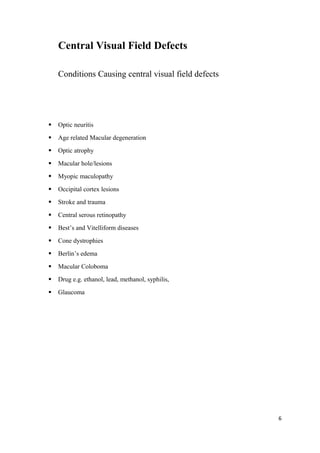
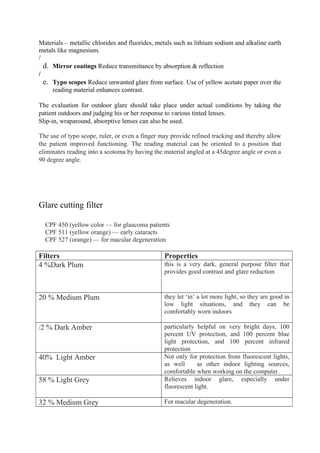
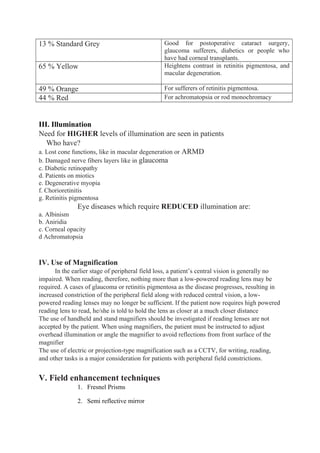
The document discusses various aspects of visual impairment, including definitions, types, and classifications based on conditions causing vision loss. It outlines rehabilitation methods to enhance the independence and quality of life for visually impaired individuals, emphasizing a multidisciplinary approach involving ophthalmologists, optometrists, and rehabilitation specialists. Additionally, it details low vision aids and therapies aimed at maximizing visual function and addressing the specific needs of patients with different types of visual impairment.