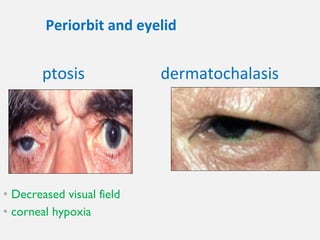
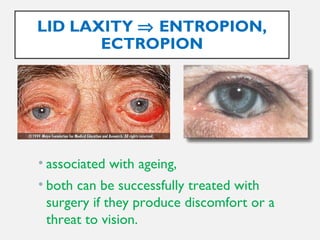
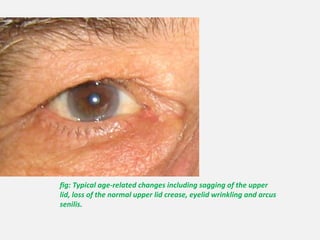
This document discusses various age-related changes that occur in the eye and visual system. It notes decreased visual field and corneal sensitivity with age. The eyelids show signs of atrophy, wrinkling, and misalignment. The conjunctiva thins and produces fewer tears. The lens thickens and becomes less transparent, increasing nearsightedness. The vitreous shrinks and detaches from the retina more easily. The retina has poorer response to light and contrast sensitivity. Overall, aging reduces visual acuity, especially for moving targets, and increases the need for brighter lighting.