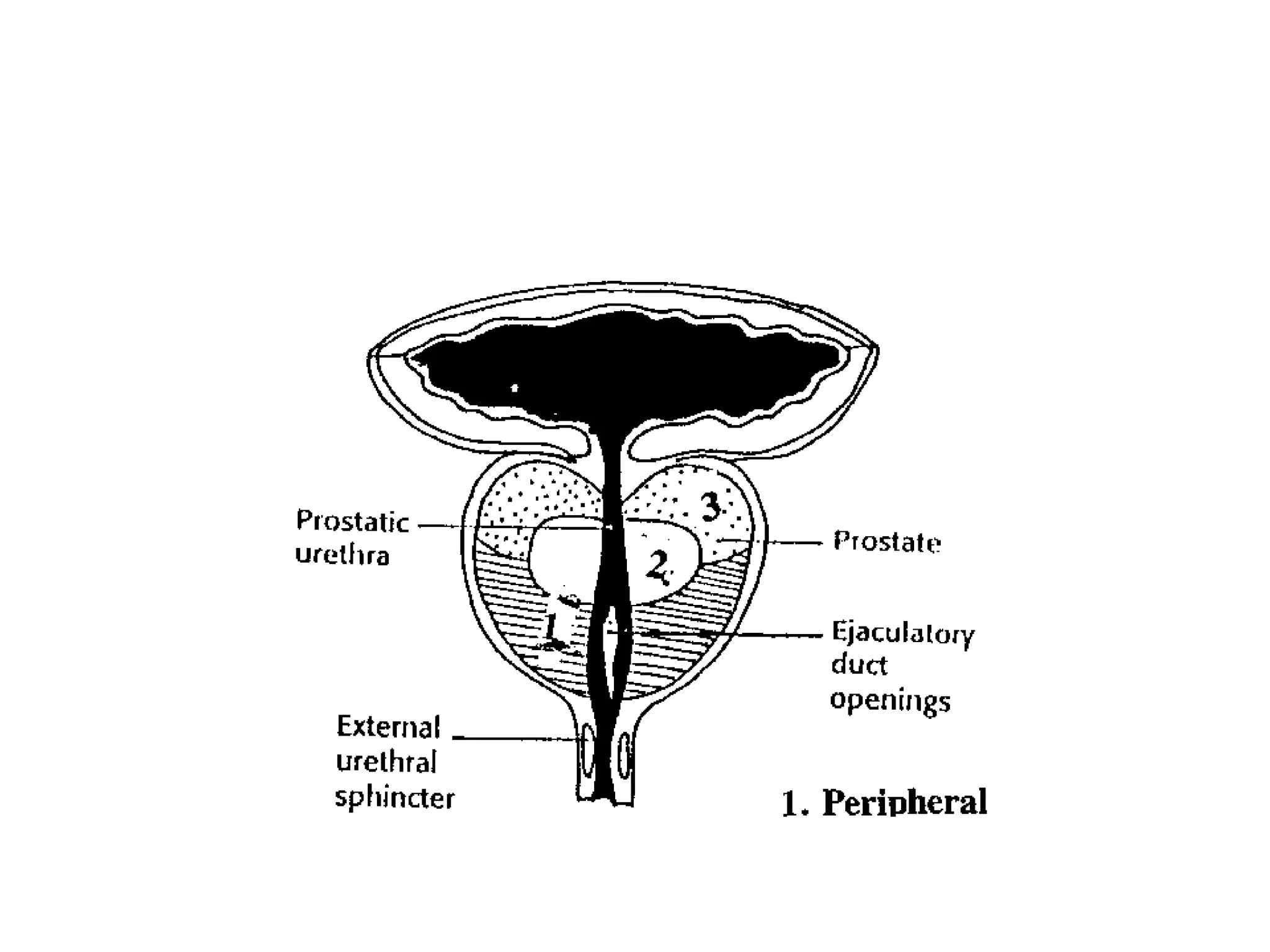
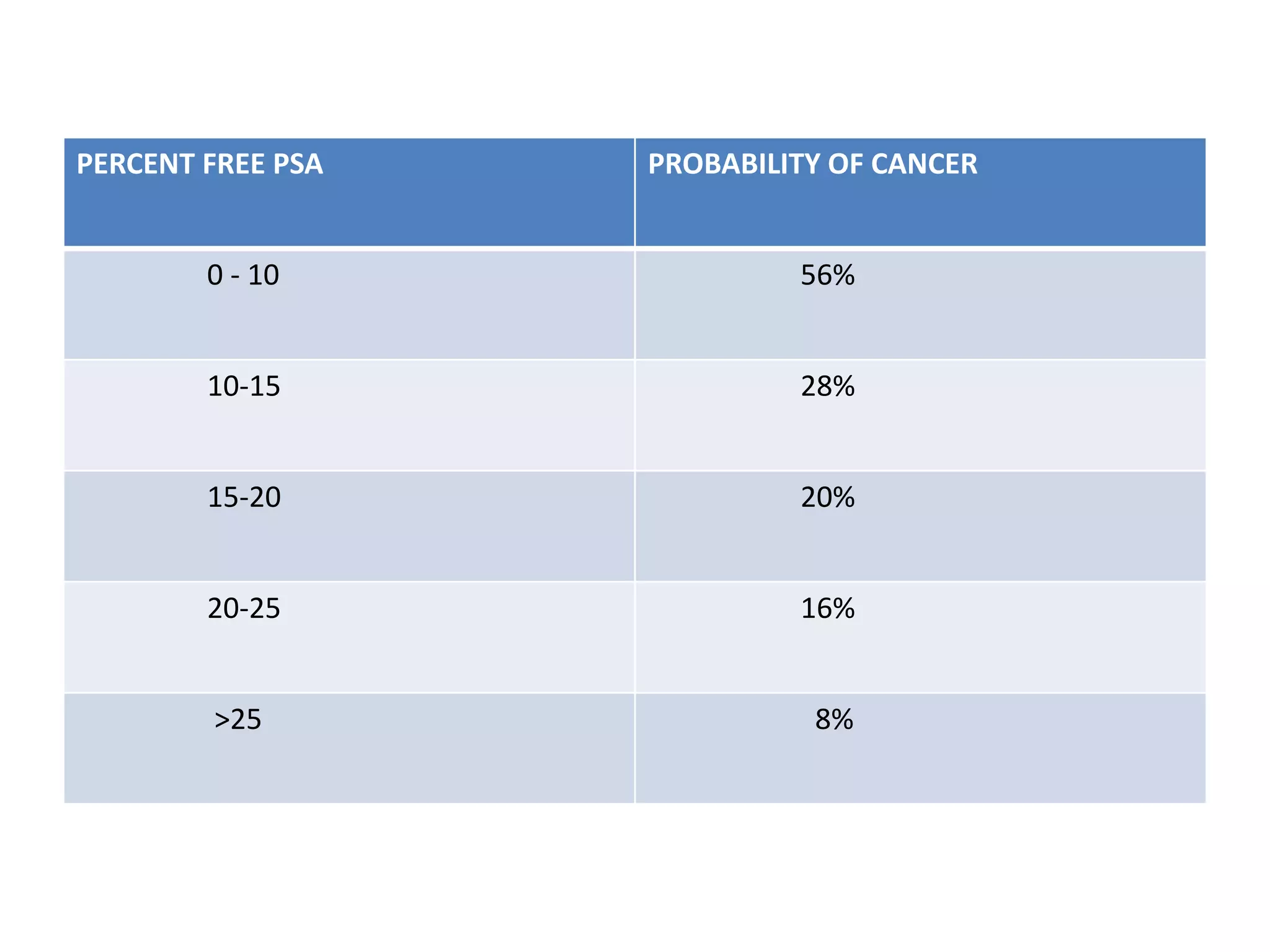
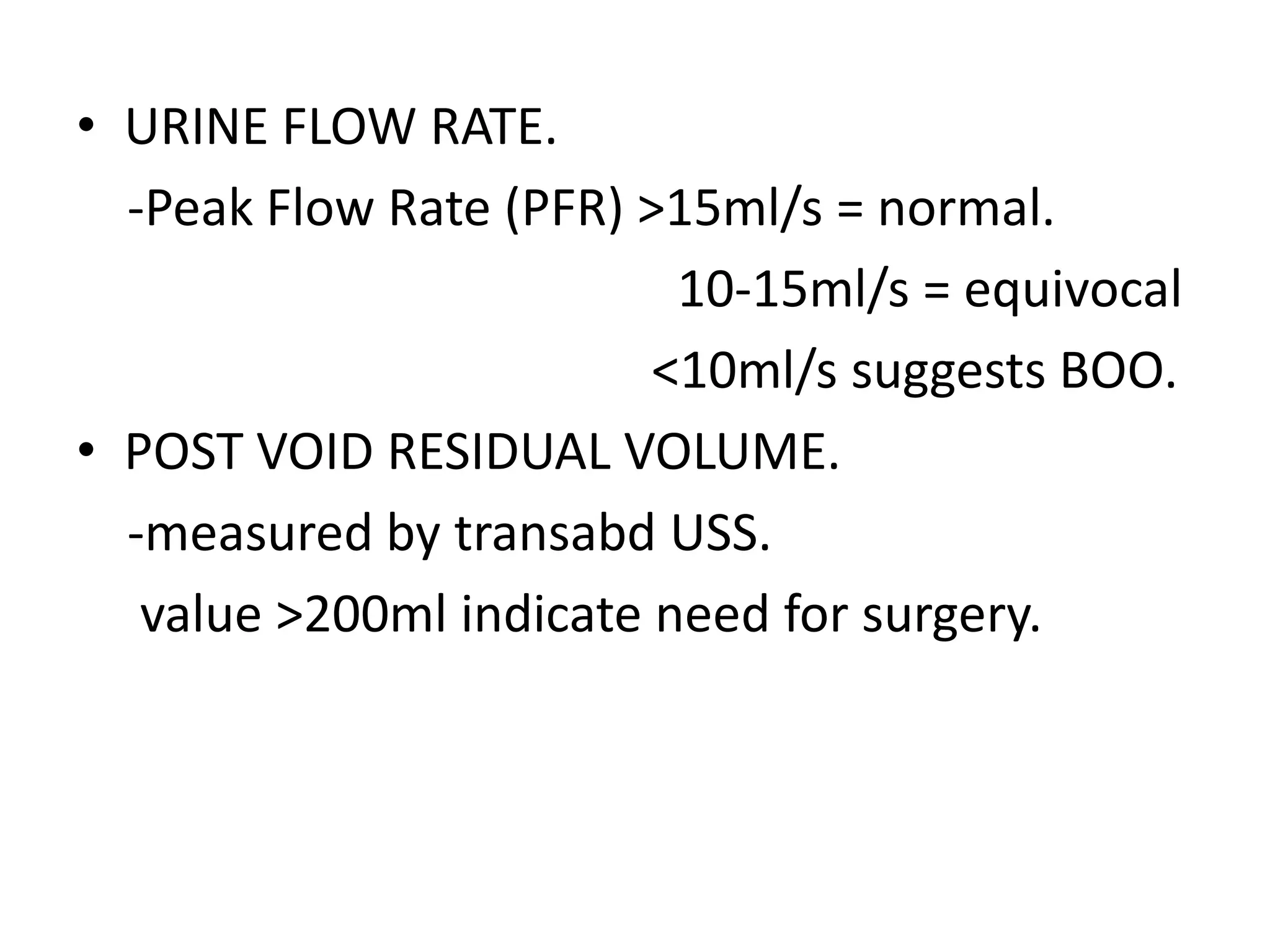
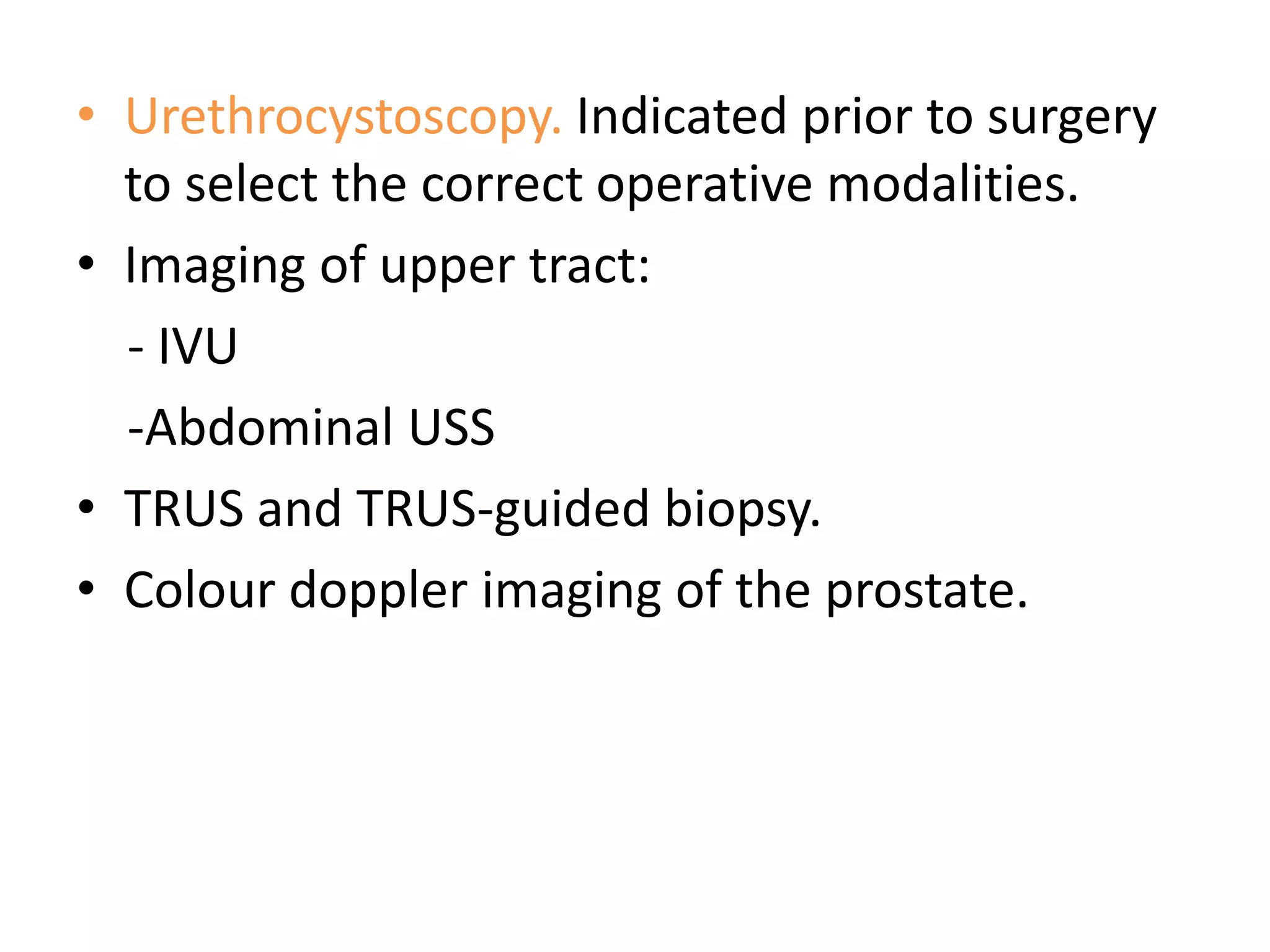
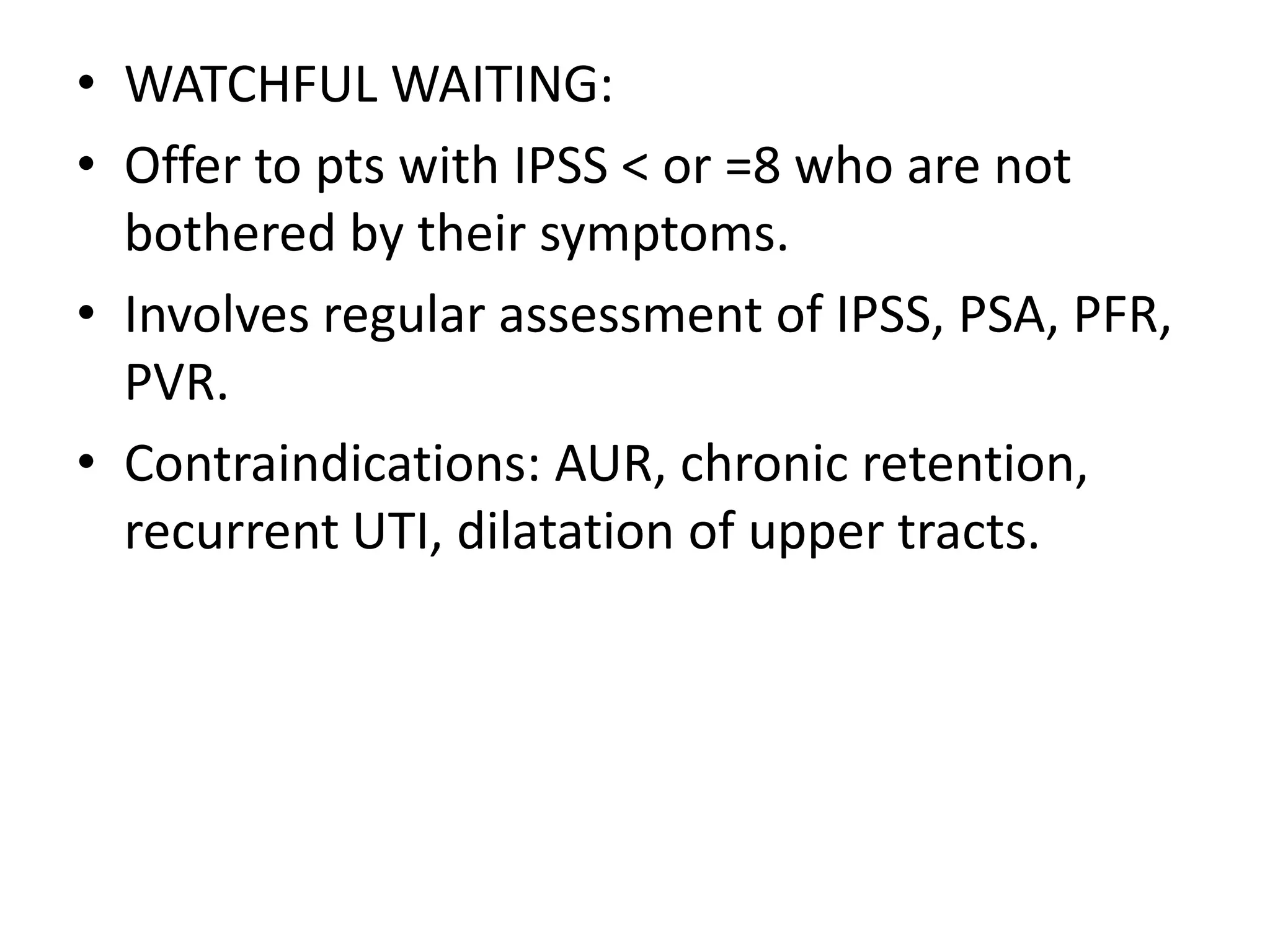
This document provides an overview of benign prostatic hyperplasia (BPH), including its anatomy, epidemiology, pathophysiology, clinical features, diagnosis, investigations, and treatment options. It discusses the relevant anatomy of the prostate and zones of the prostate involved in BPH. It also outlines guidelines for diagnosis, potential investigations including prostate-specific antigen testing, and treatment modalities including watchful waiting, medical therapy, minimally invasive procedures, and surgical options like transurethral resection of the prostate. Complications of treatments are also summarized.