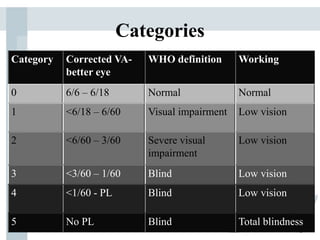
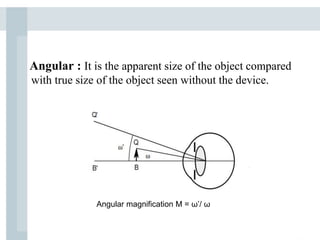
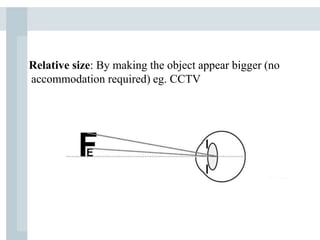
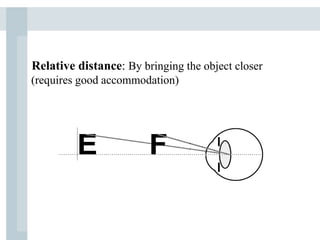
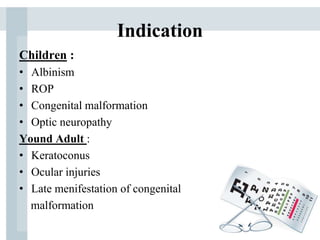
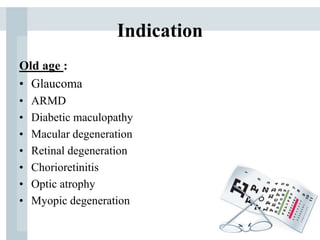
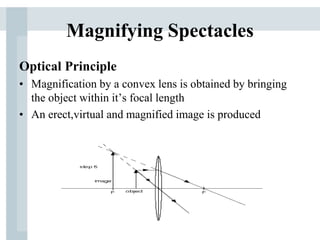
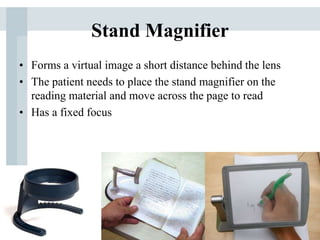
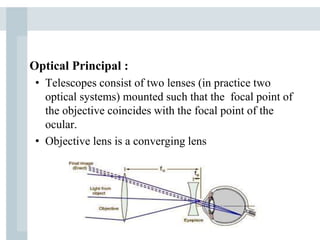
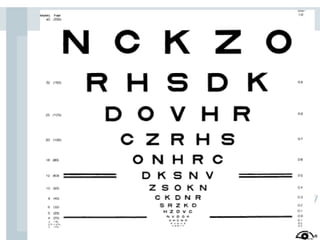
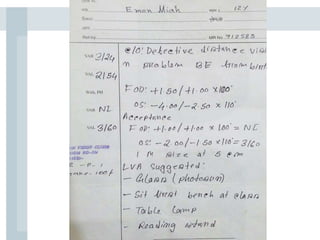
This document discusses low vision aids and their use for people with low vision. It defines low vision as visual acuity between 6/18 and 3/60 in the better eye after correction, or a field of vision between 20 to 30 degrees. Common causes of low vision include macular degeneration, glaucoma, and diabetic retinopathy. Optical low vision aids like magnifying spectacles, hand magnifiers, and telescopes use magnification to improve vision. Non-optical aids include increased lighting, contrast enhancement, and electronic magnifiers. Proper evaluation and prescribing of low vision aids depends on the patient's needs, vision status, and motivation. The goal is to prescribe simple, portable devices to help low vision