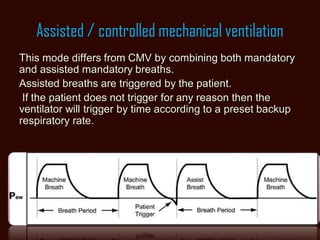
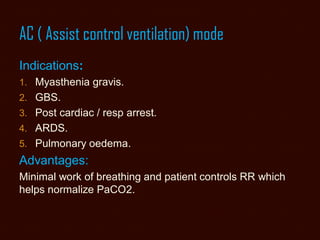
The document explains key concepts of mechanical ventilation in an ICU setting, focusing on ventilator variables, modes, and their clinical applications. It details the five types of ventilator variables: control, trigger, limit, cycle, and baseline, as well as various breath types and ventilation modes such as CMV, A/C, SIMV, and pressure support. Finally, it discusses the advantages and disadvantages of each mode, emphasizing the importance of proper ventilator settings to ensure patient safety and comfort.