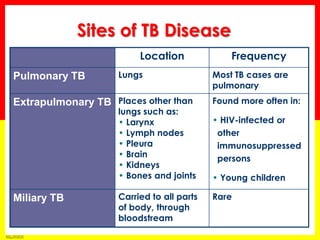
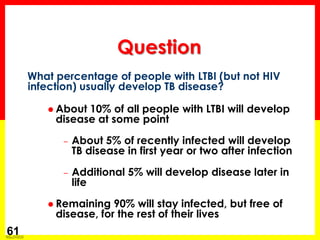
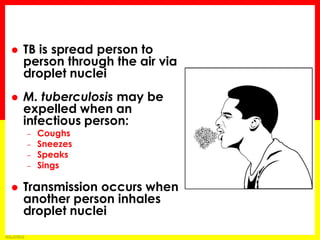
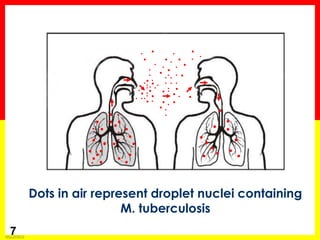
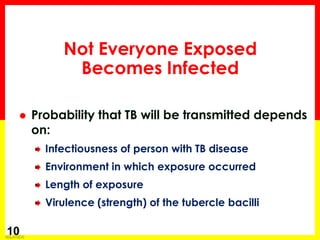
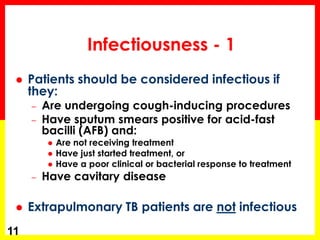
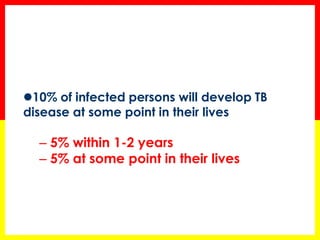
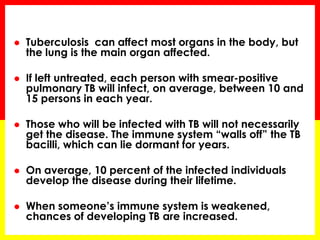
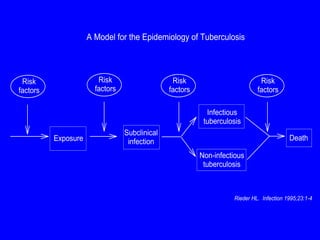
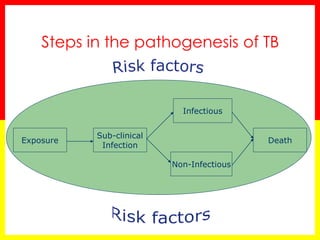
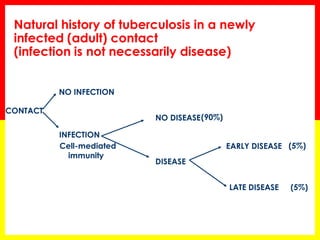
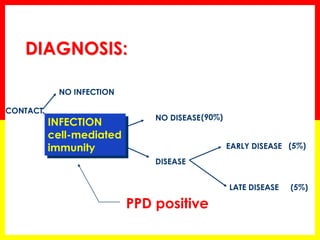
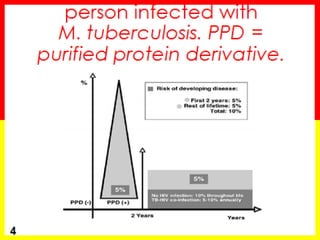
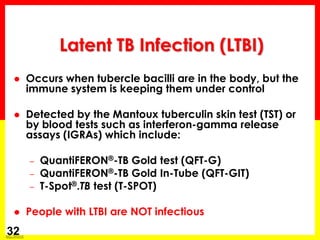
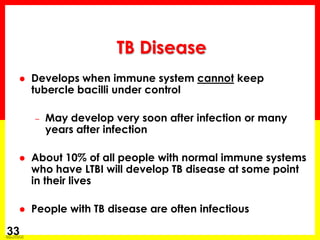
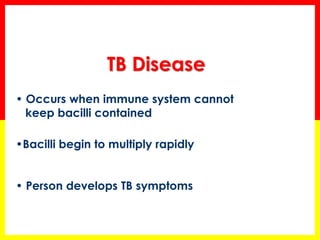
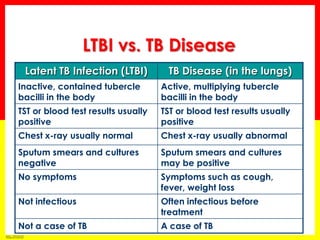
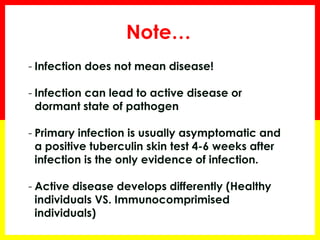
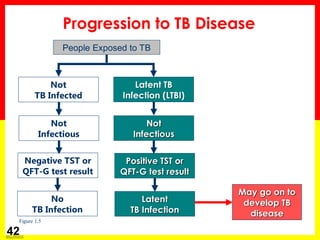
Tuberculosis is caused by infection with Mycobacterium tuberculosis bacteria, which most often affects the lungs. It spreads through the air when people who have active TB in their lungs cough, sneeze, speak, or sing. Only those with active lung infection are infectious. Most exposed people will develop latent TB infection without symptoms, but around 10% will develop active TB disease, especially if their immune system is weakened.



![Module 1 – Transmission and Pathogenesis of Tuberculosis
41
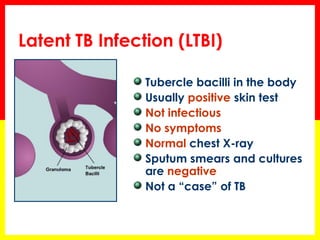
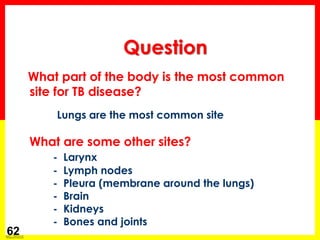
Infection with HIV
Chest x-ray findings suggestive of previous TB
Substance abuse
Recent TB infection
Prolonged therapy with corticosteroids and other immunosuppressive therapy, such as prednisone and tumor necrosis factor-alpha [TNF-α] antagonists
Organ transplant
Silicosis
Diabetes mellitus
Severe kidney disease
Certain types of cancer
Certain intestinal conditions
Low body weight
Some conditions increase probability of LTBI progressing to TB disease](https://image.slidesharecdn.com/tbtransmission-140909170305-phpapp01/85/Tb-transmission-41-320.jpg)
![Module 1 – Transmission and Pathogenesis of Tuberculosis
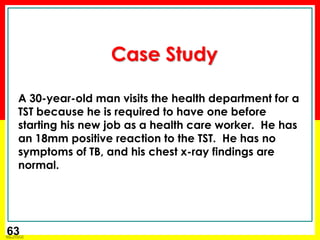
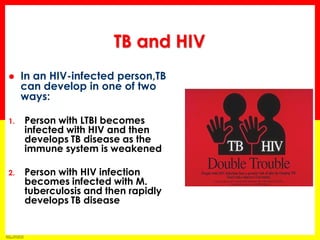
44 TB and HIV
People who are infected with both M. tuberculosis and HIV are much more likely to develop TB disease
TB infection and NO risk factors
TB infection and HIV infection
(pre-Highly Active Antiretroviral Treatment [HAART])
Risk is about 5% in the first 2 years after infection and about 10% over a lifetime
Risk is about 7% to 10% PER YEAR, a very high risk over a lifetime](https://image.slidesharecdn.com/tbtransmission-140909170305-phpapp01/85/Tb-transmission-44-320.jpg)