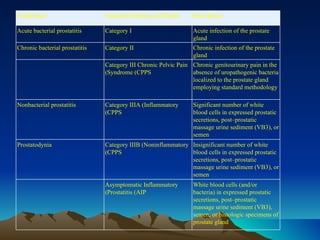
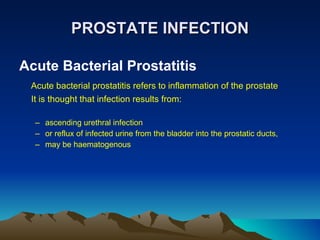
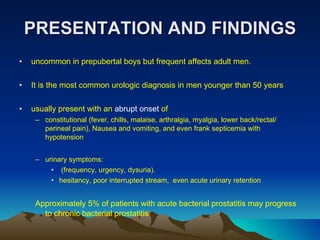
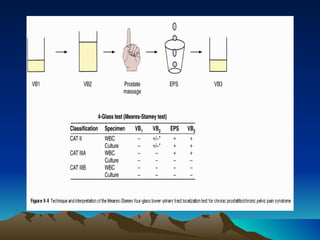
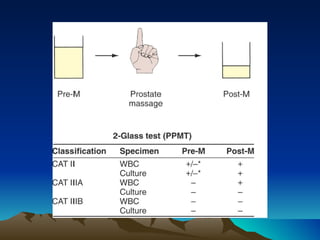
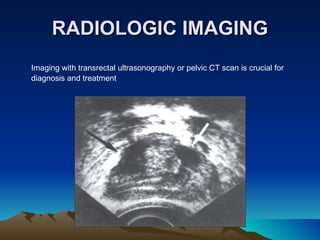
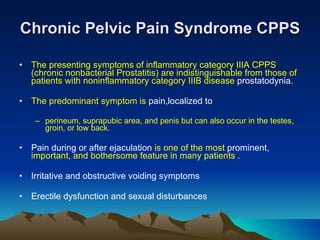
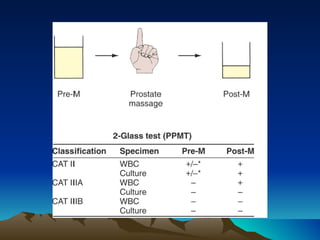
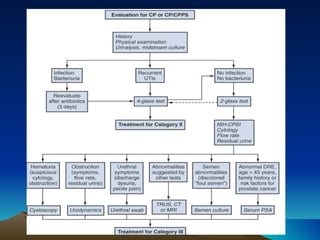
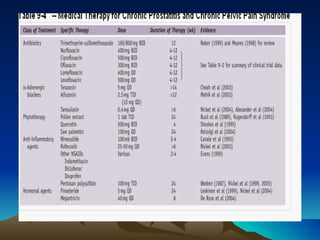
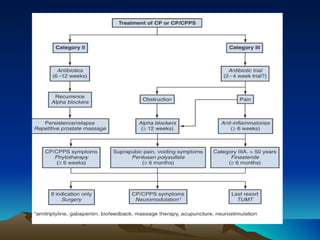
This document discusses different types of prostatitis, including acute bacterial prostatitis, chronic bacterial prostatitis, chronic pelvic pain syndrome, and prostate abscess. It describes the presentation, findings, diagnostic approach, and management for each condition. Chronic pelvic pain syndrome is further divided into inflammatory and noninflammatory subtypes based on cytological examination findings. While antibiotics may help certain types of prostatitis, treatment for chronic pelvic pain syndrome focuses on medications, physical therapies, and occasionally minimally invasive procedures to manage symptoms.