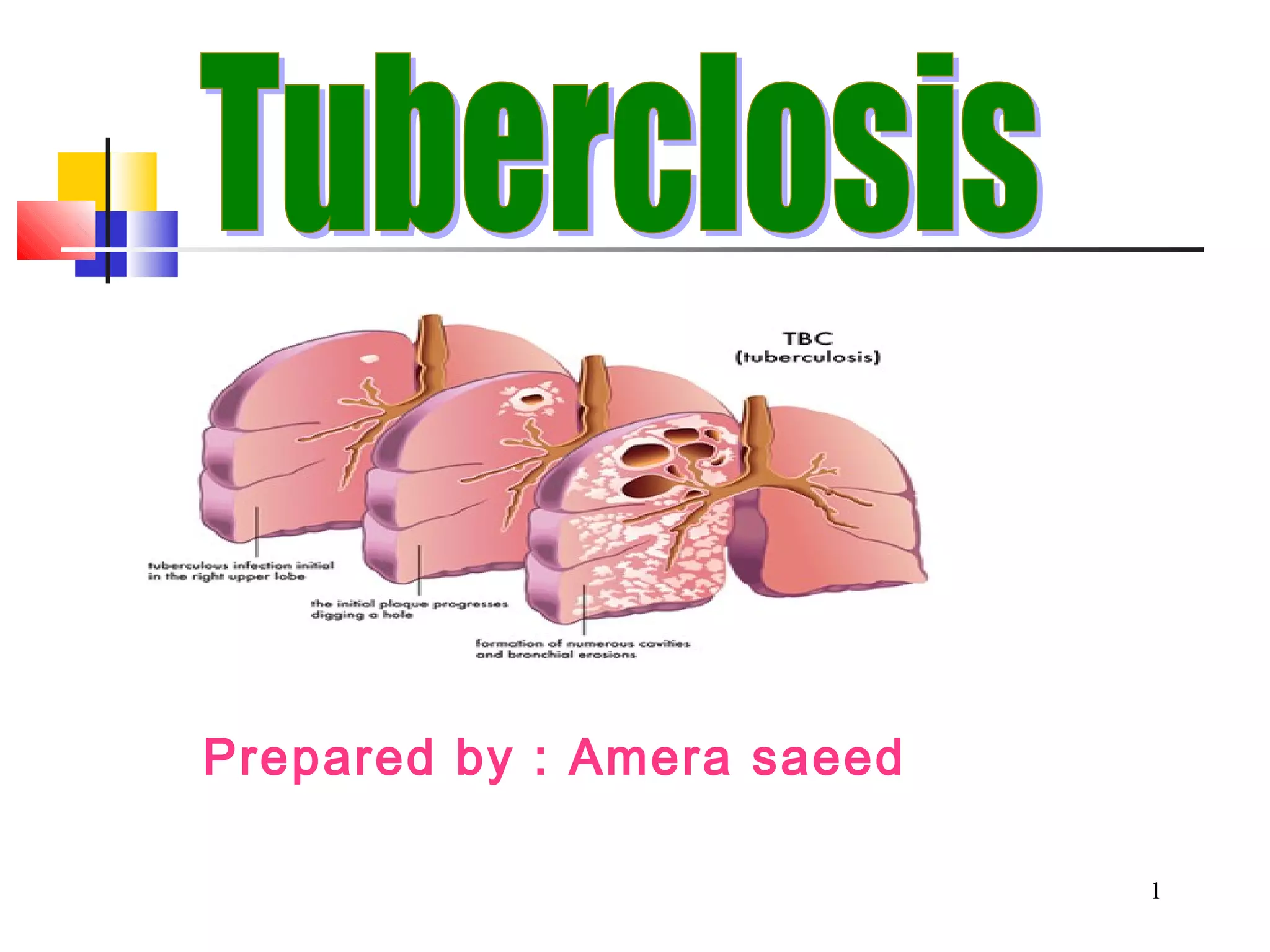
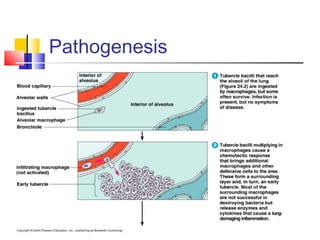
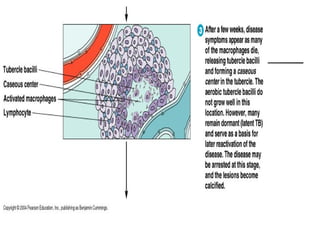
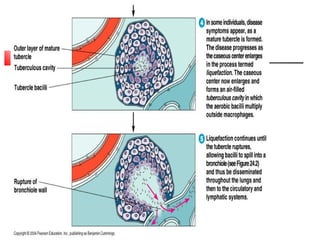
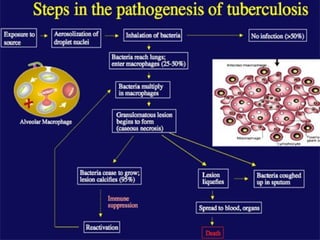
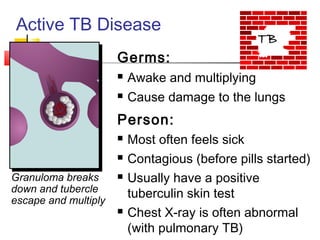
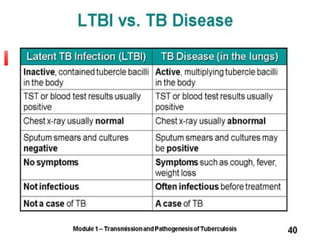
1) TB is caused by Mycobacterium tuberculosis and is one of the top infectious disease killers.
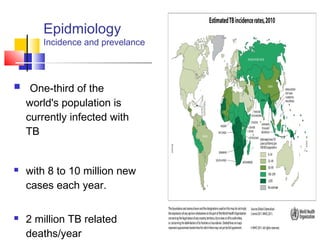
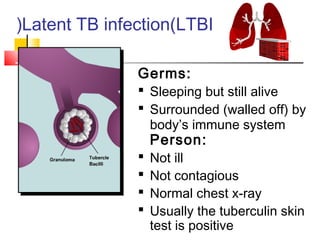
2) It is transmitted through the air and one-third of the world's population is infected with latent TB.
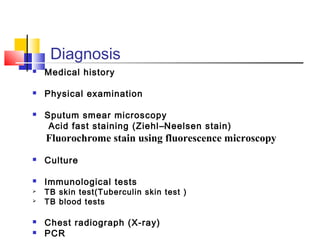
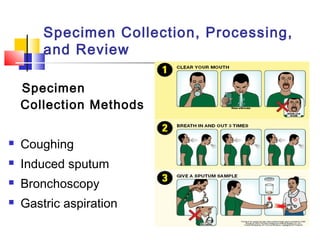
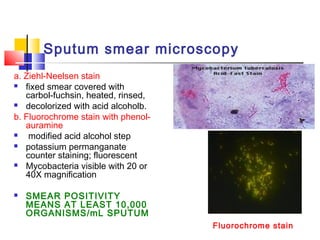
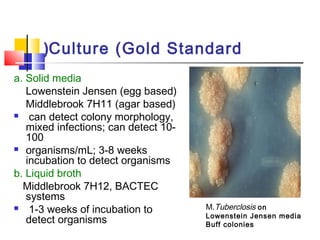
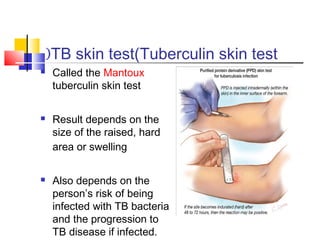
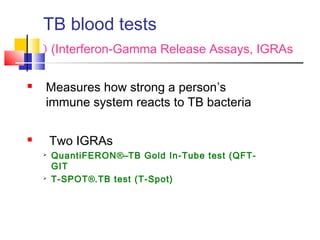
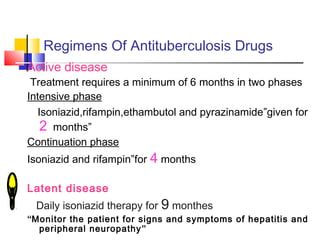
3) Diagnosis involves sputum smear microscopy, culture, tuberculin skin test, chest x-ray and PCR. Treatment requires a minimum of 6 months of multiple antibiotic drugs.

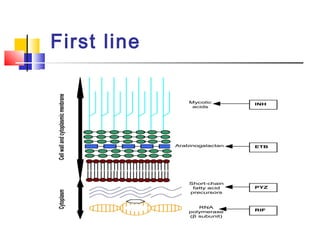
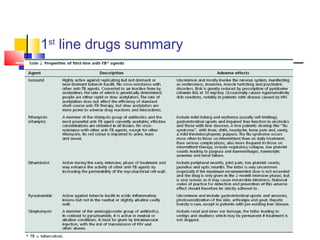
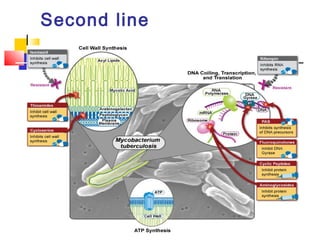
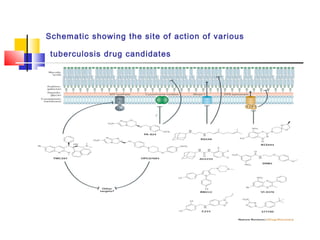
![Second line
Drug target effect
Para-amino
salicylic
acid )PAS`)
Dihydro _pteroate
synthase
Inhibits folate
biosynthesis
Ethionamide Enoyl-[acyl-carrier-
protein] reductase
Inhibits mycolic acid
biosynthesis
Ofloxacin DNA gyrase and DNA
topoisomerase Inhibits DNA
supercoiling
Kanamycin 30S ribosomal subunit Inhibits protein
synthesis
Amikacin 30S ribosomal subunit Inhibits protein
synthesis
Cycloserin d-alanine racemase and
ligase
Inhibits
peptidoglycan](https://image.slidesharecdn.com/tb-140519182851-phpapp02/85/Tuberclosis-39-320.jpg)