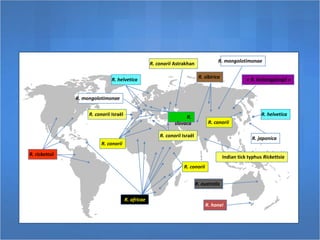
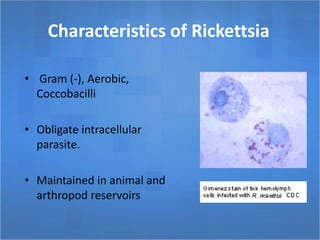
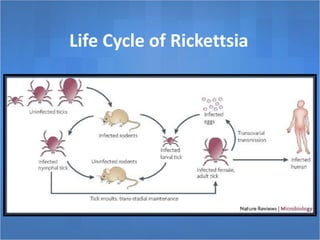
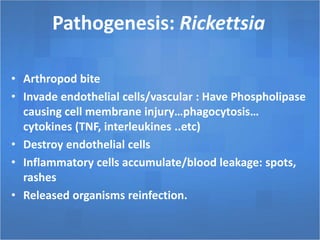
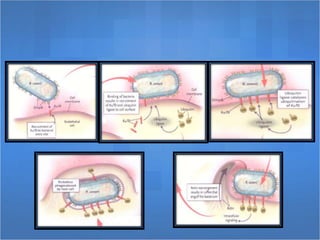
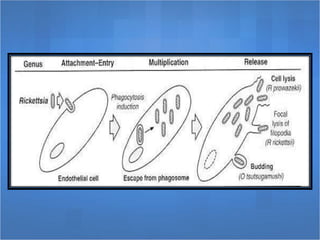
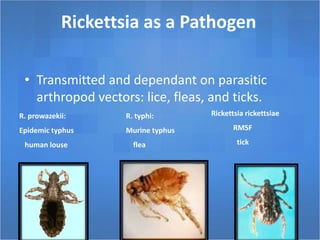
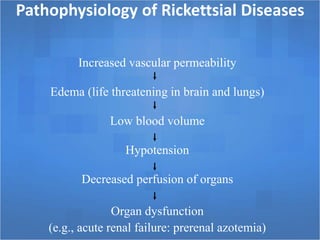
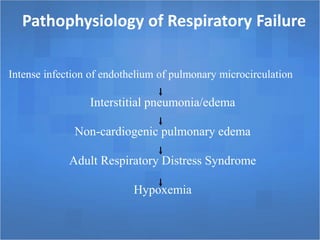
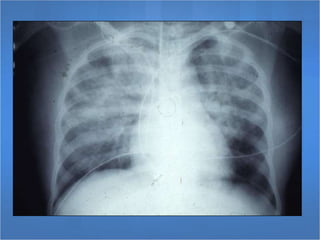
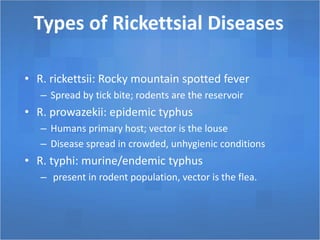
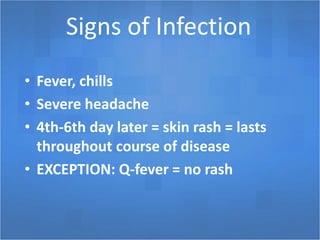
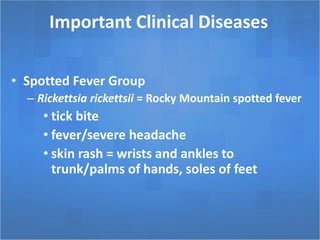
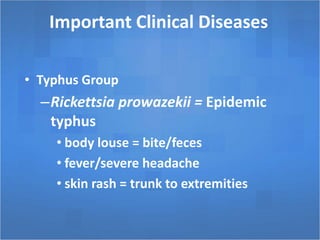
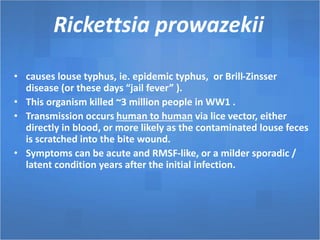
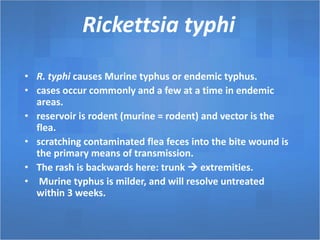
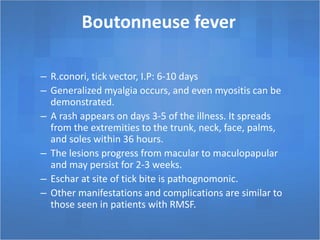
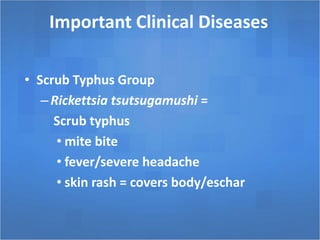
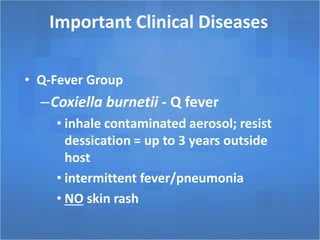
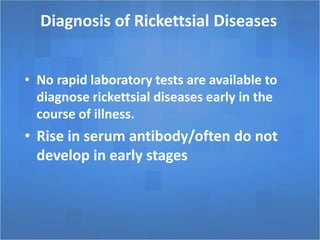
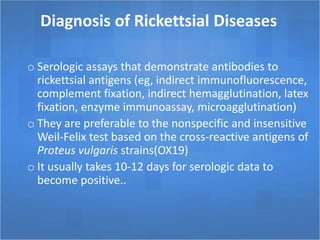
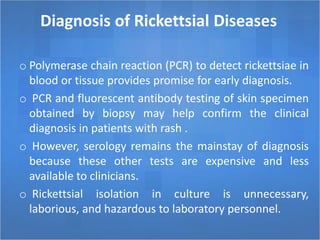
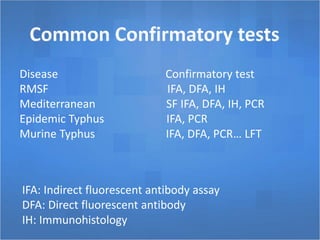
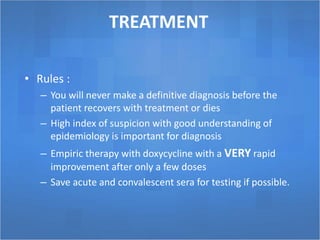
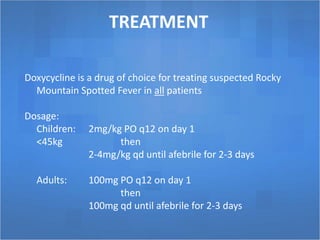
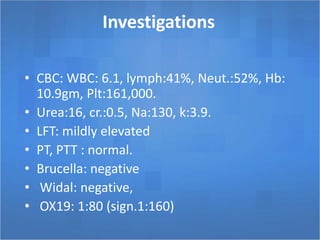
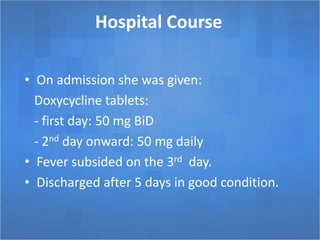
Rickettsial diseases, including Rocky Mountain spotted fever and typhus, are caused by obligate intracellular parasites transmitted through arthropod vectors like ticks, fleas, and lice. Symptoms typically include fever, severe headache, and skin rash, while diagnosis relies on serologic assays and clinical suspicion. Treatment with doxycycline is effective, and preventive measures focus on limiting exposure to ticks.