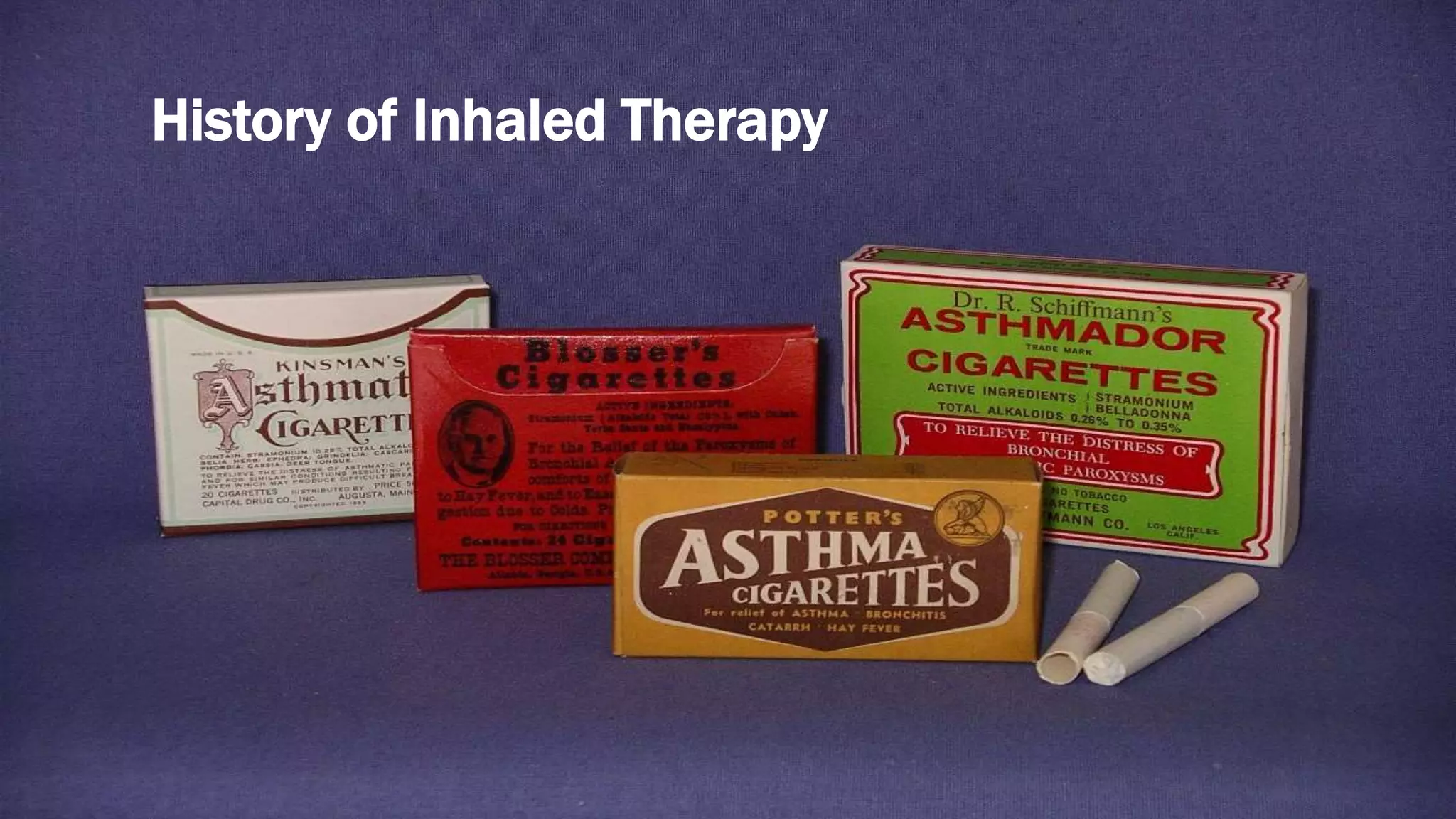
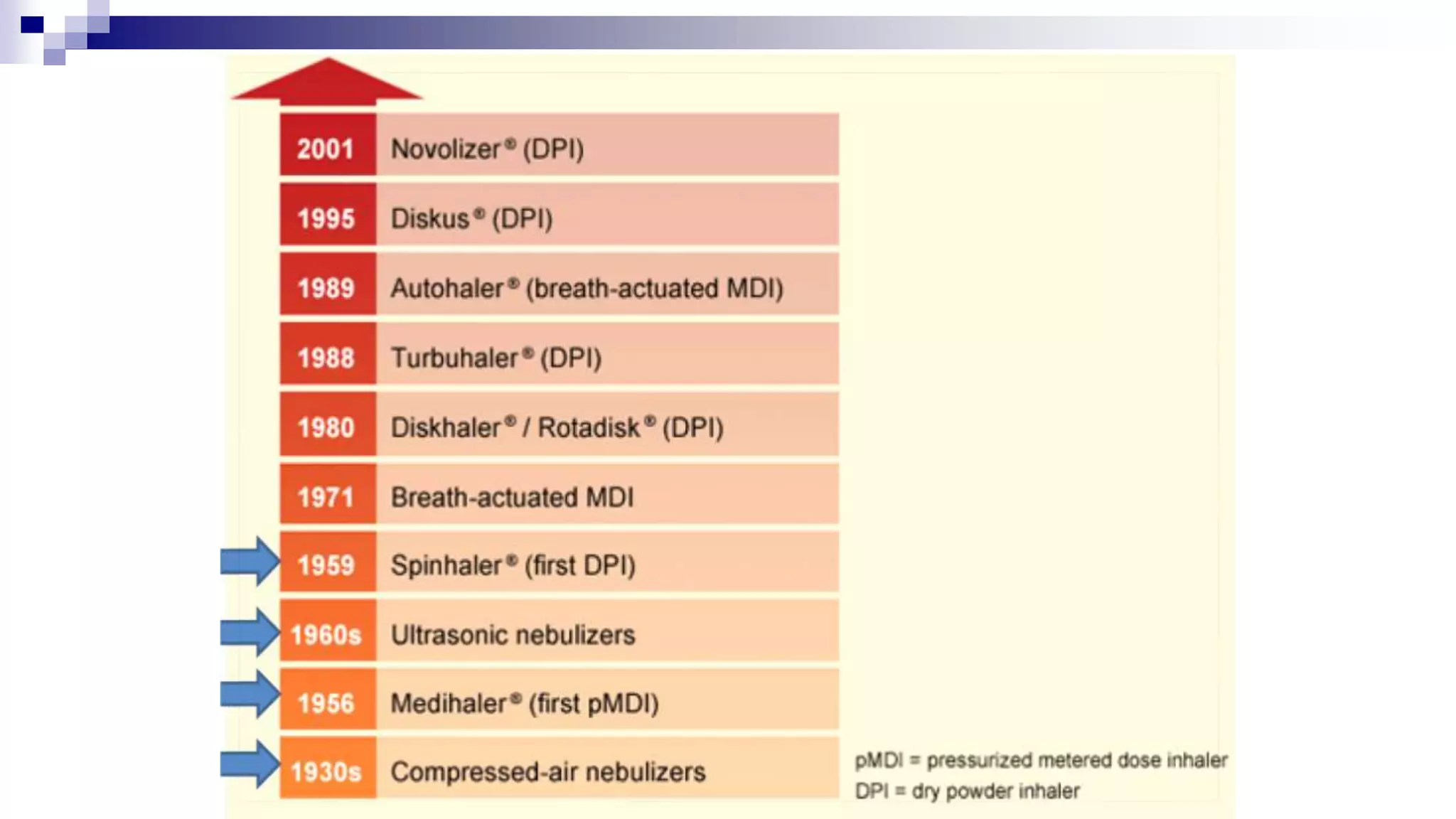
This document provides an overview of inhaled therapy for asthma. It discusses the history of inhaled treatments and different types of inhalers. The key aspects covered include:
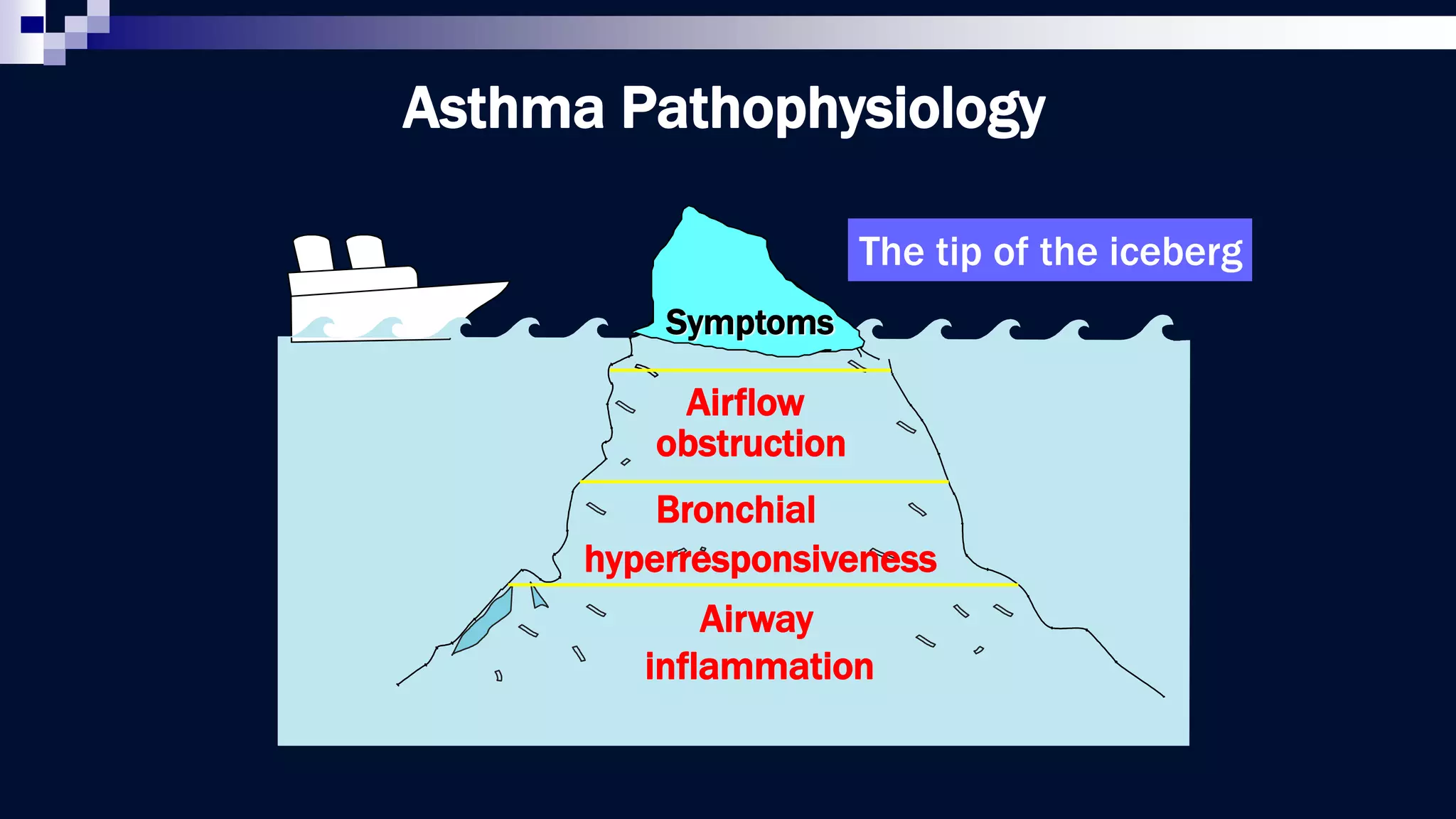
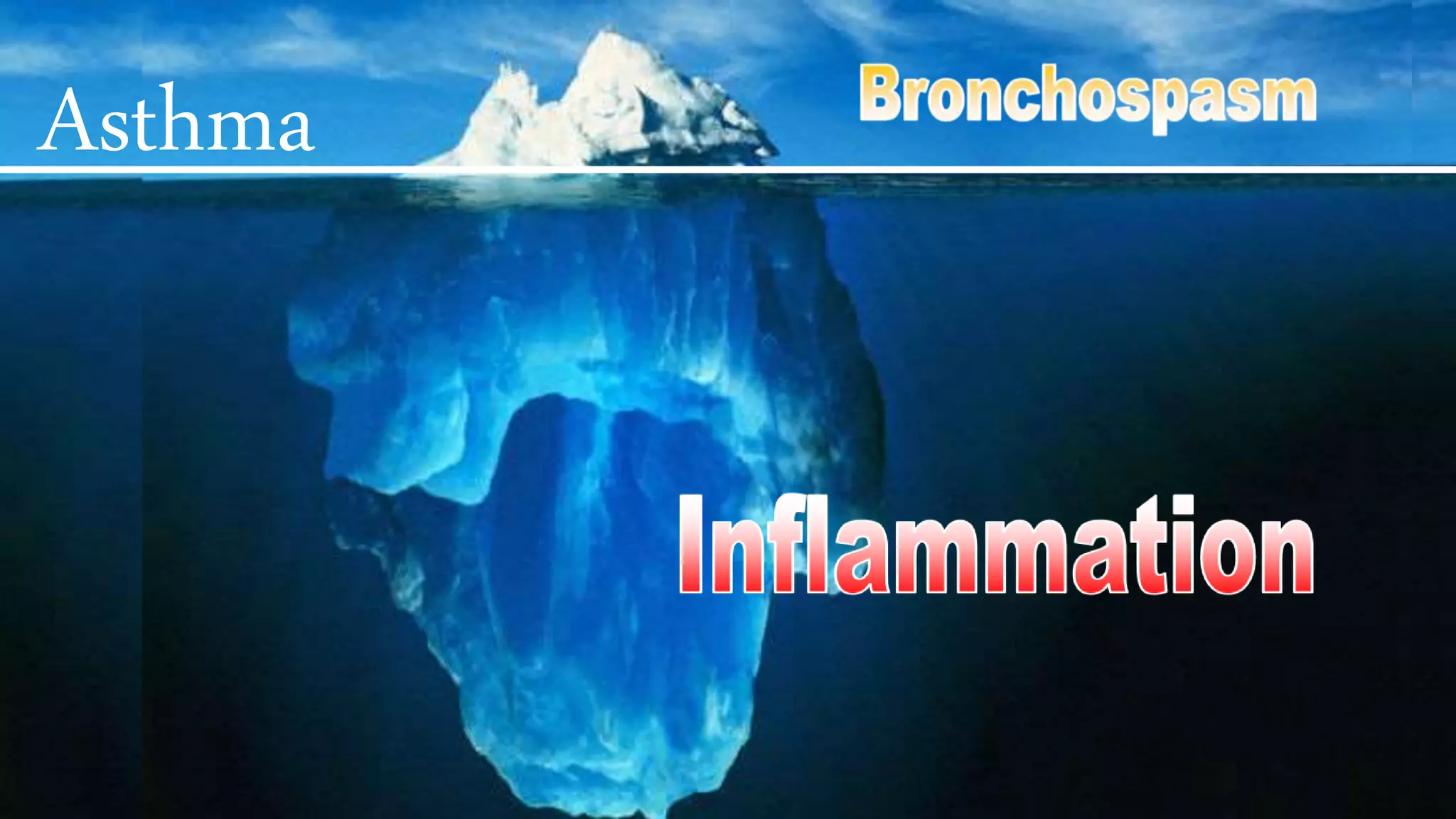
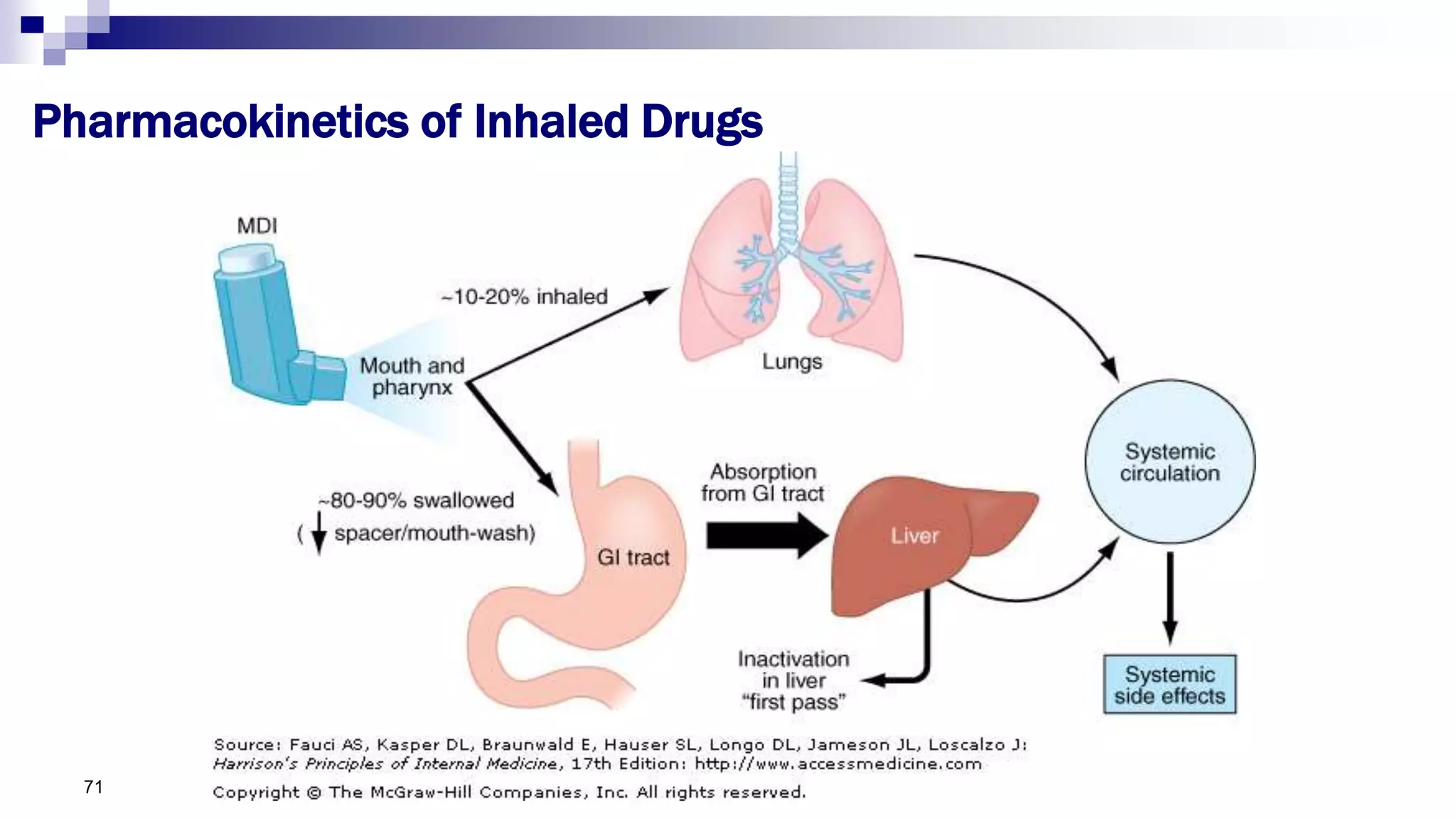
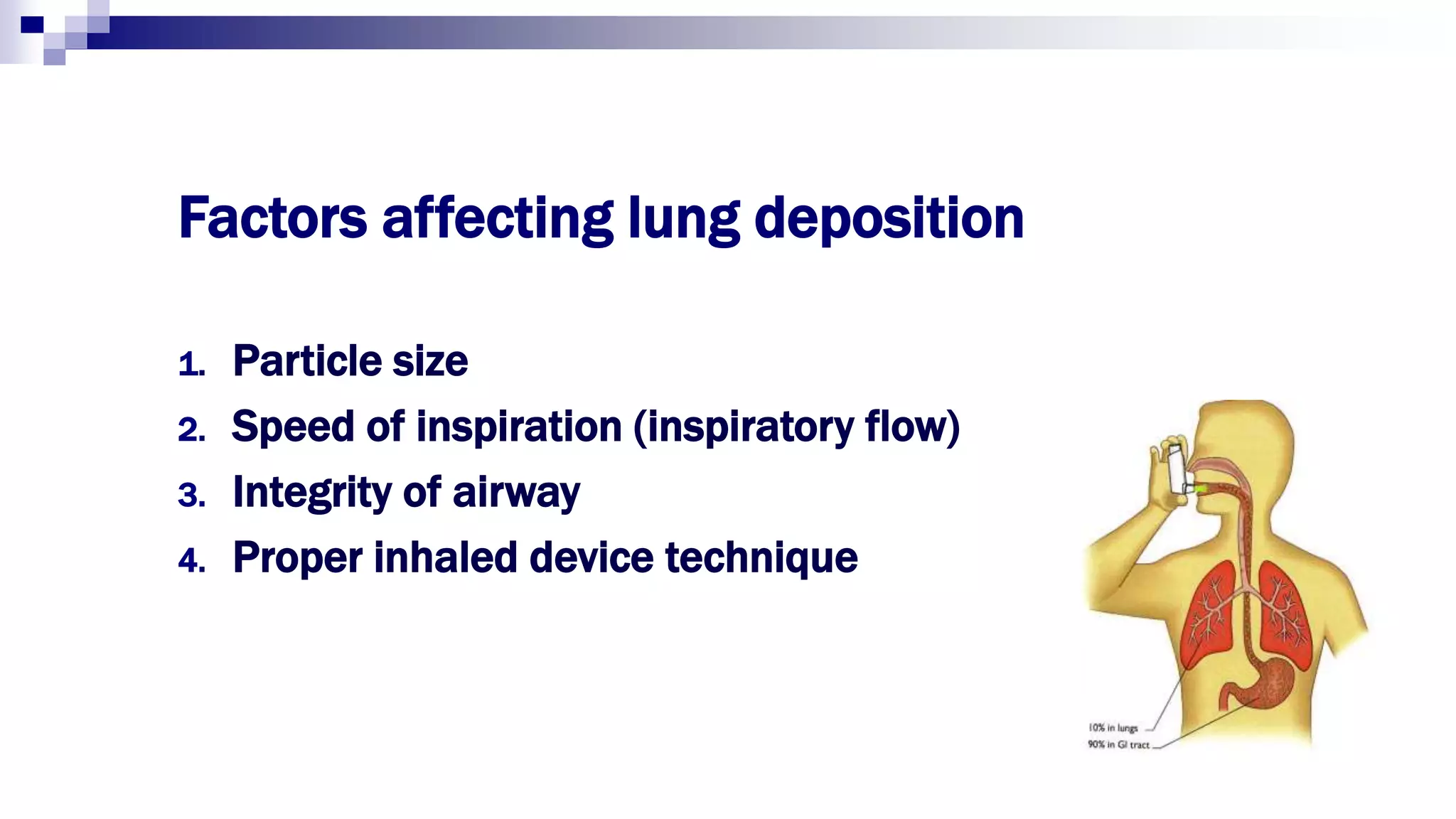
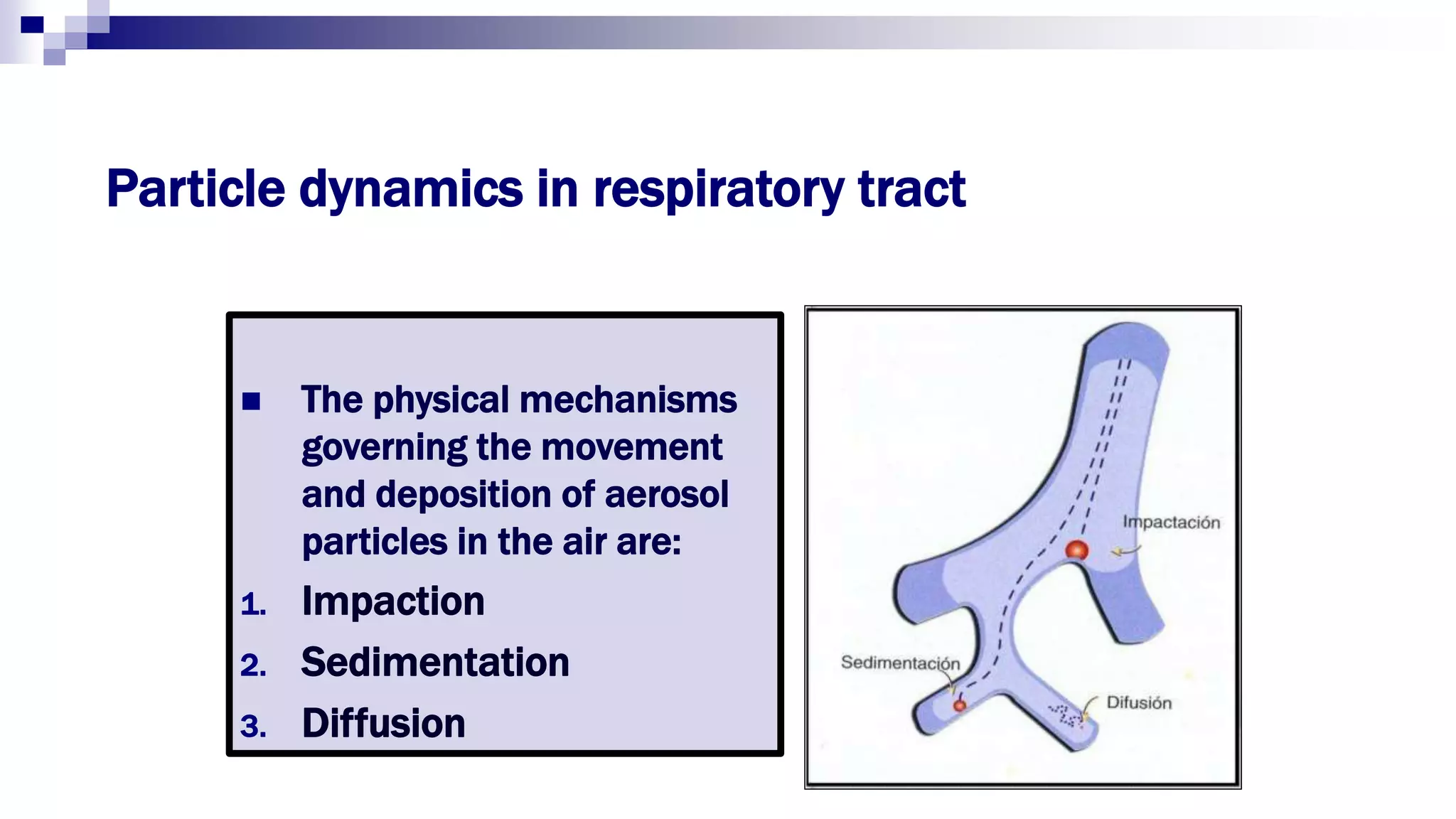
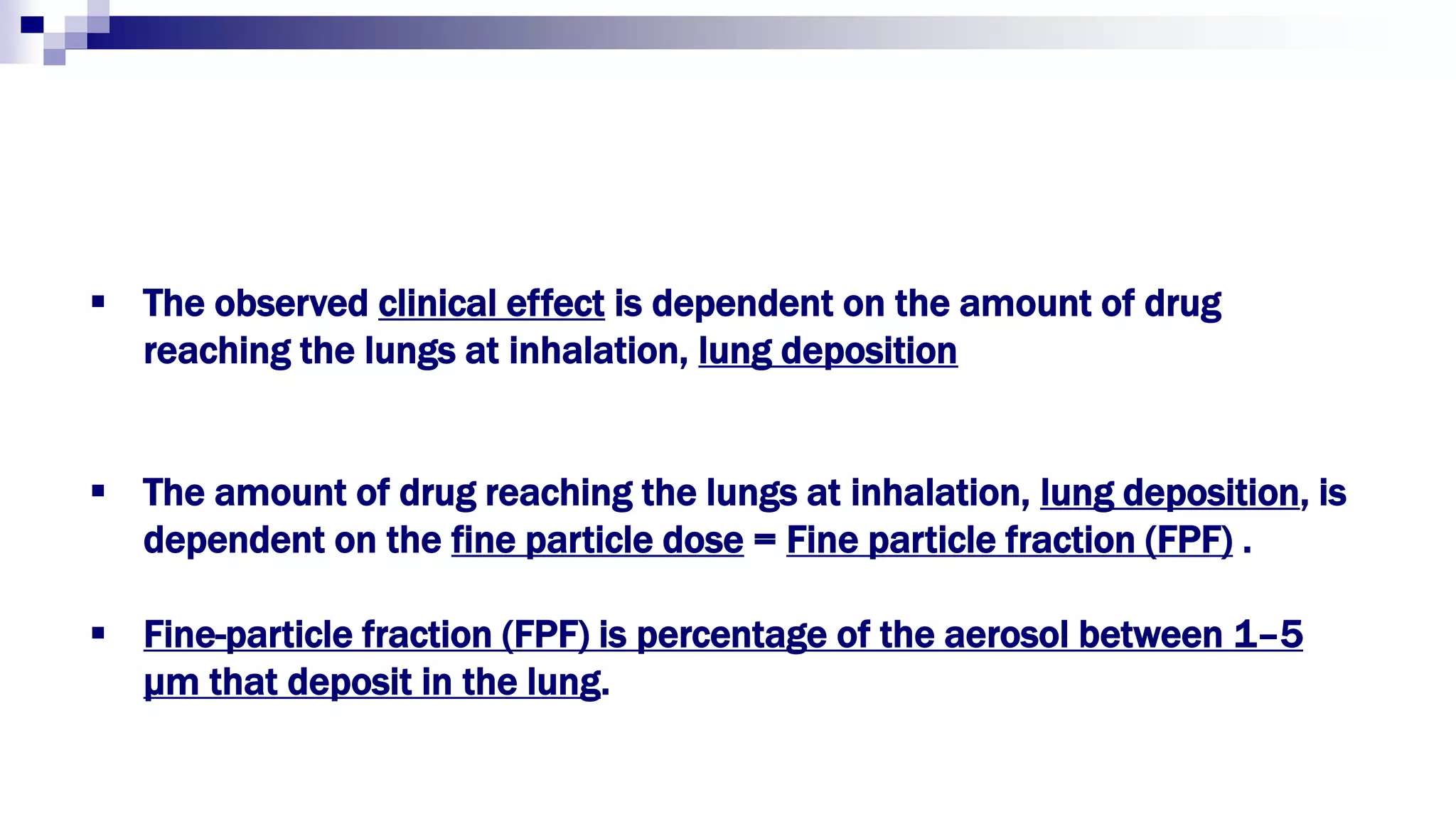
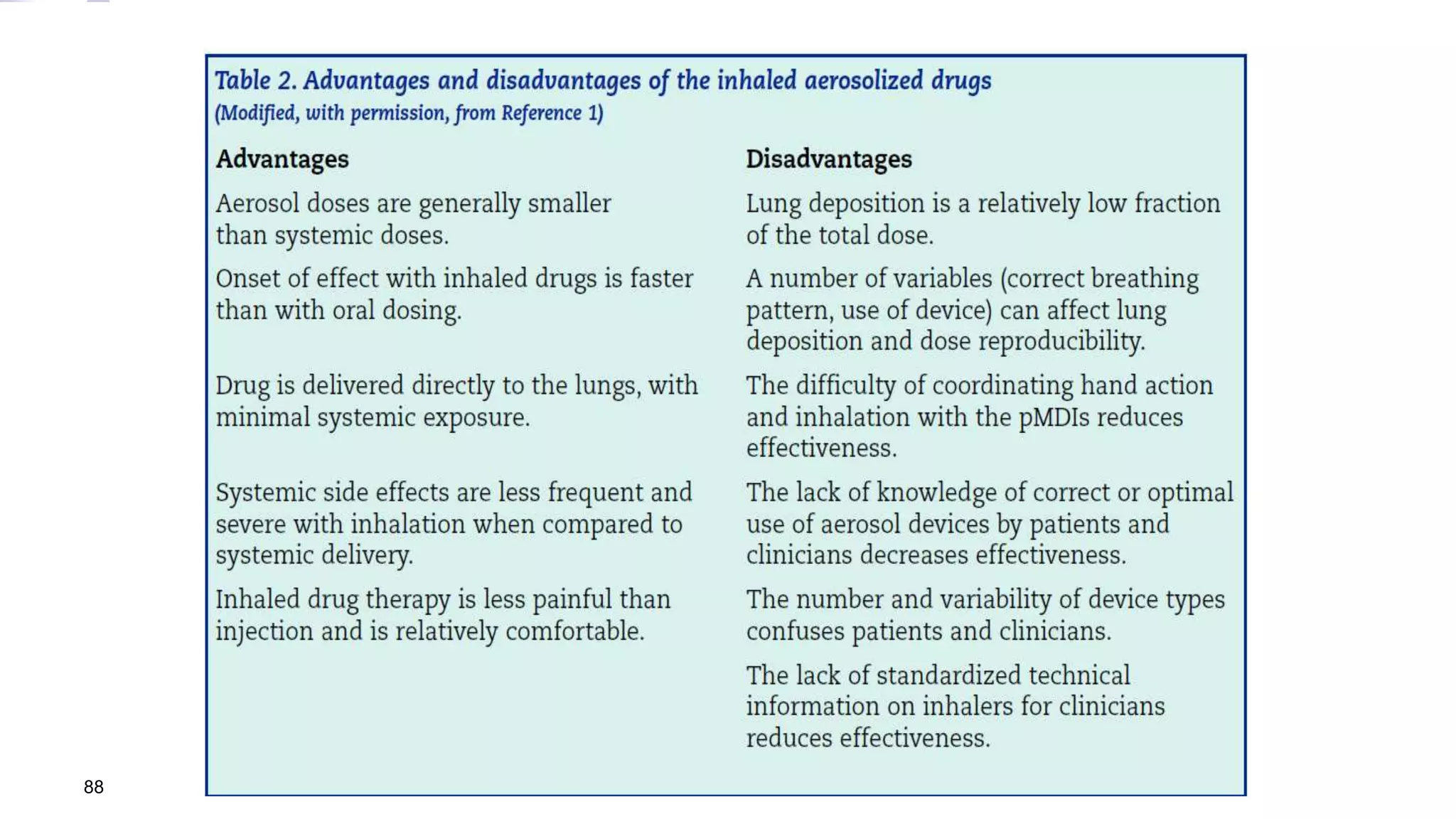
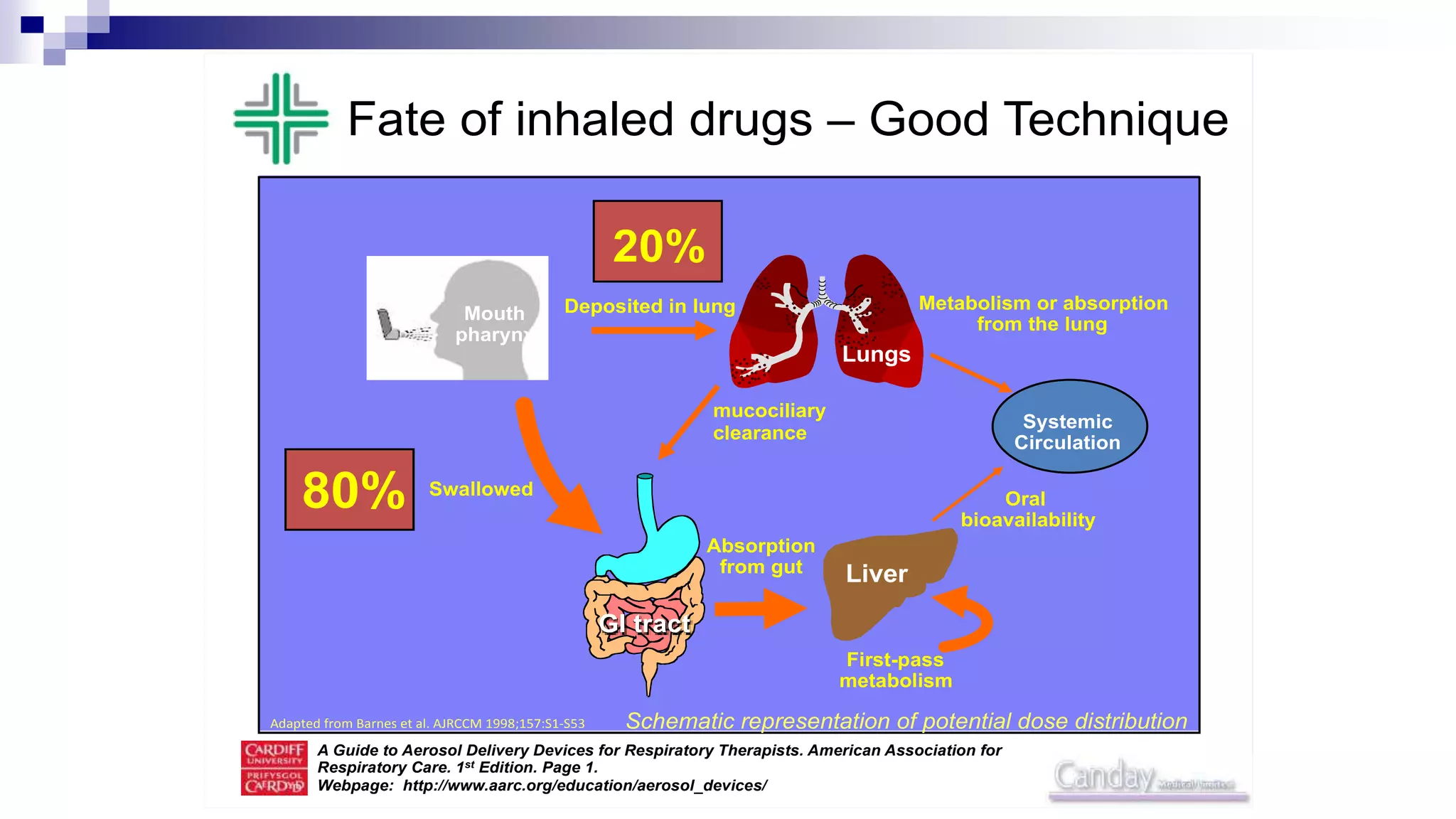
- Inhaled therapy is the cornerstone of asthma treatment and works by directly delivering medication to the airways.
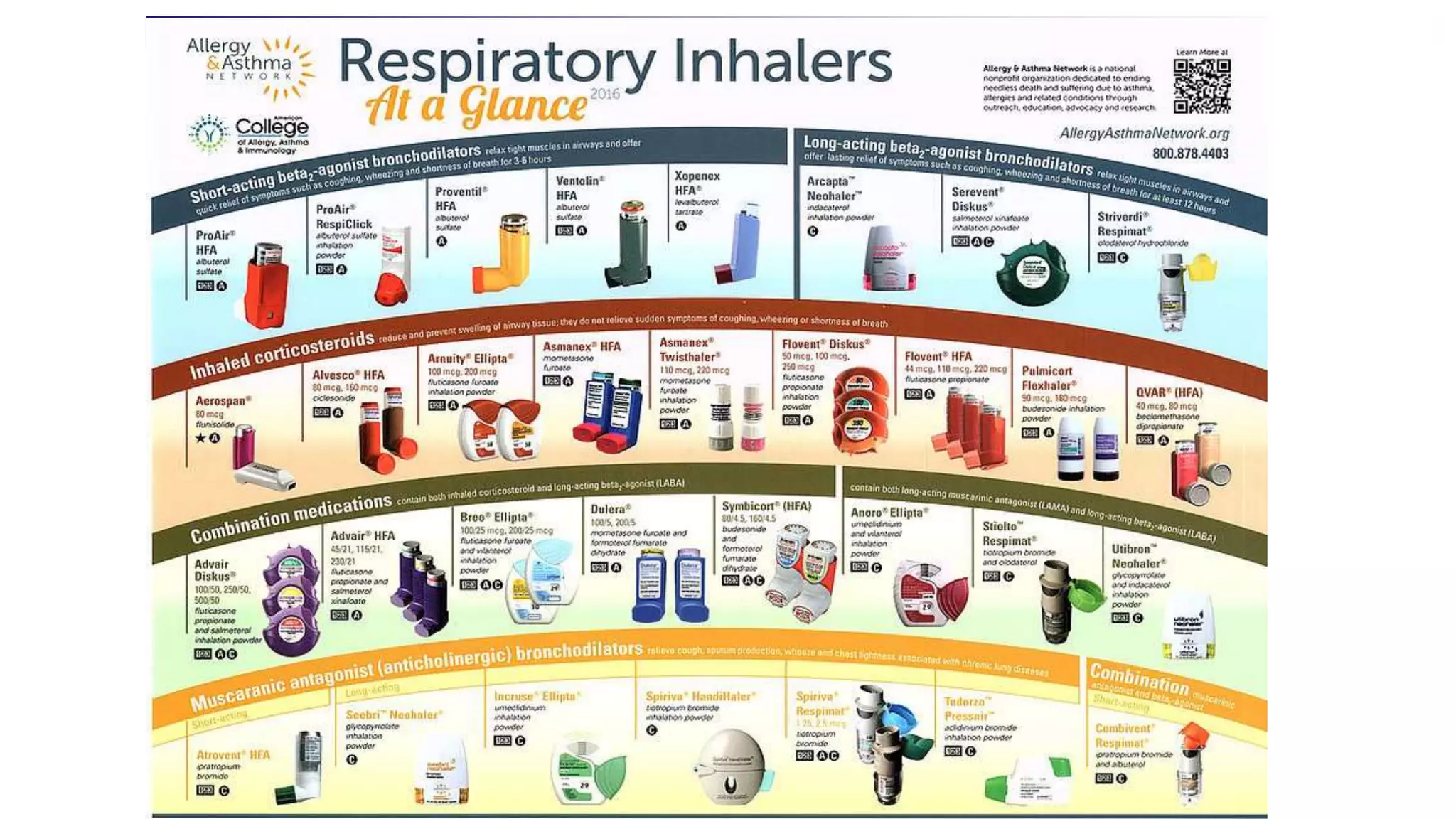
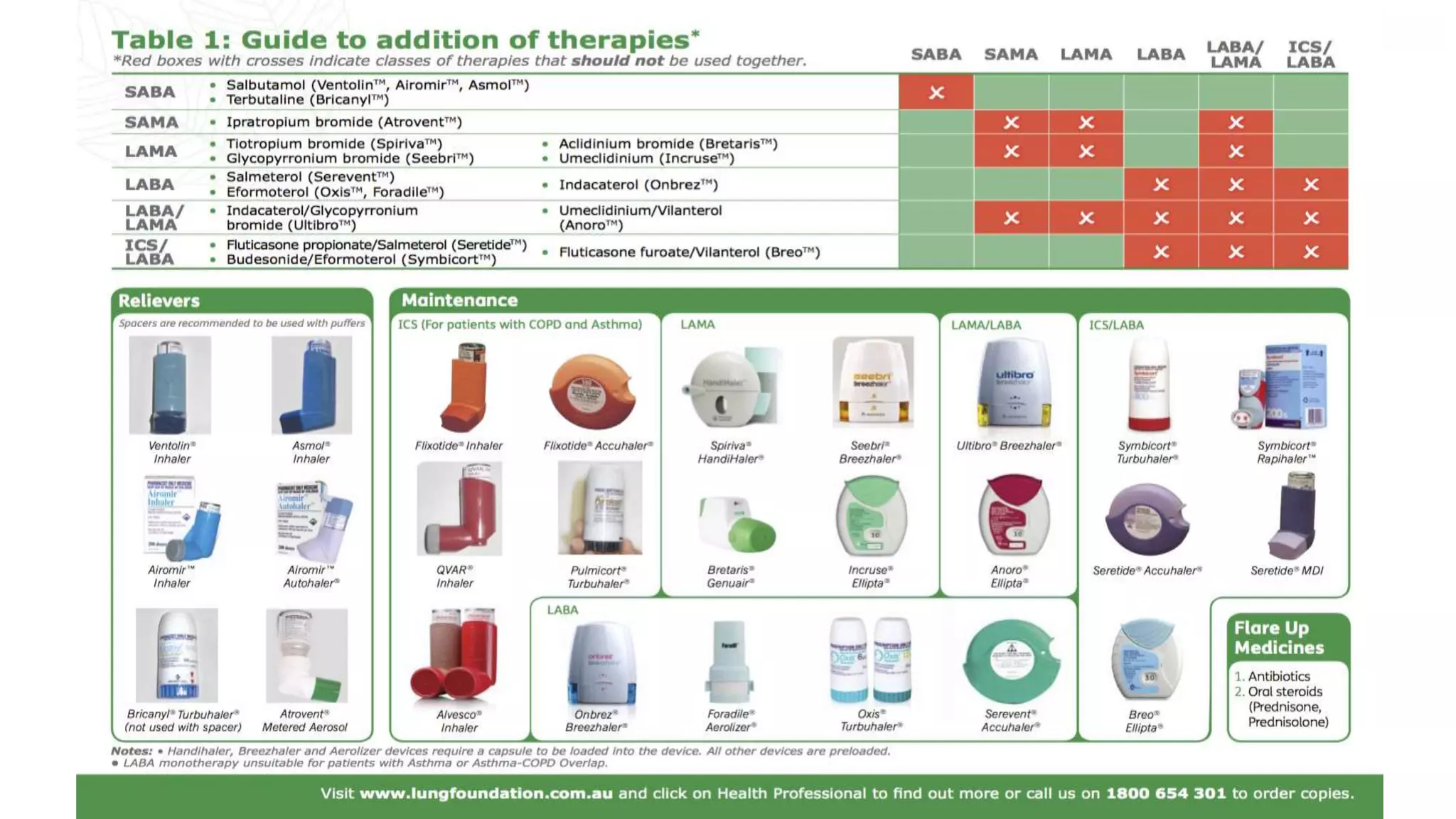
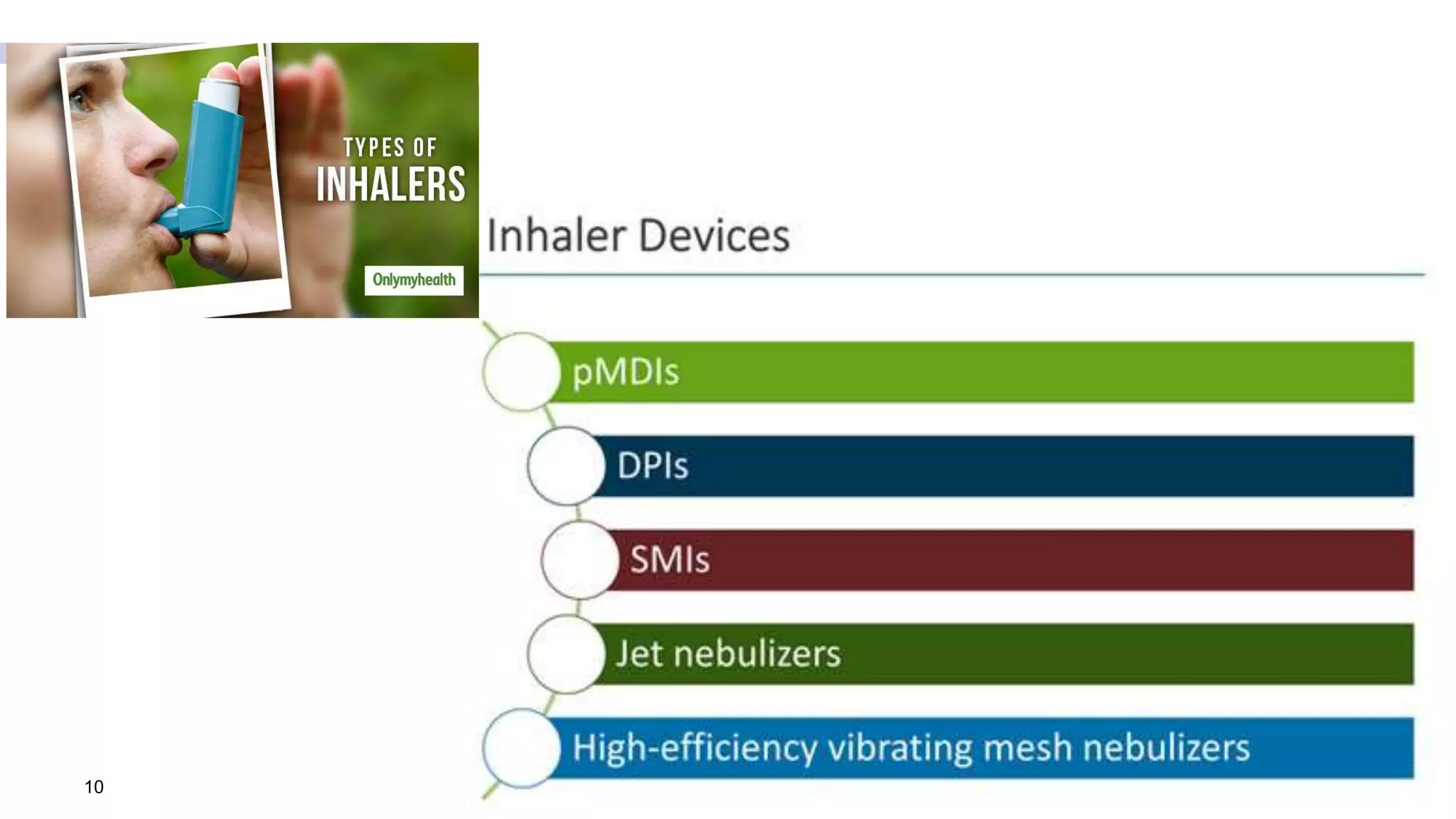
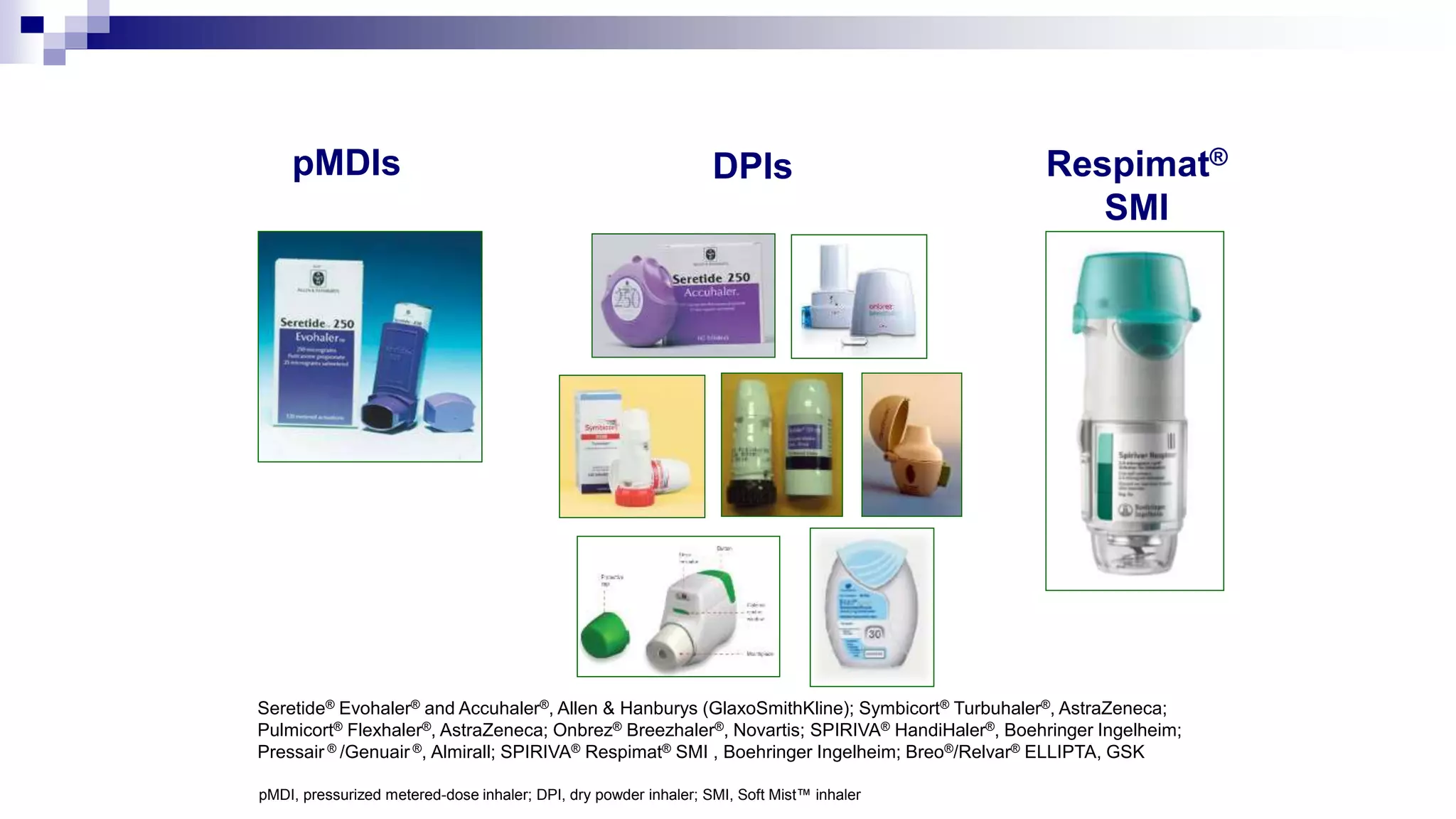
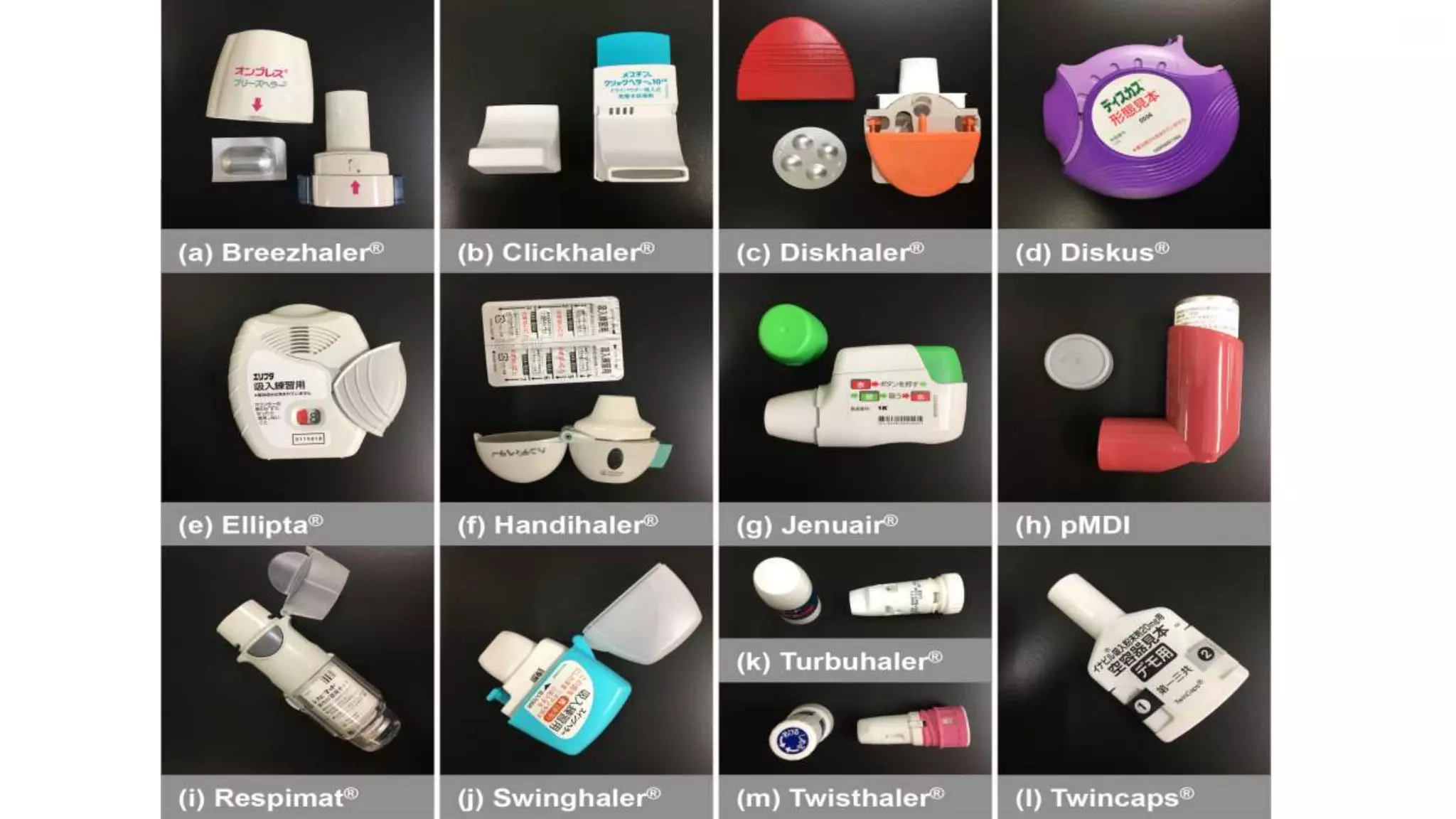
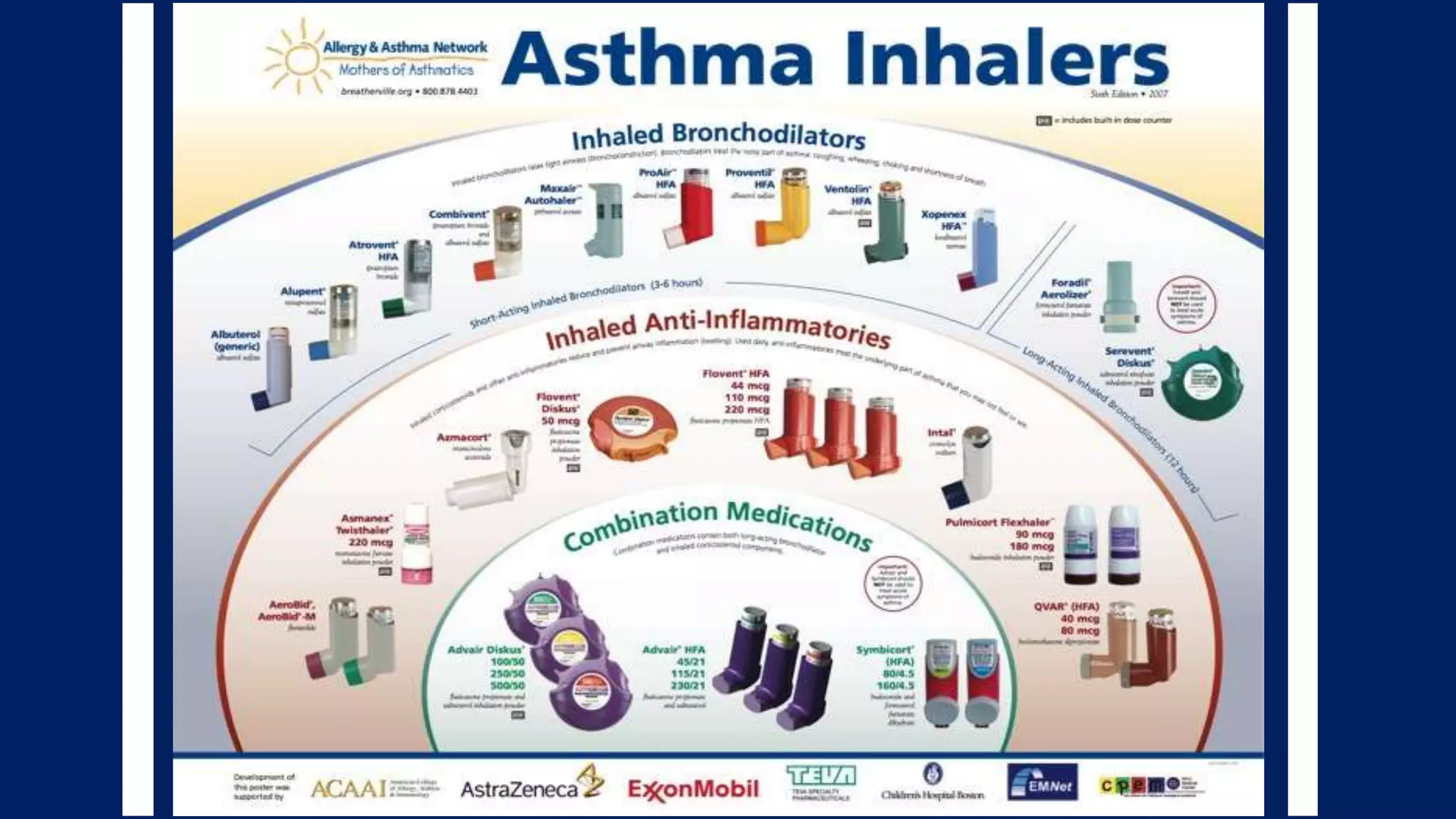
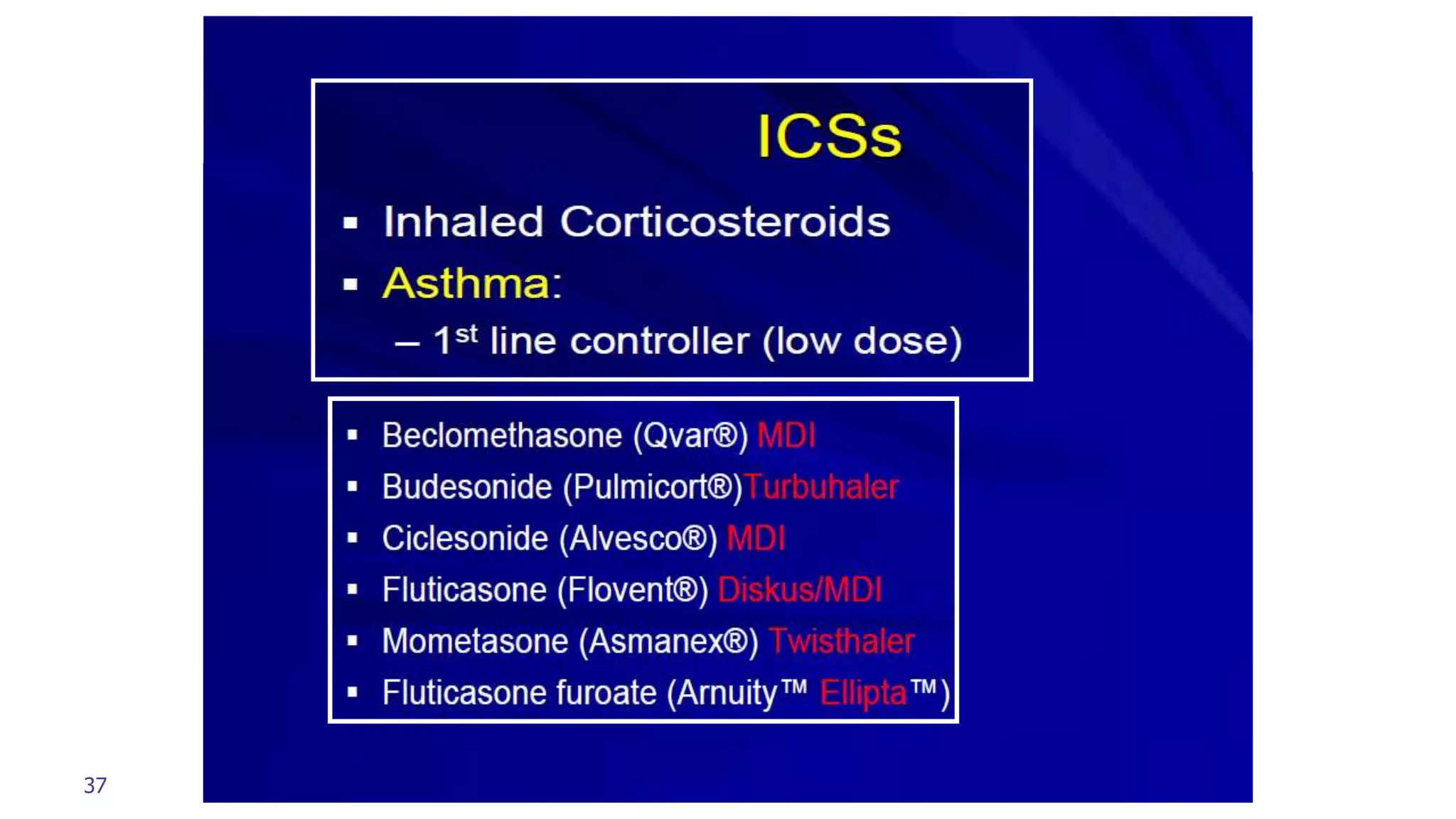
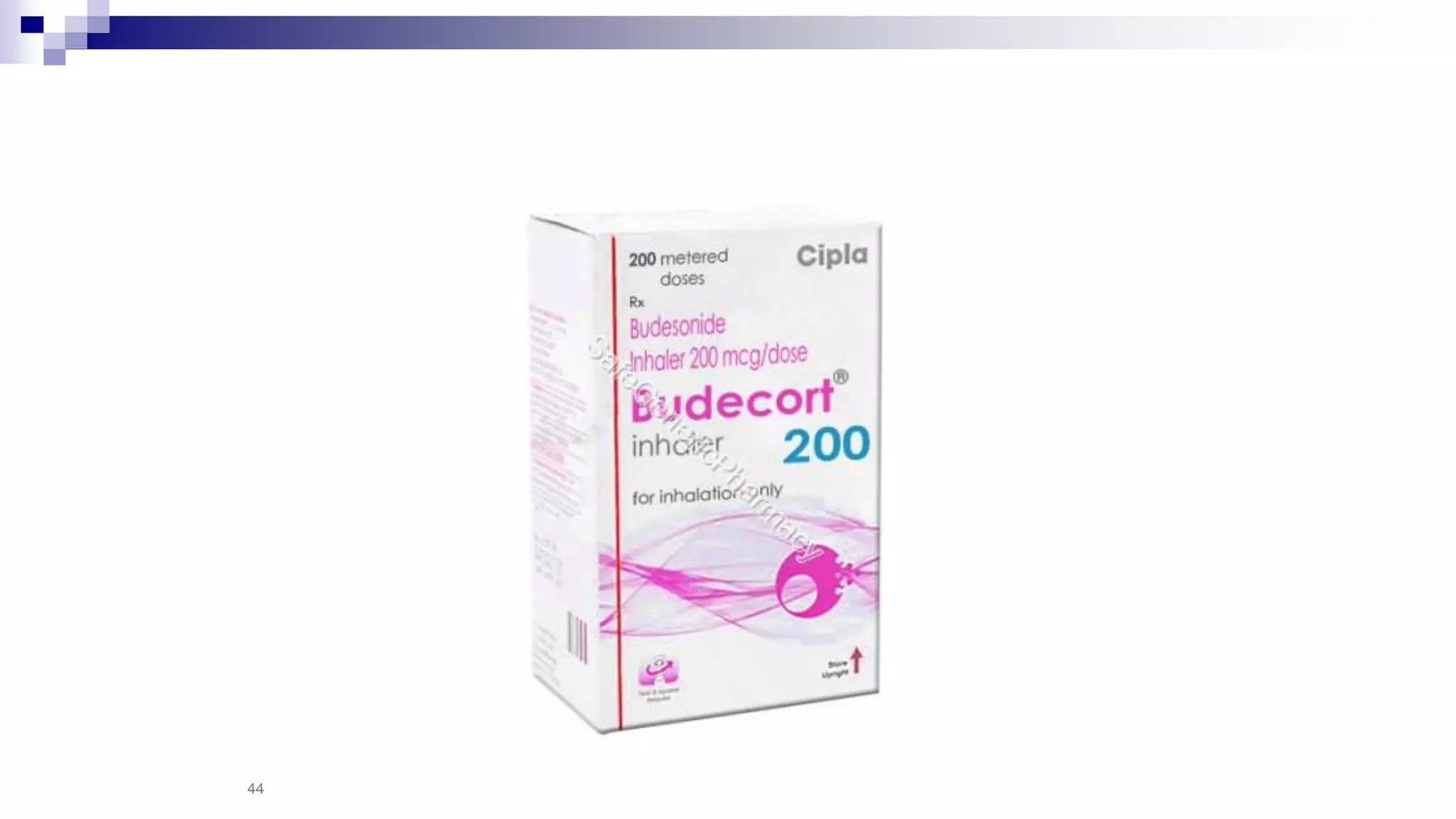
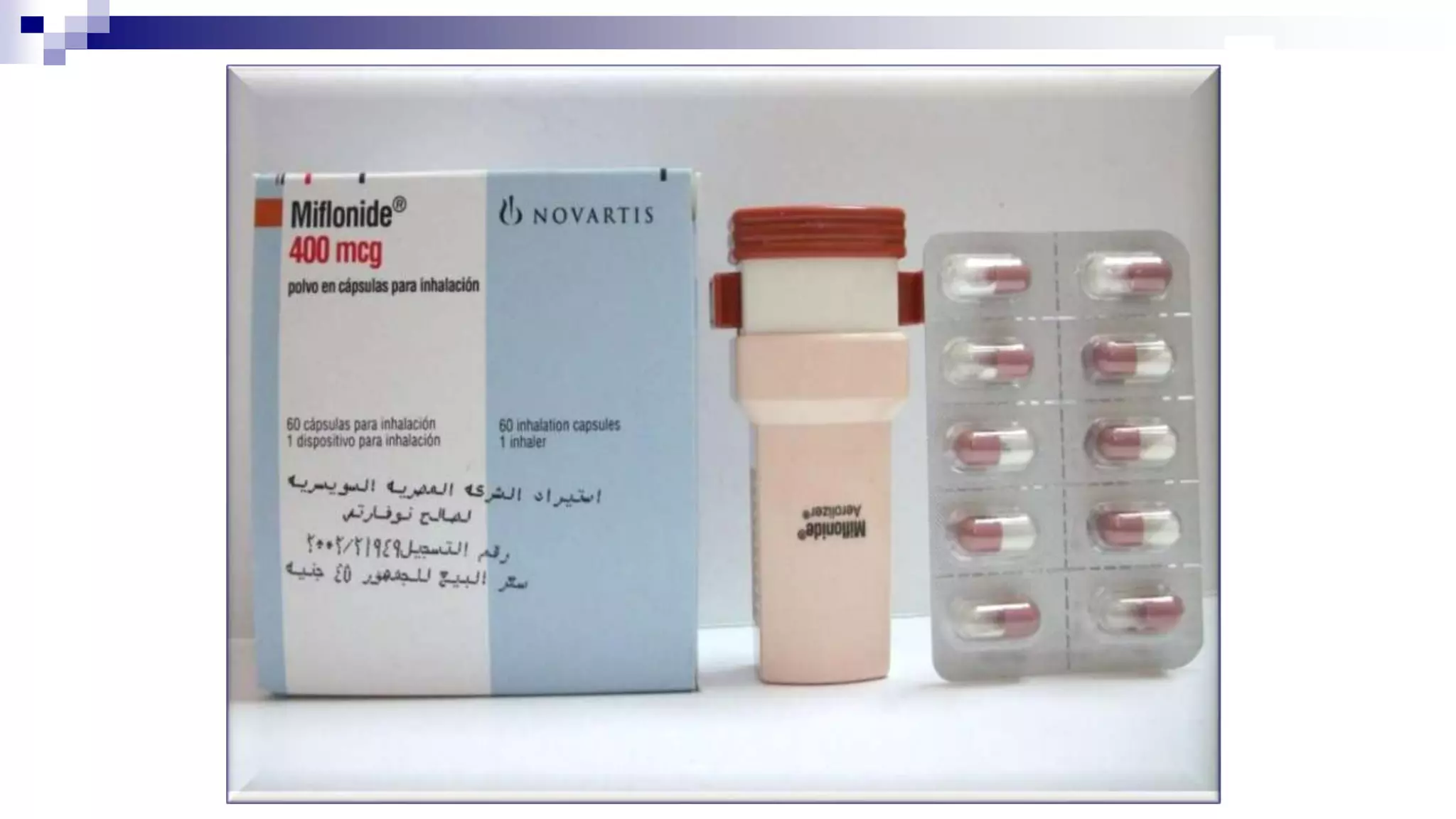
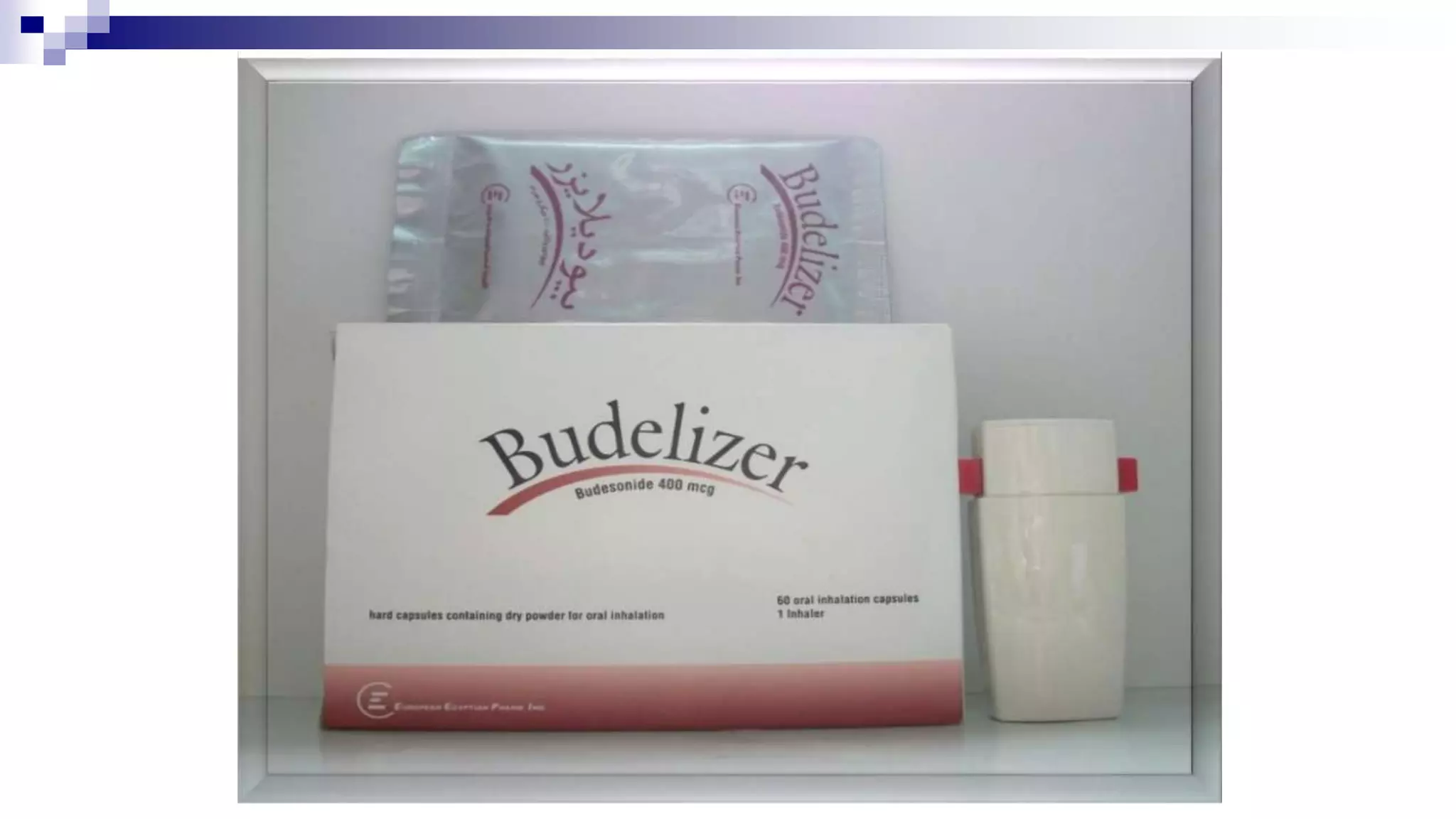
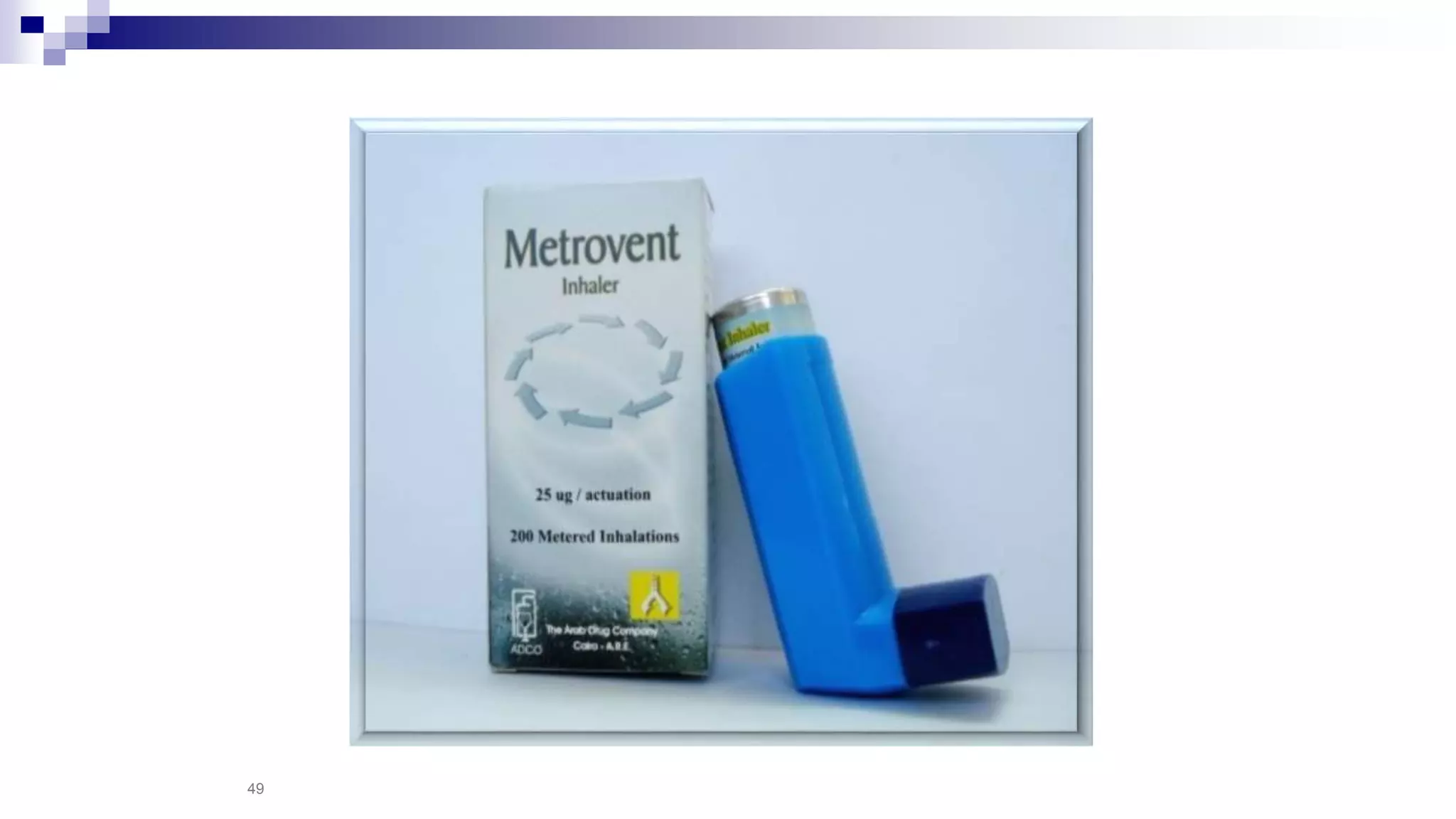
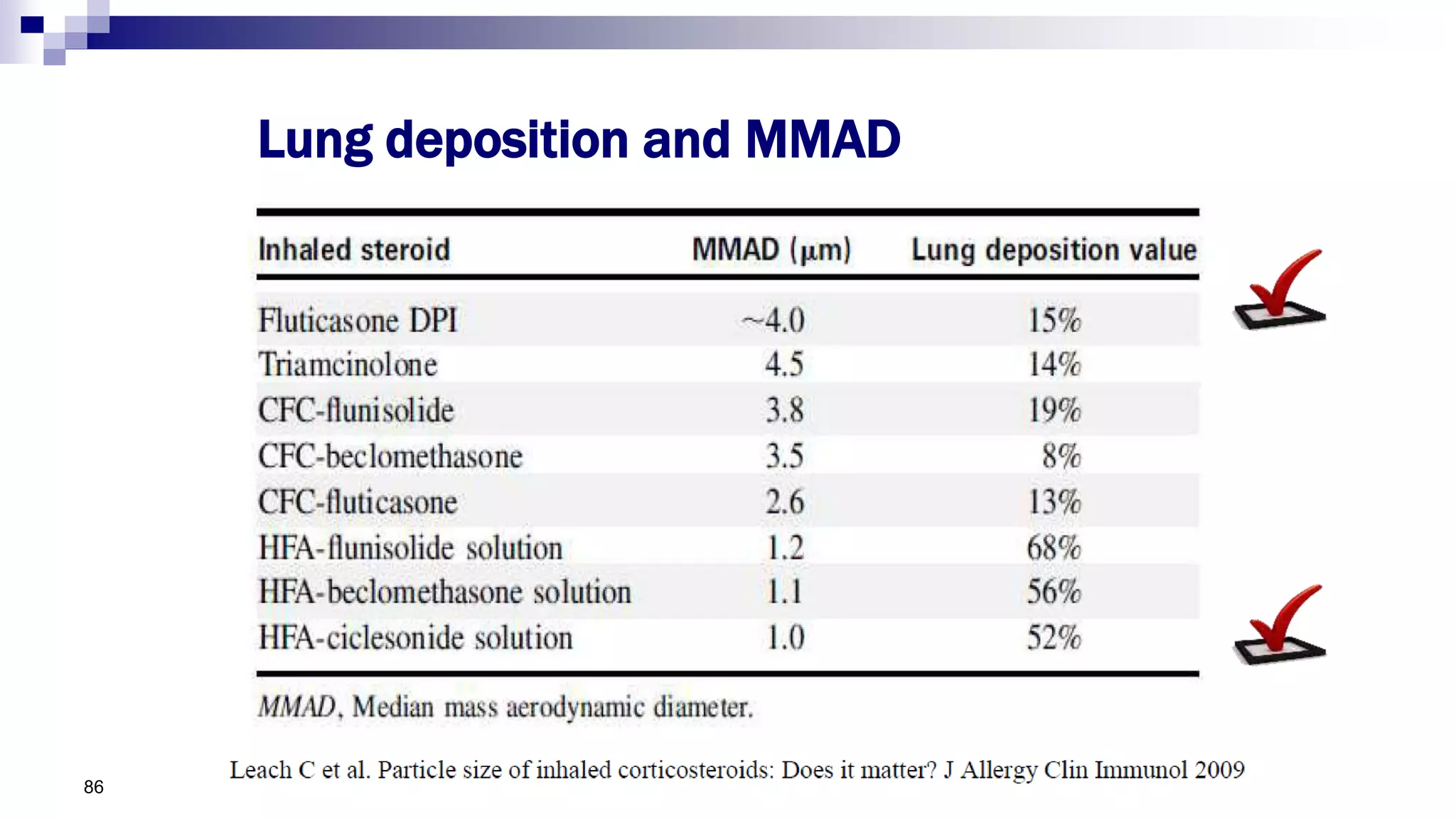
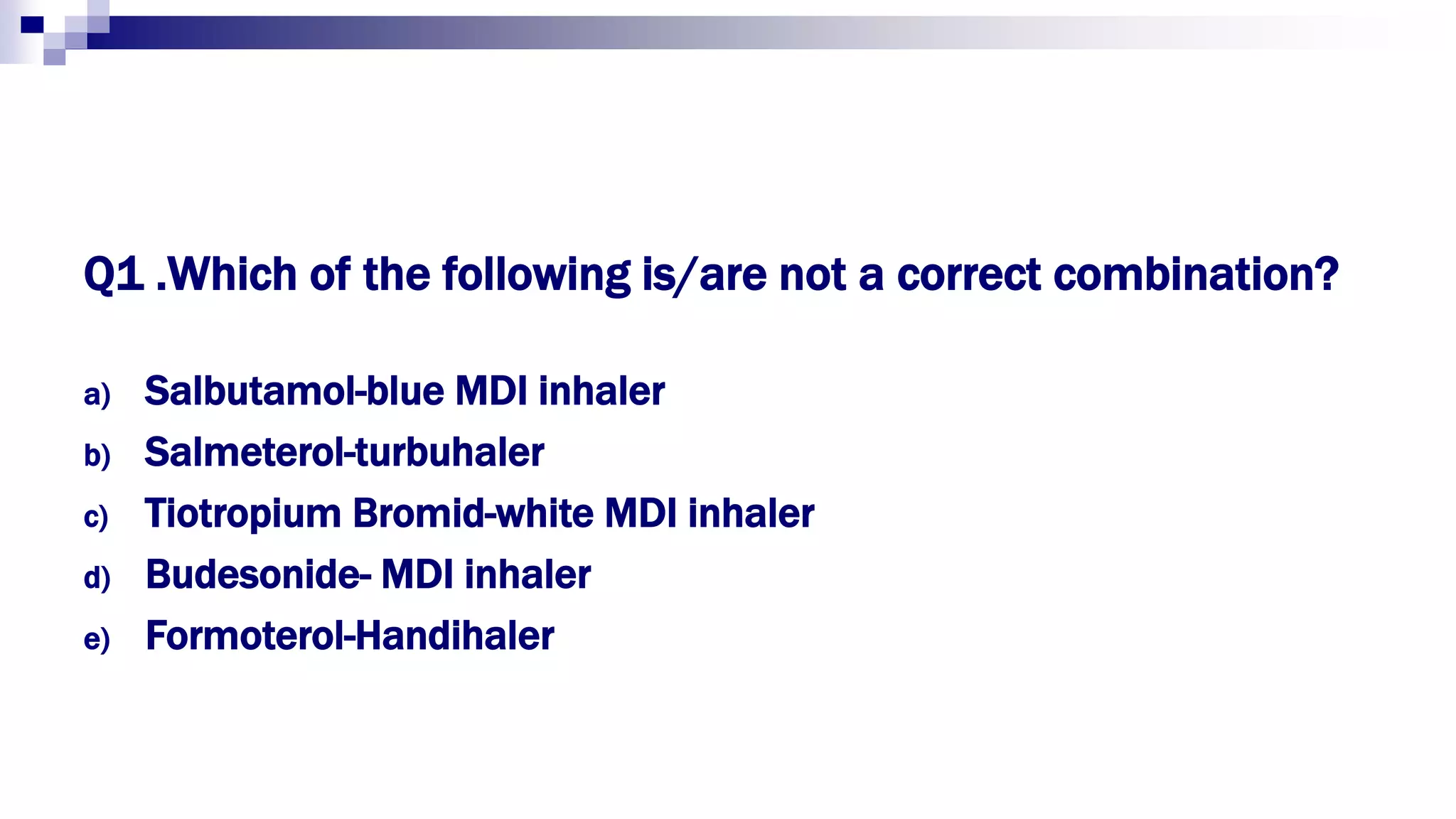
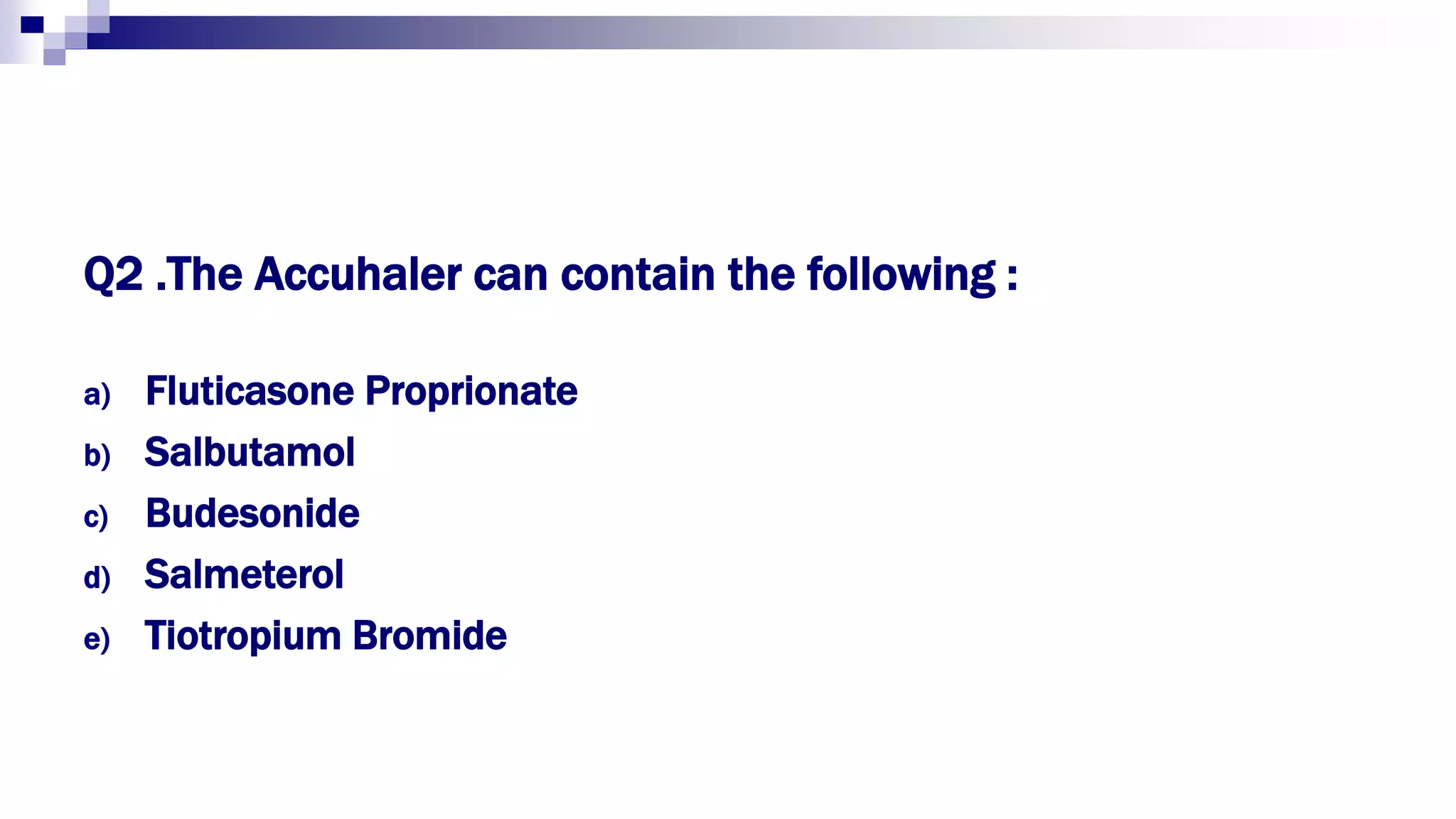
- Different types of inhalers include pressurized metered dose inhalers, dry powder inhalers, and soft mist inhalers.
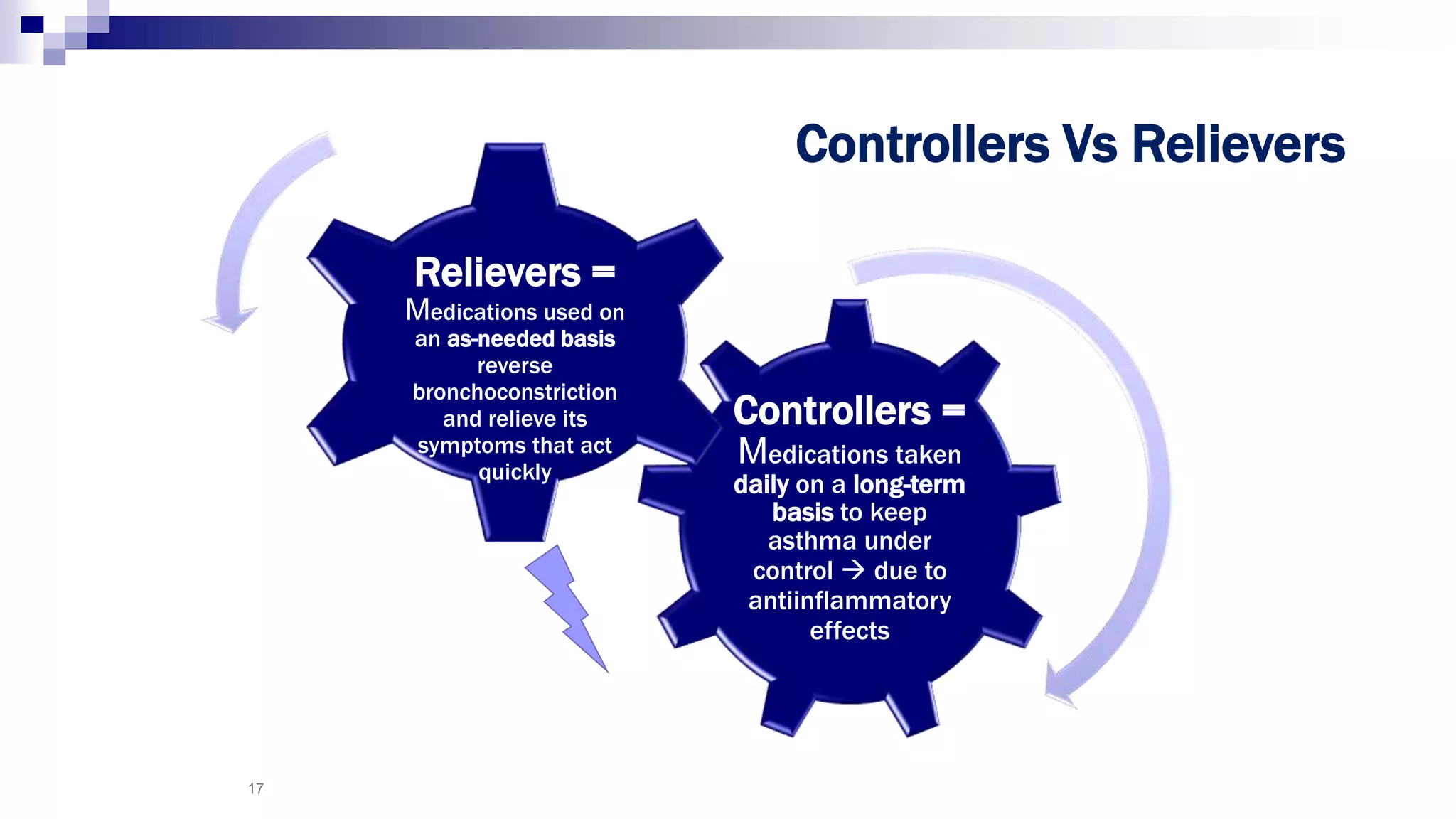
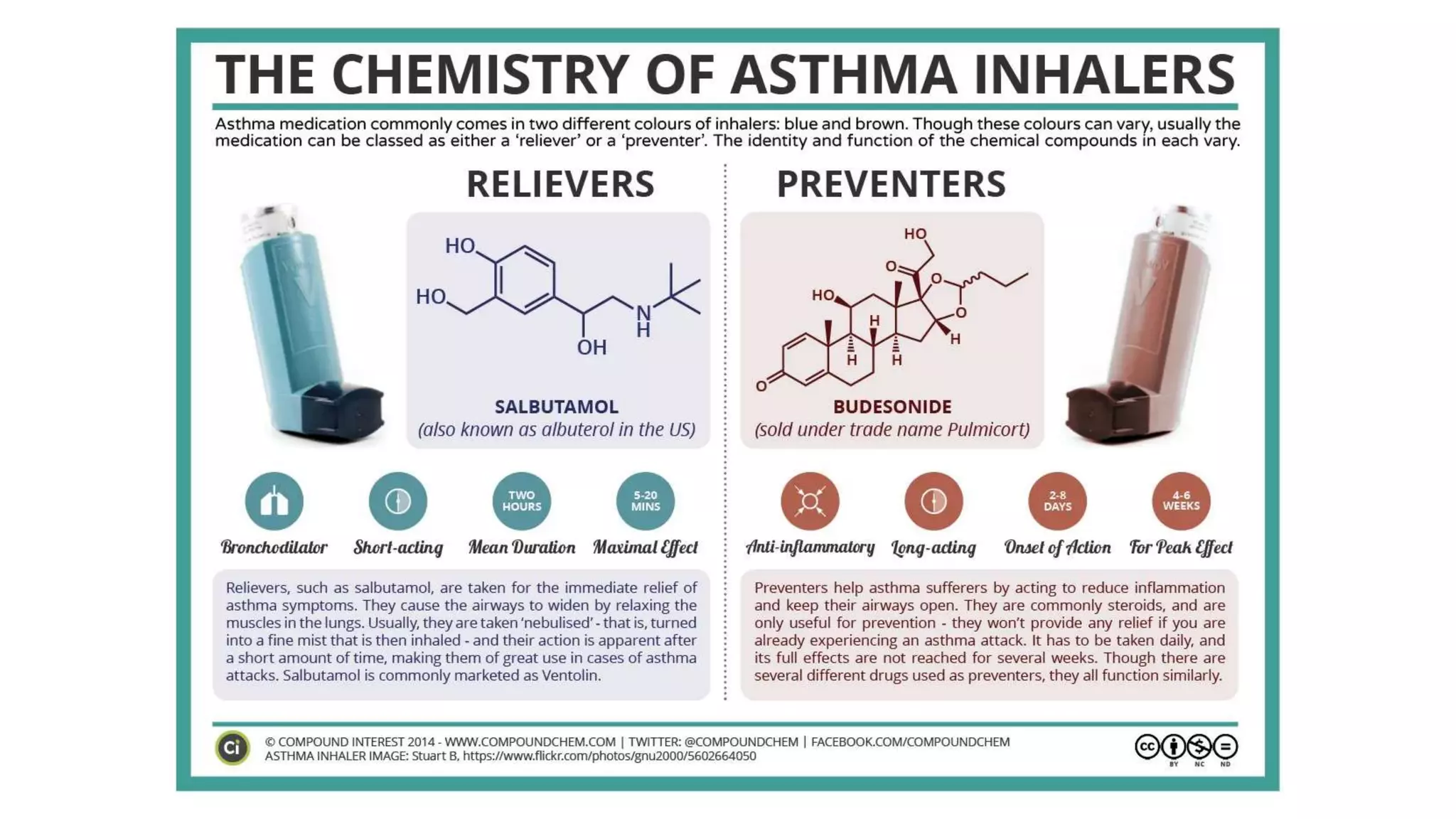
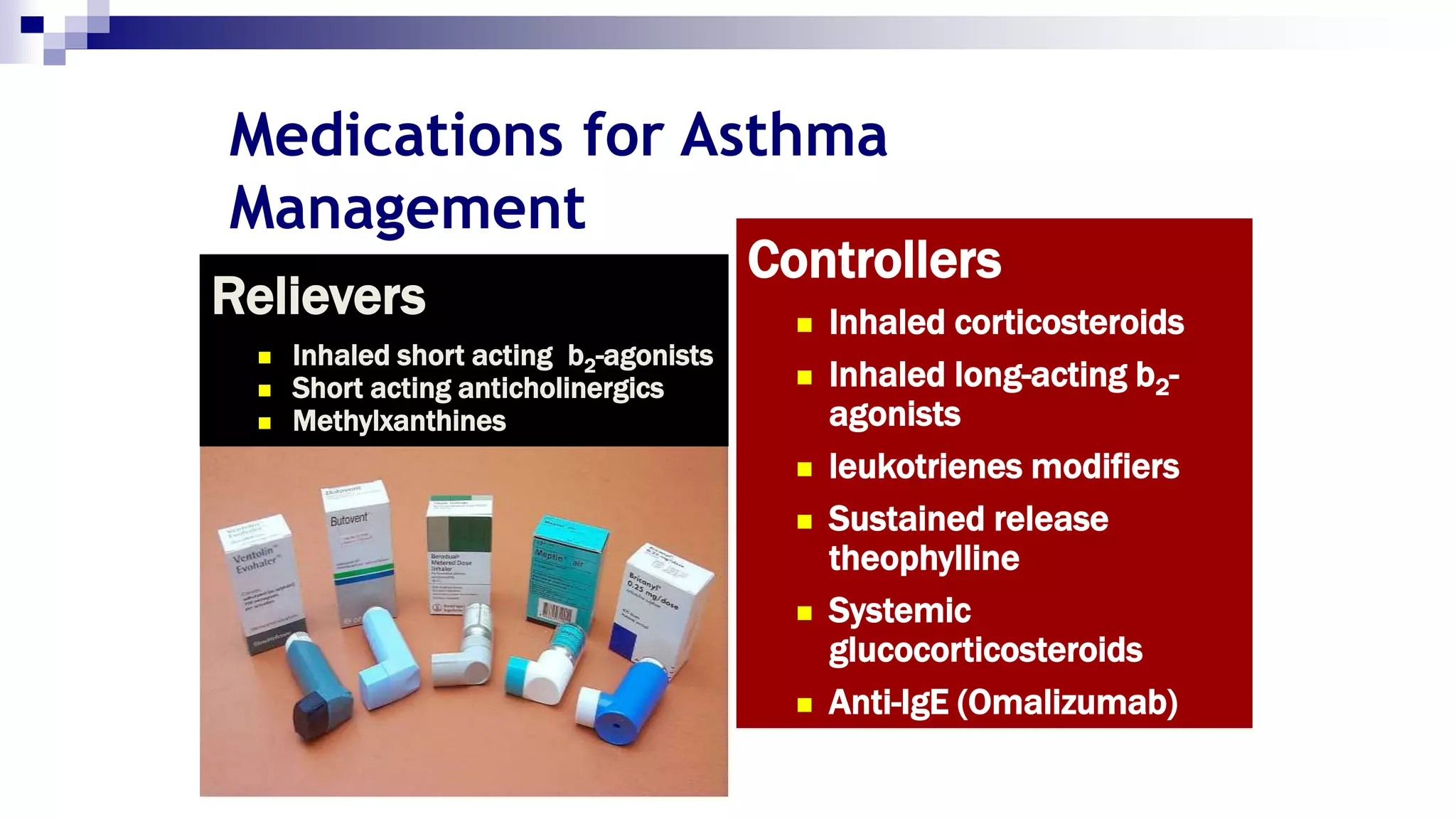
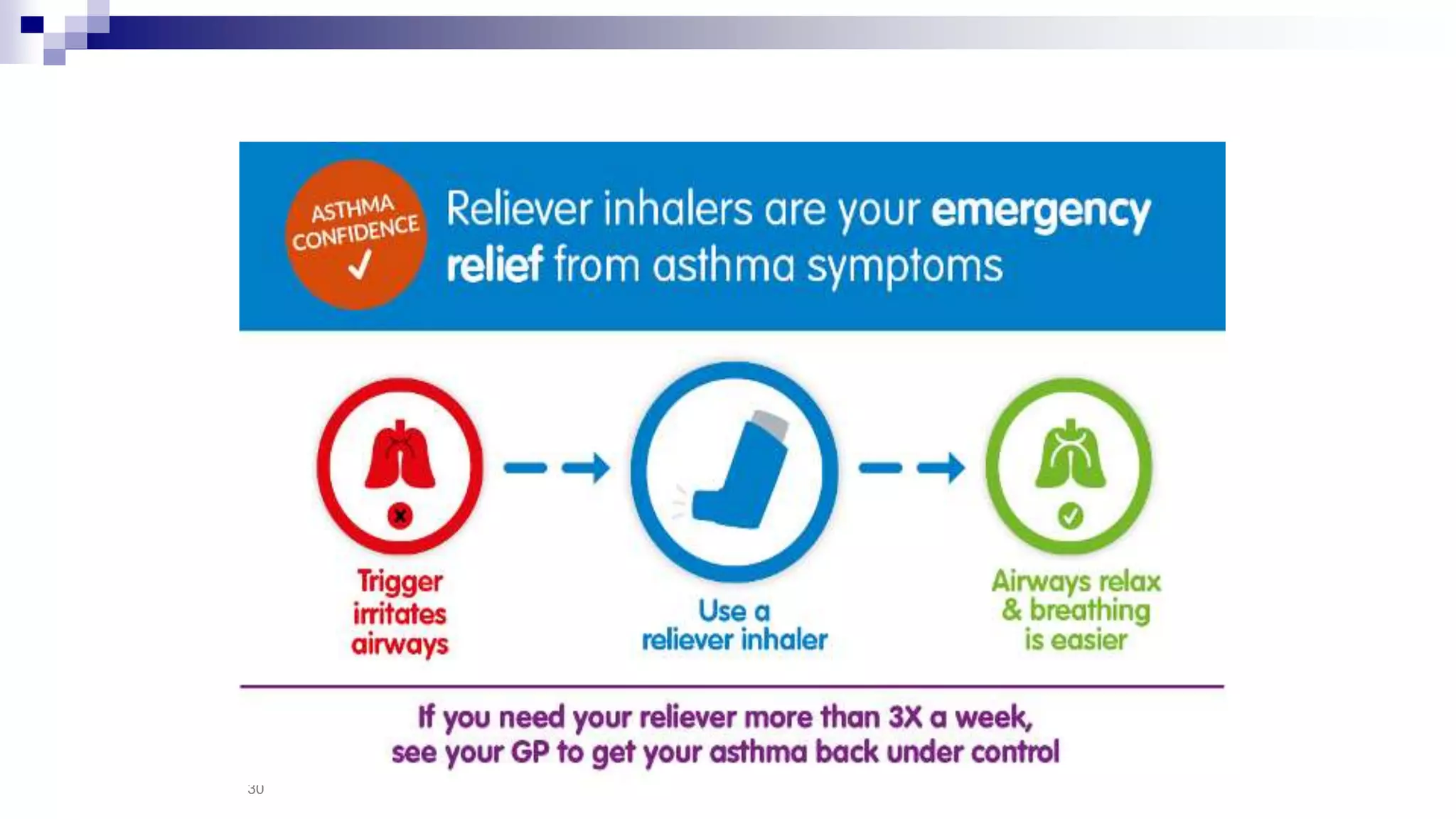
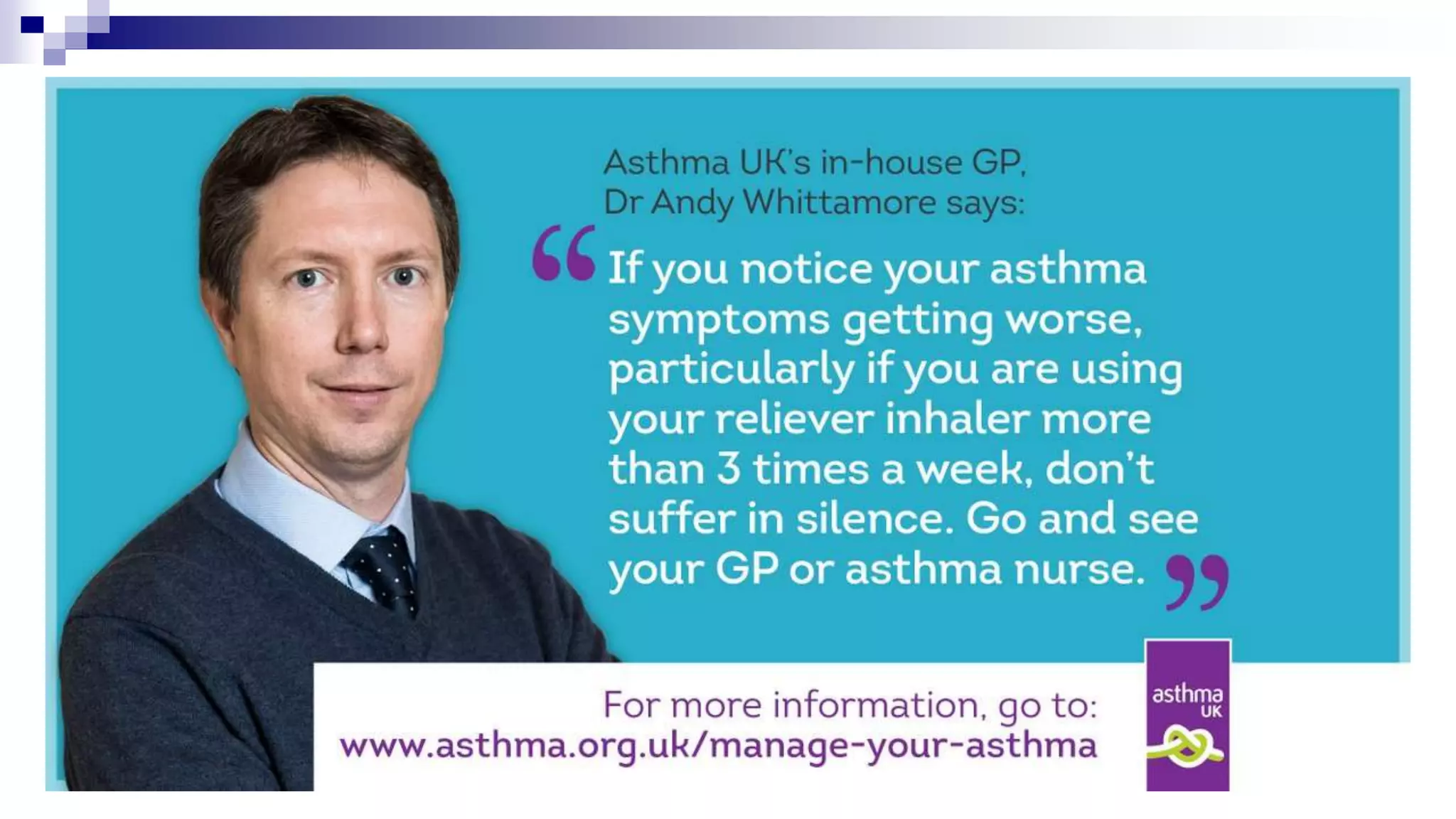
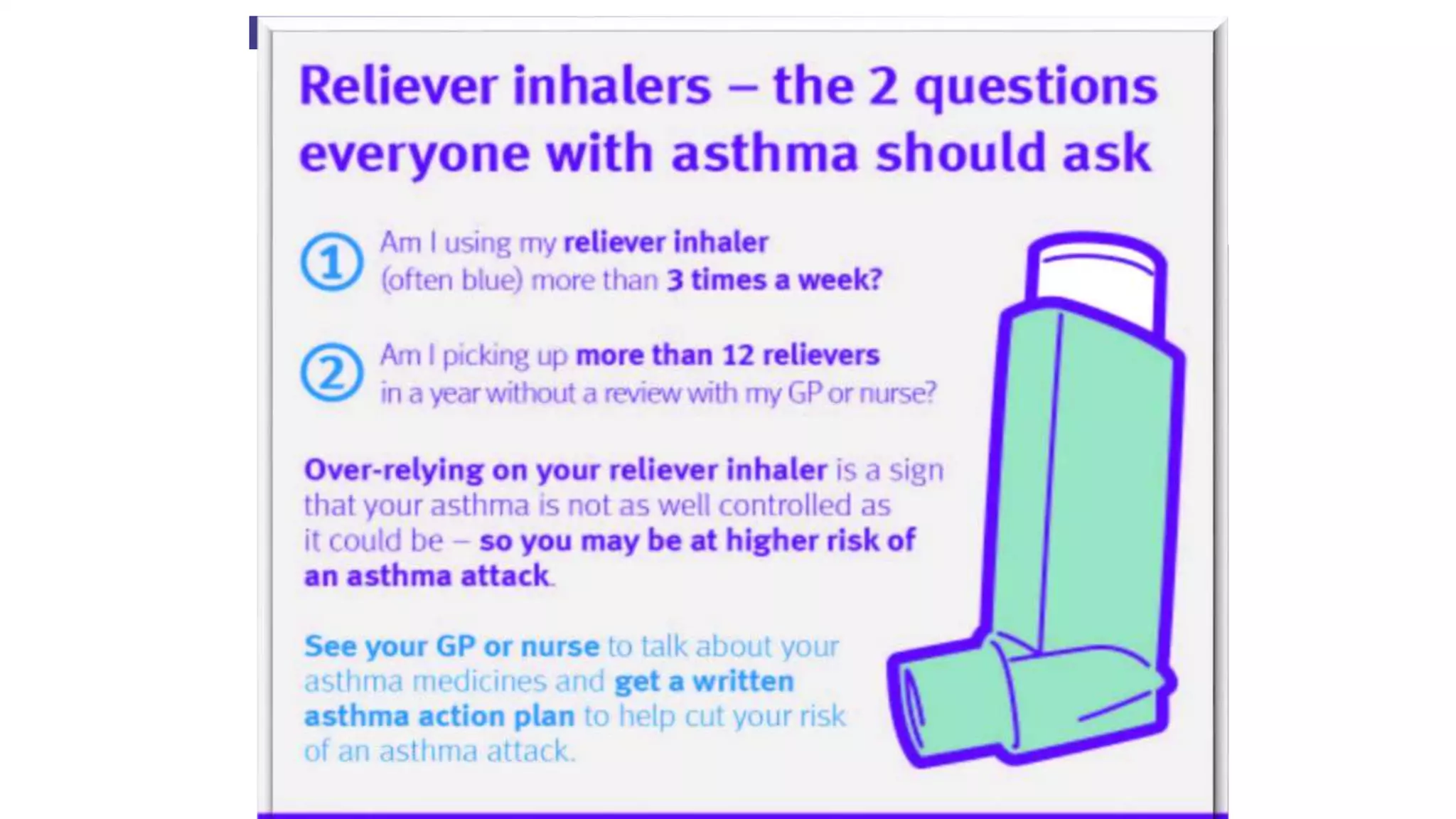
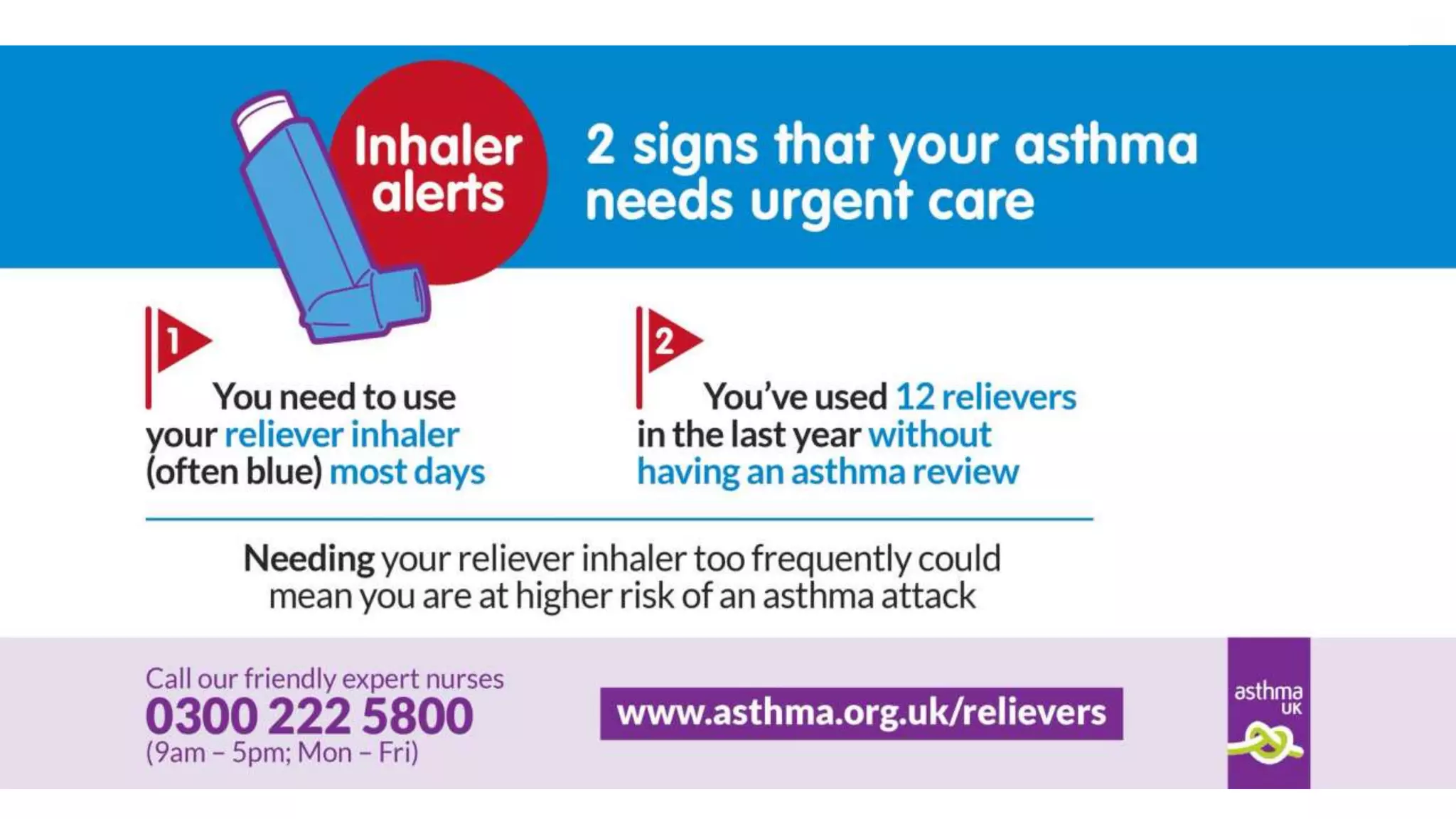
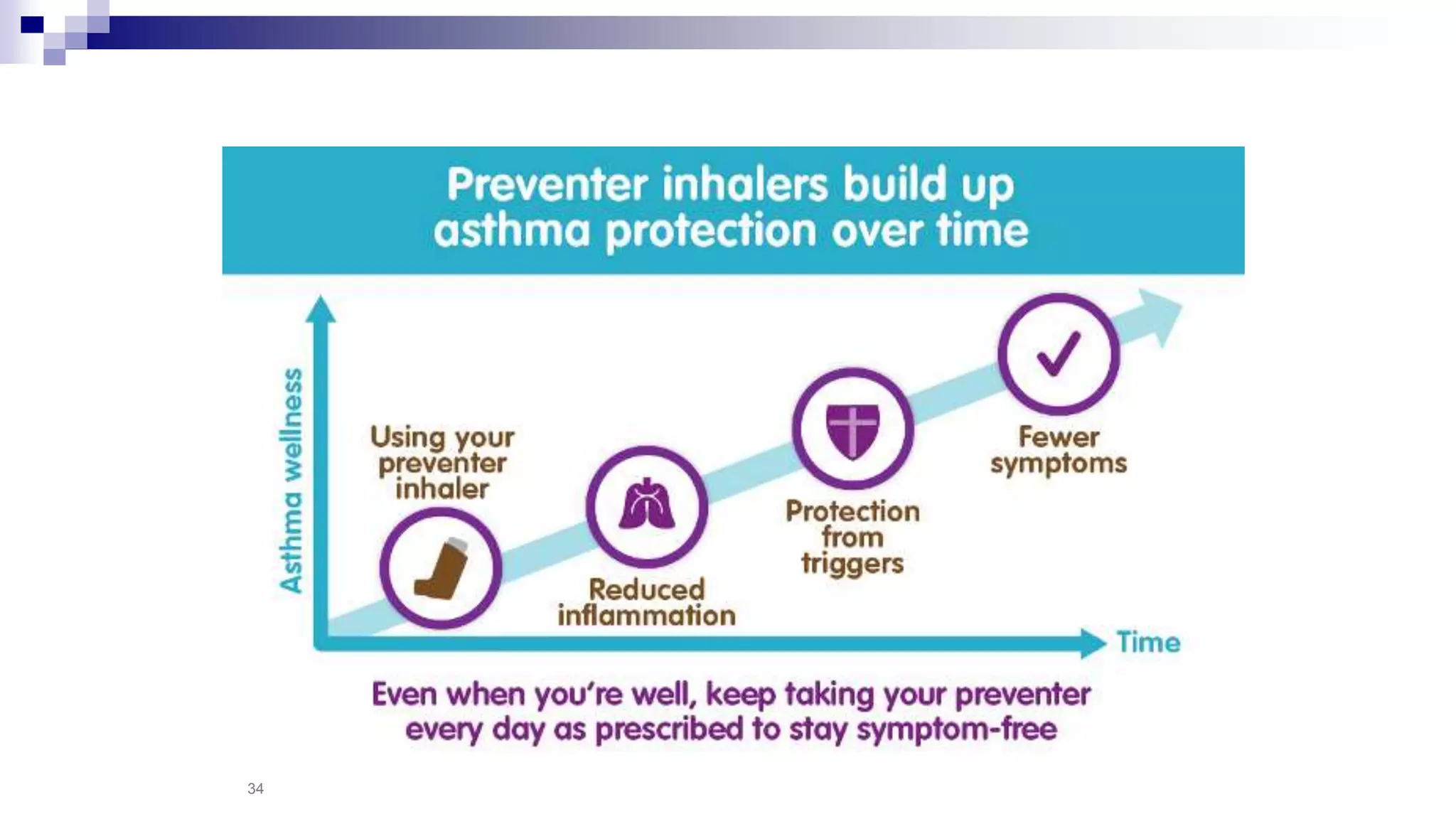
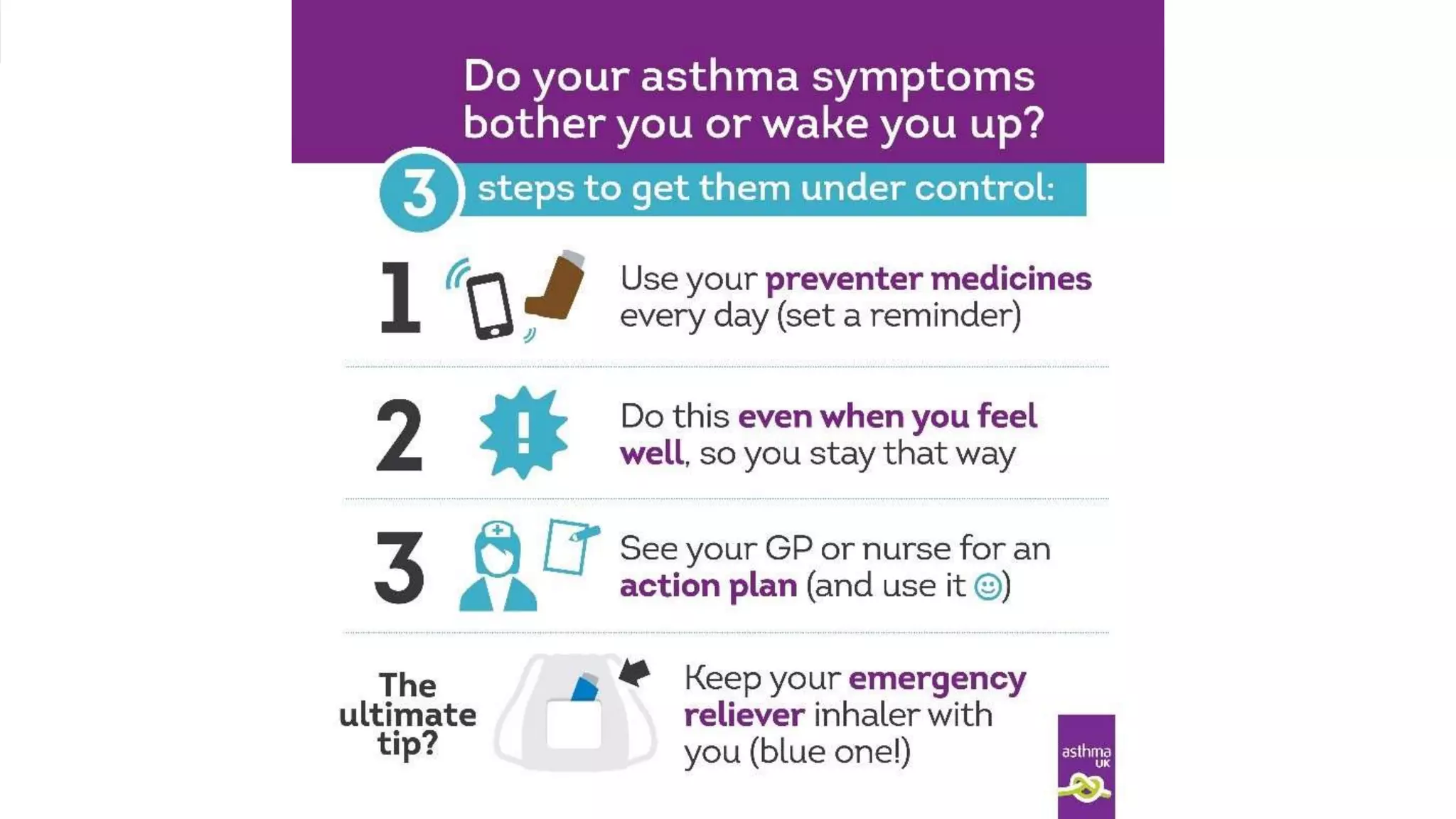
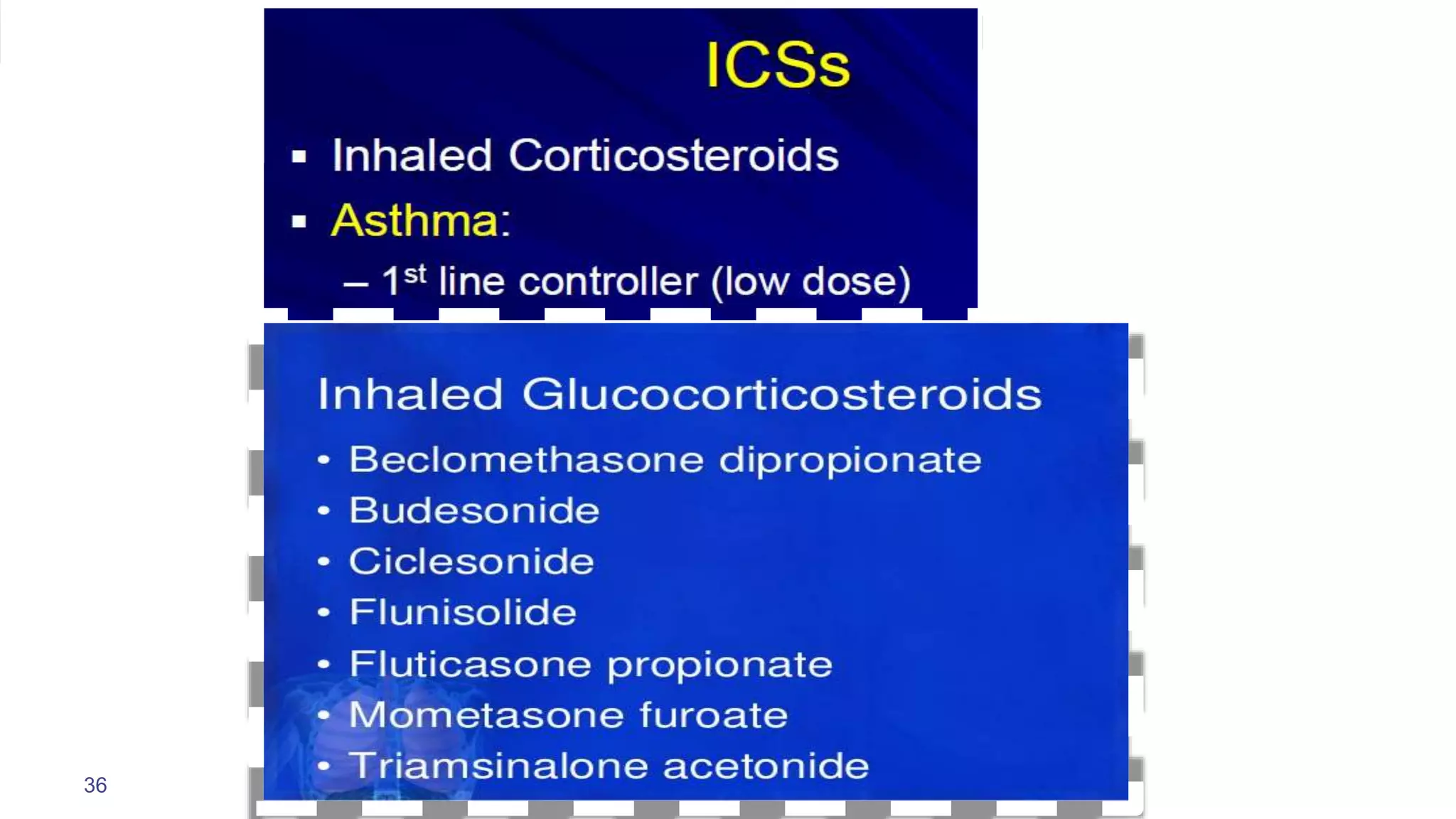
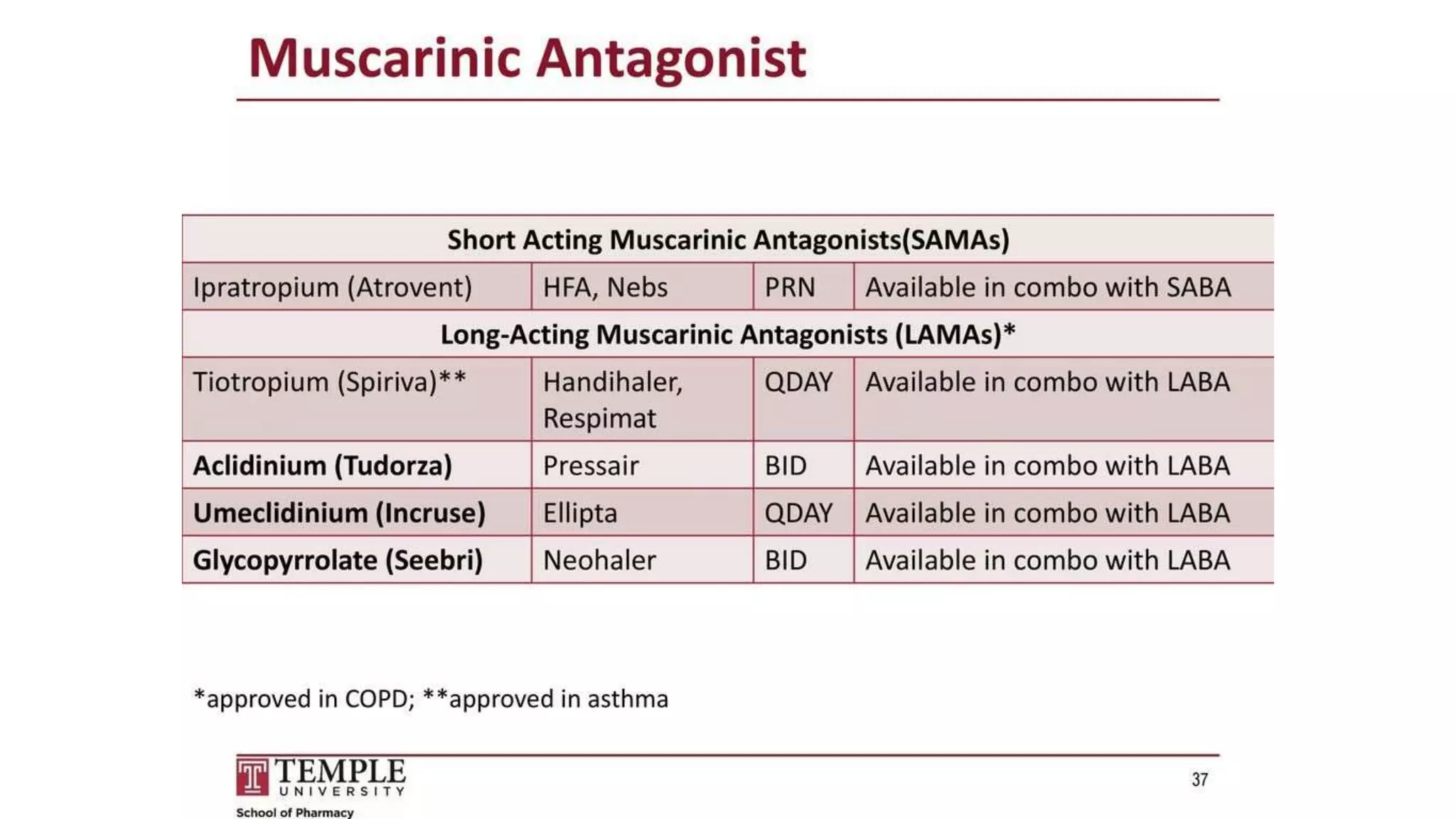
- Inhaled medications are divided into controllers taken daily to control inflammation and relievers used as needed to provide quick symptom relief.
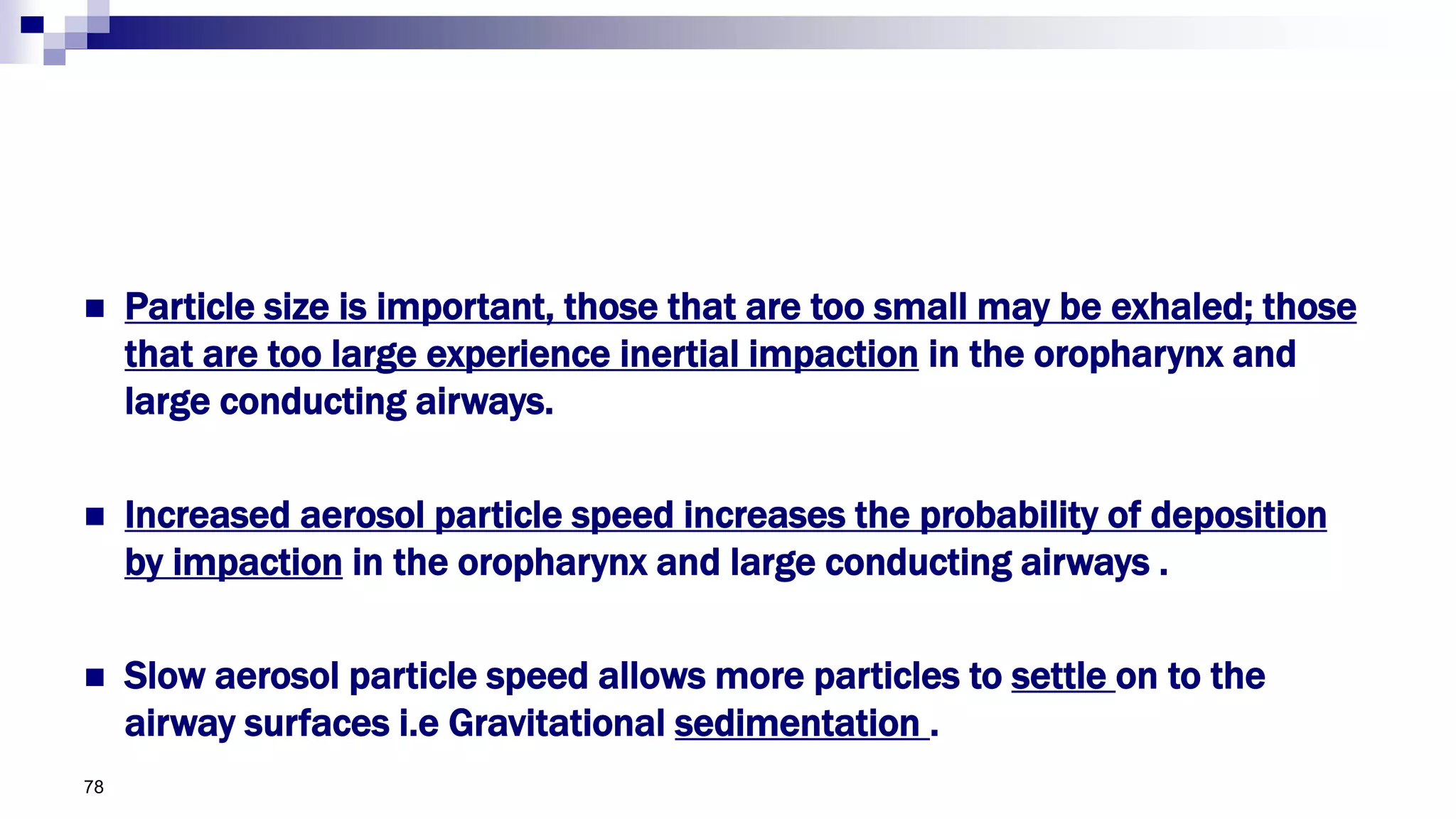
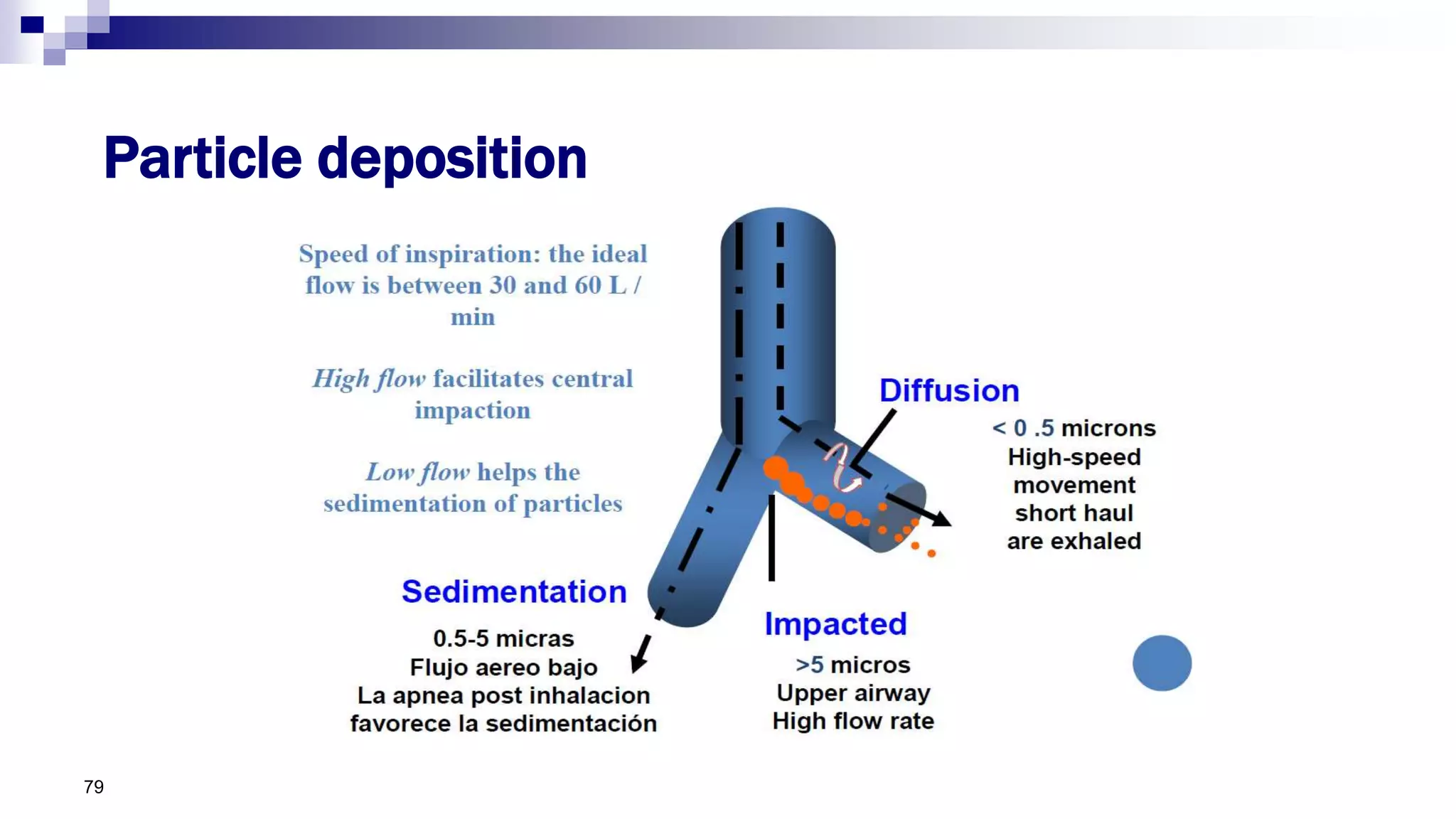
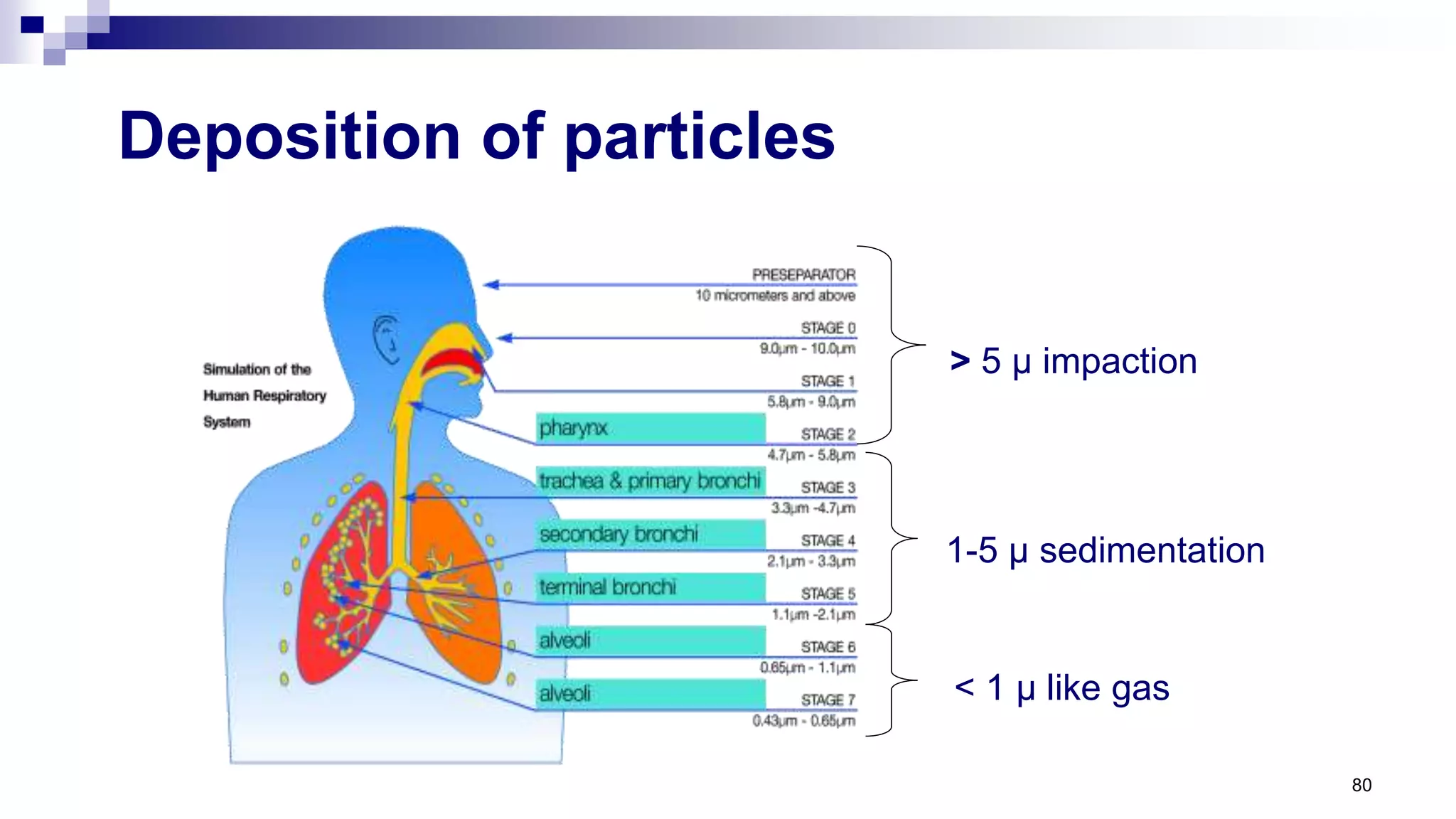
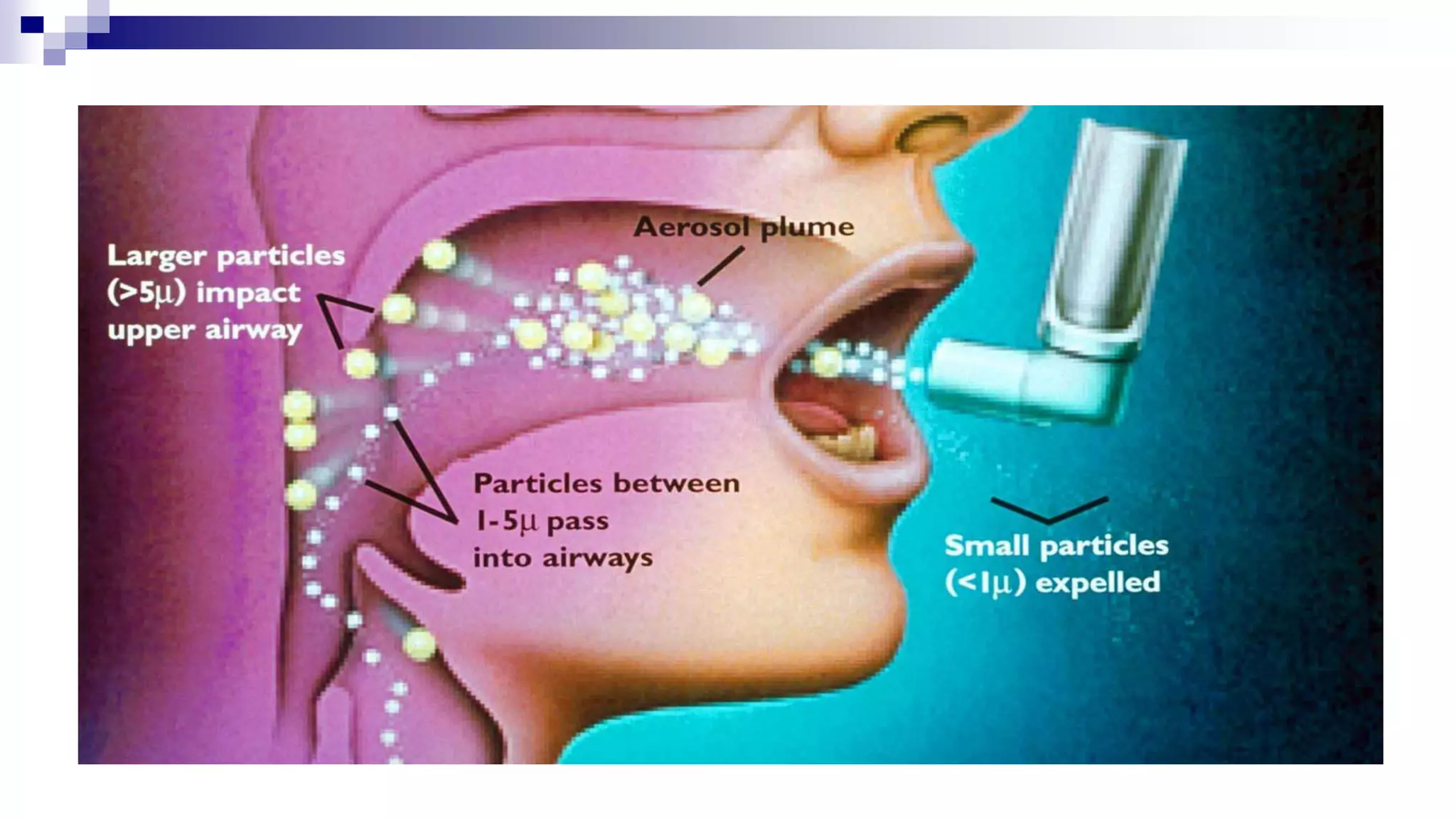
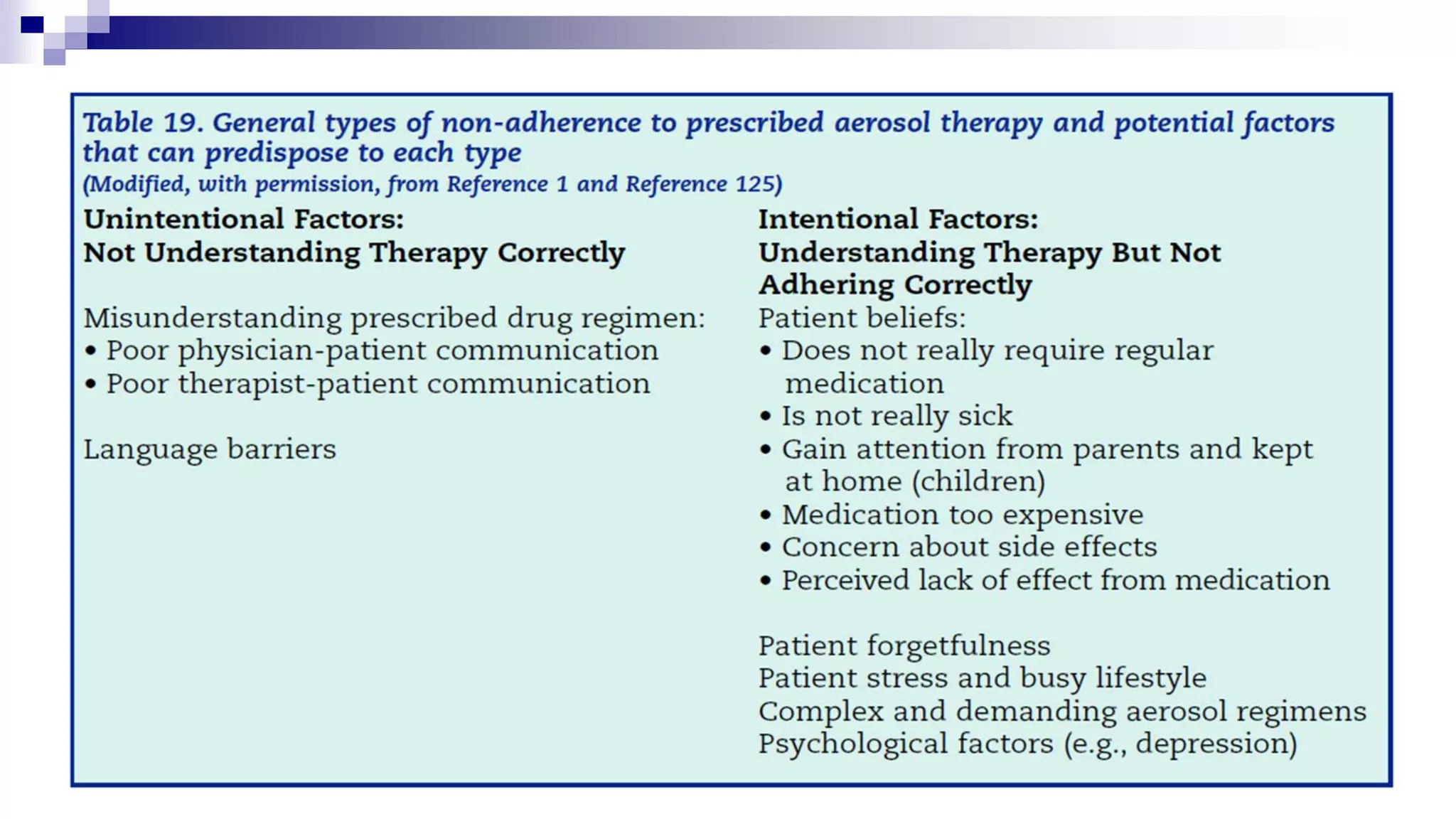
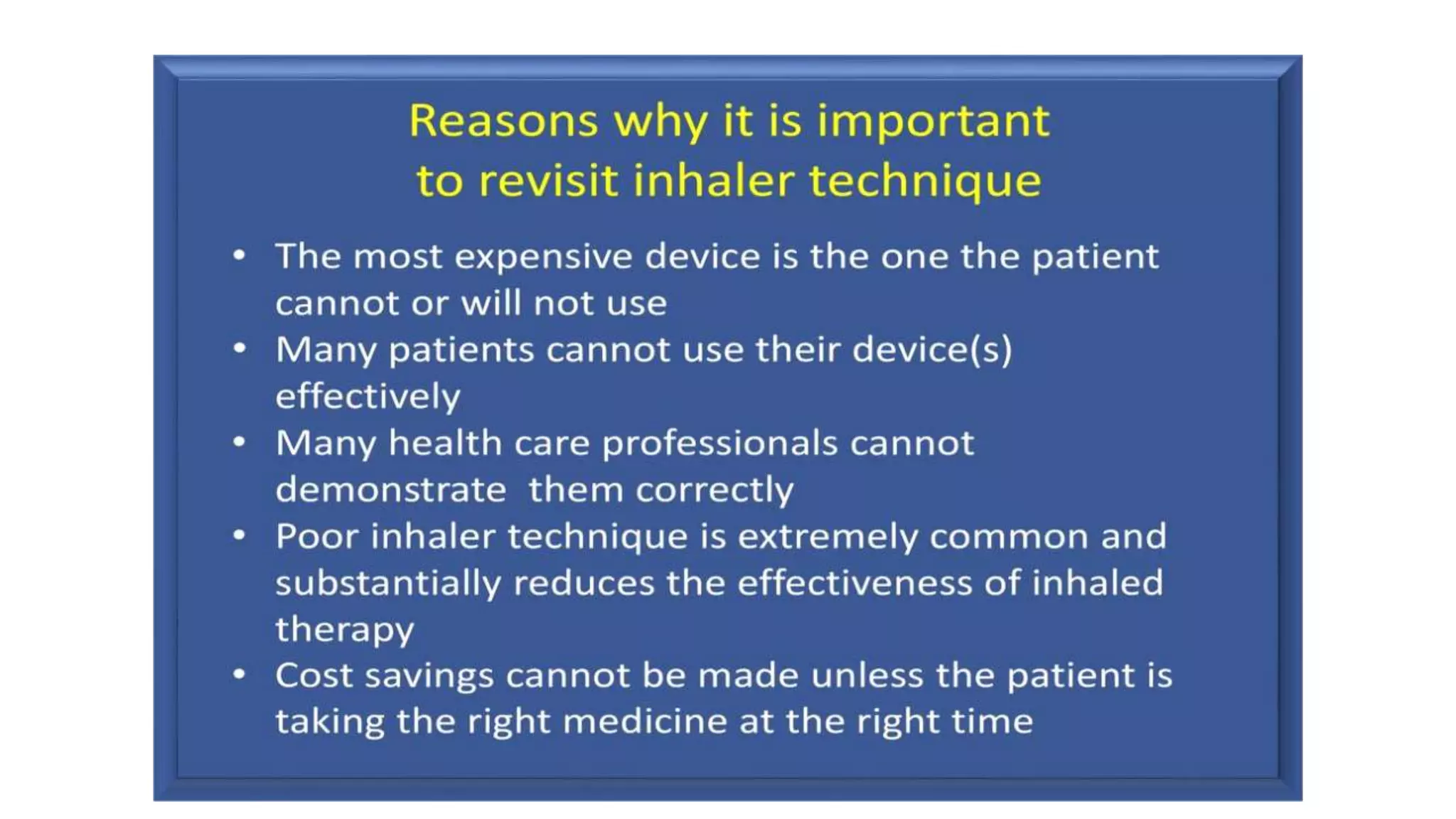
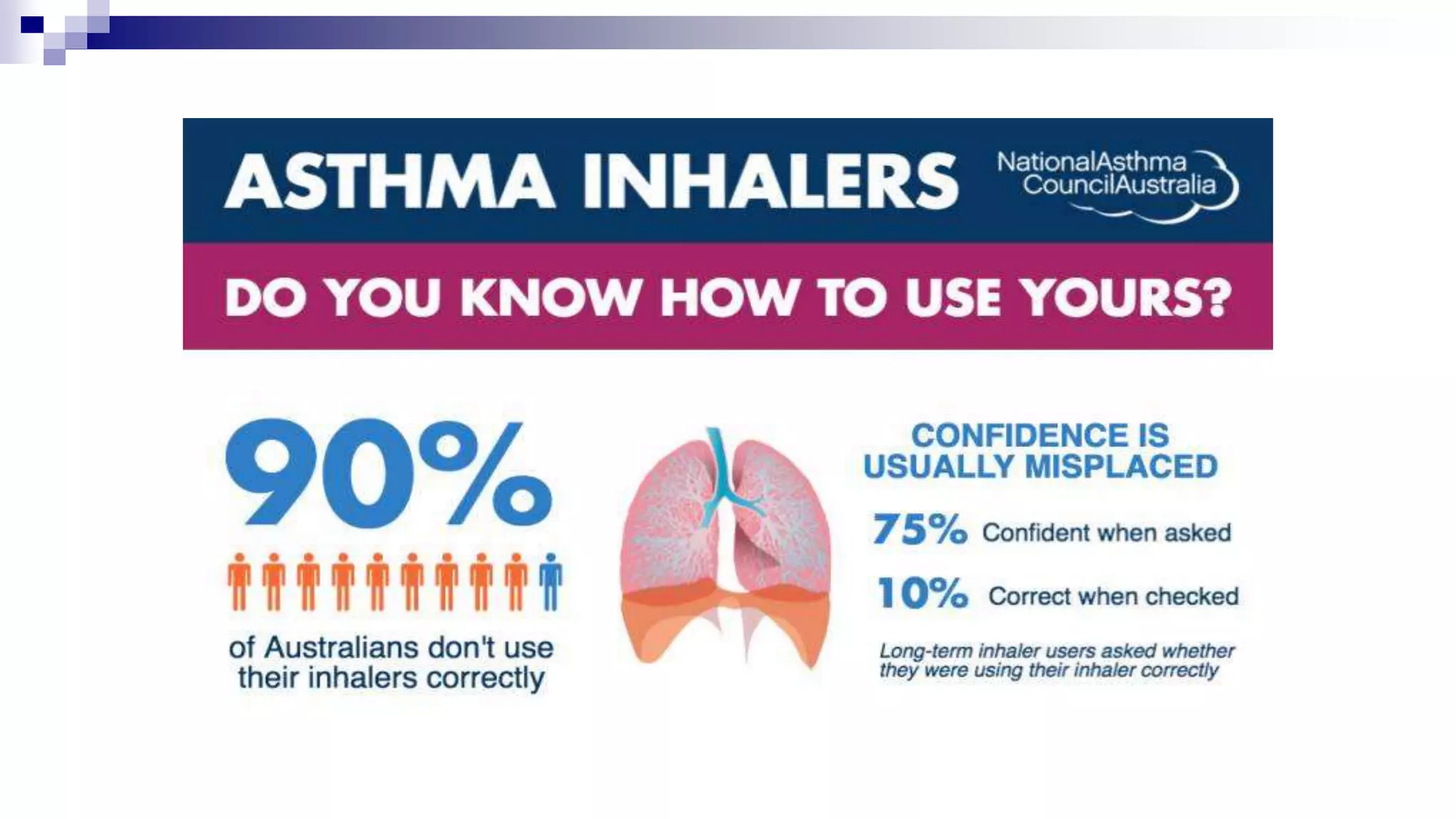
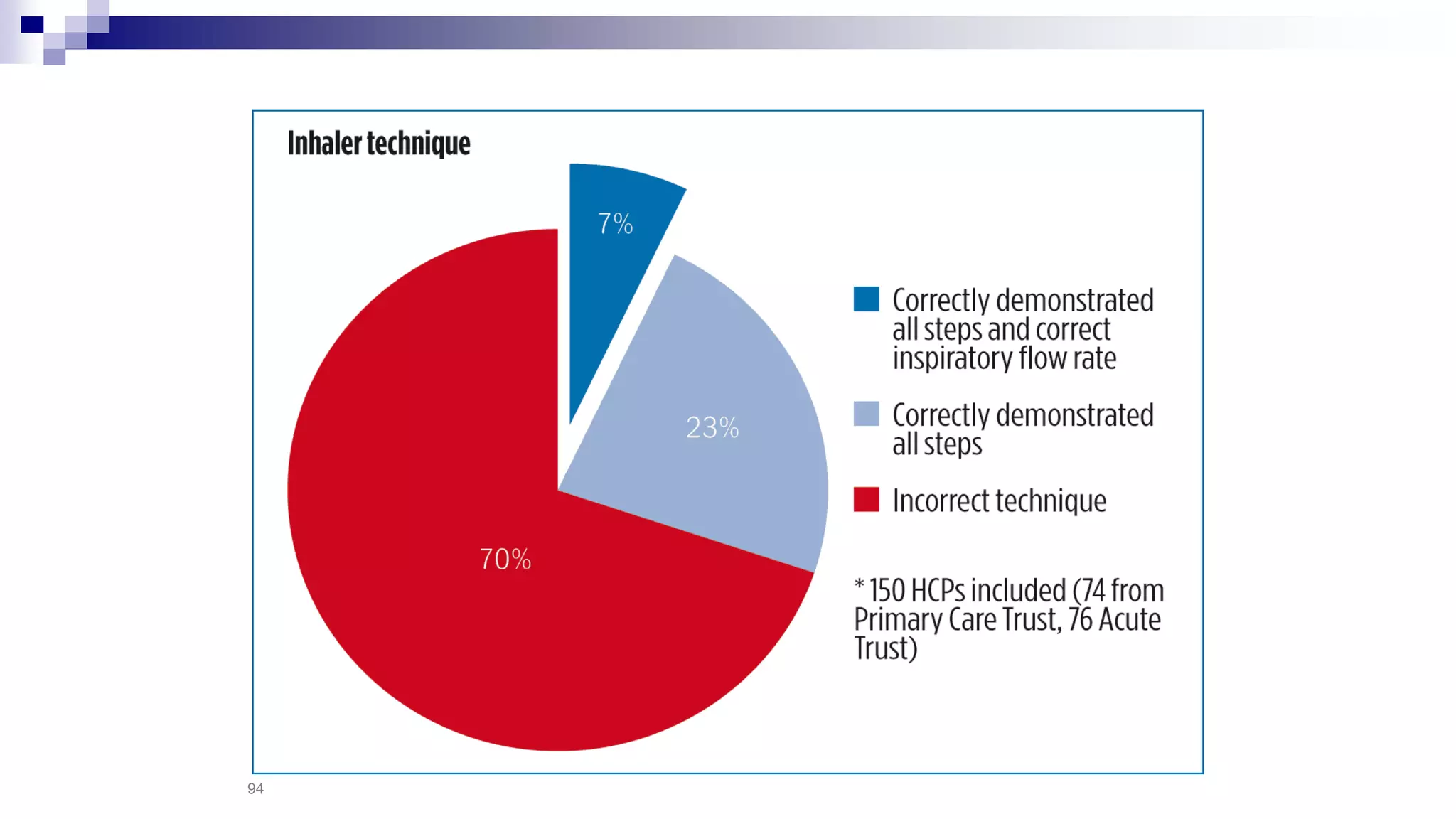
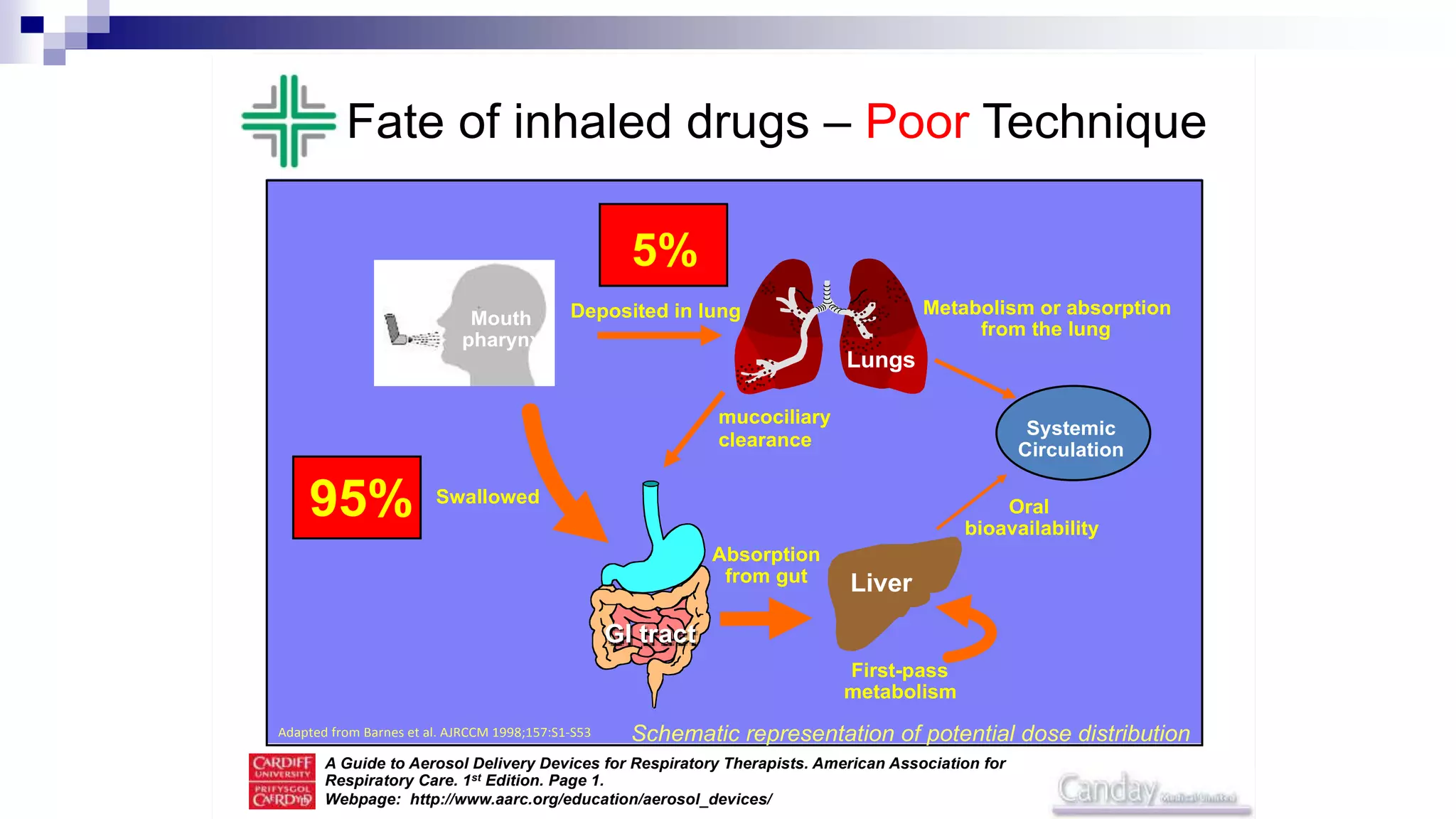
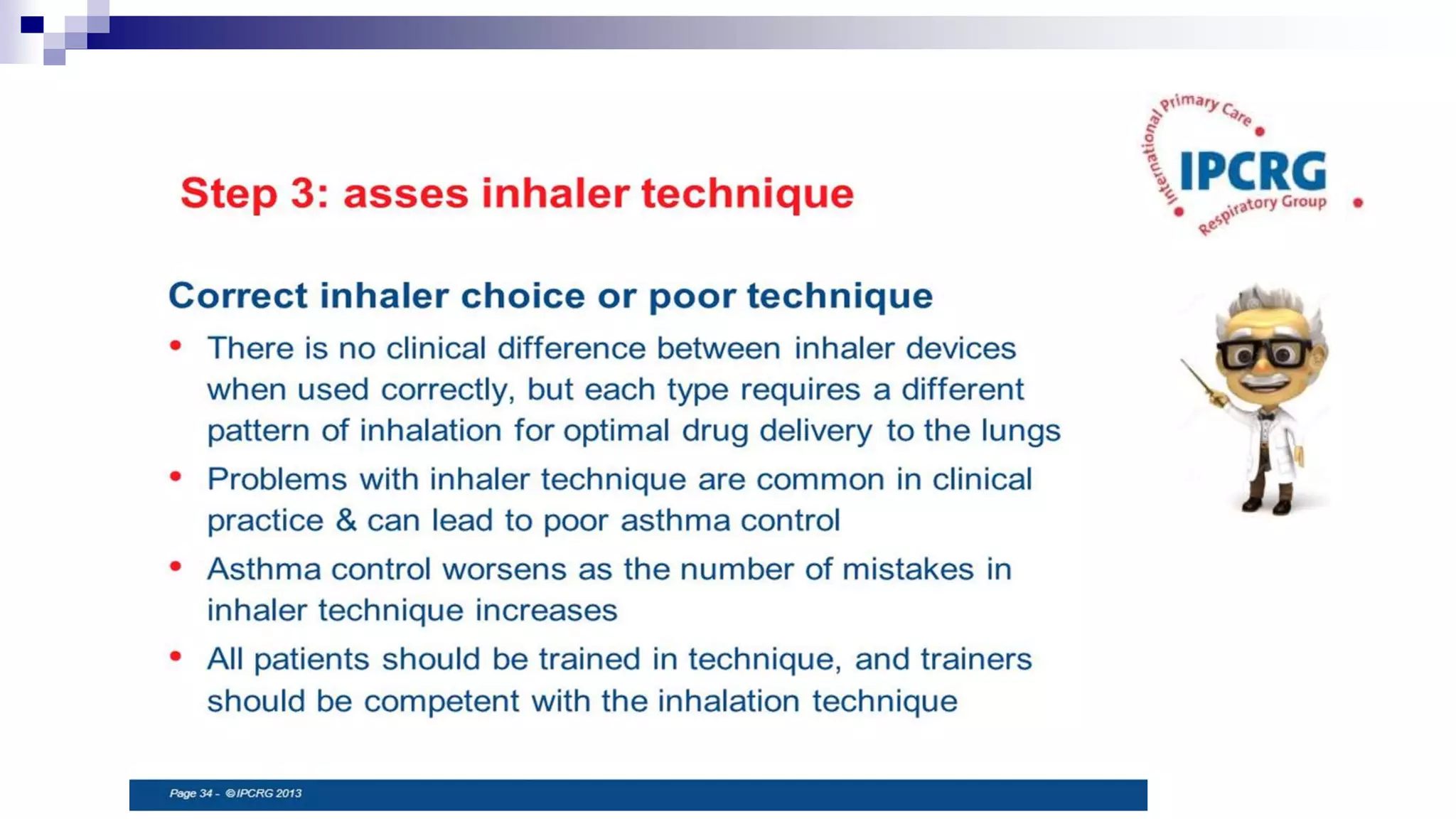
- Proper inhaler technique is important for effective delivery of medication to the lungs.