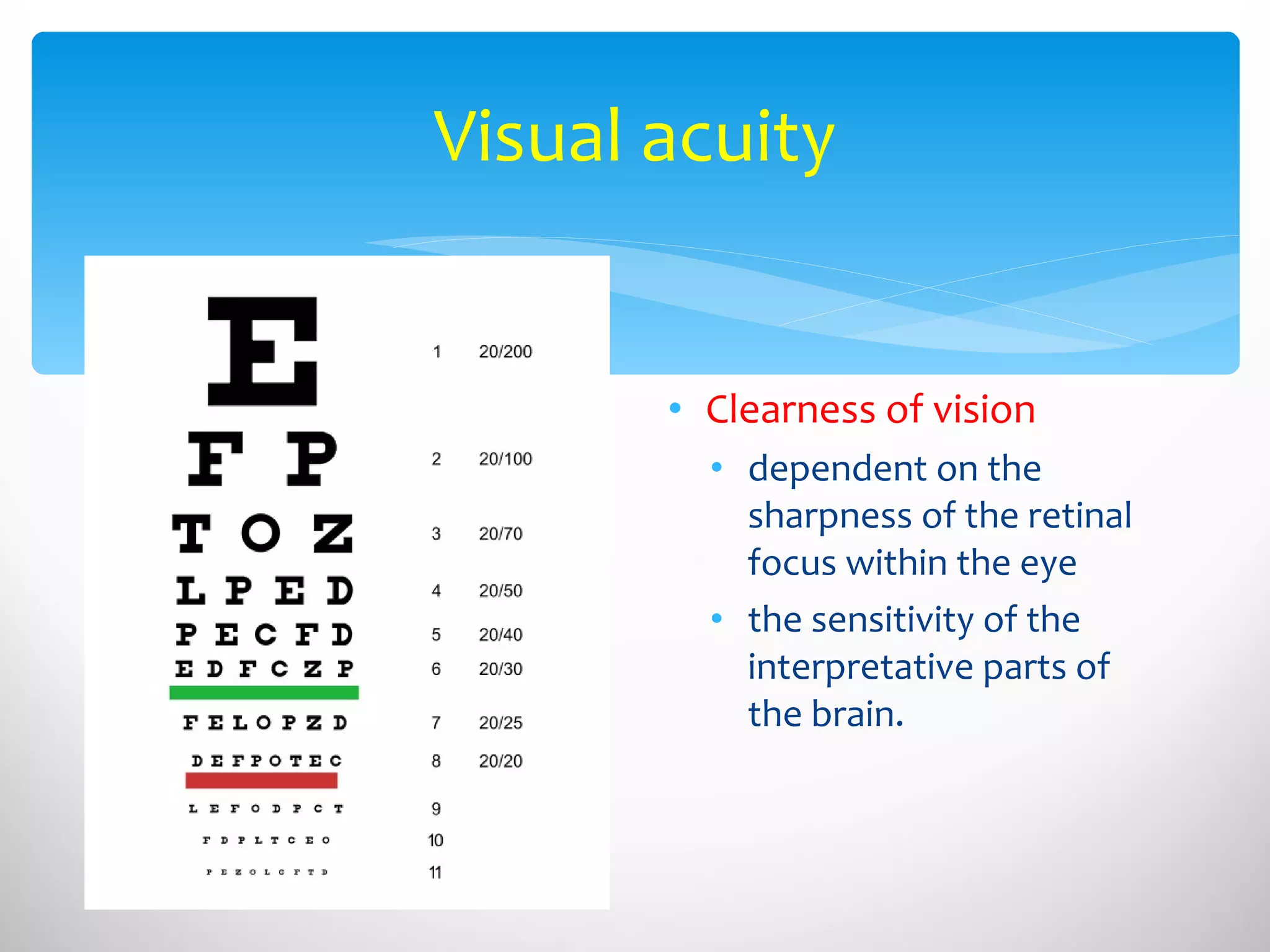
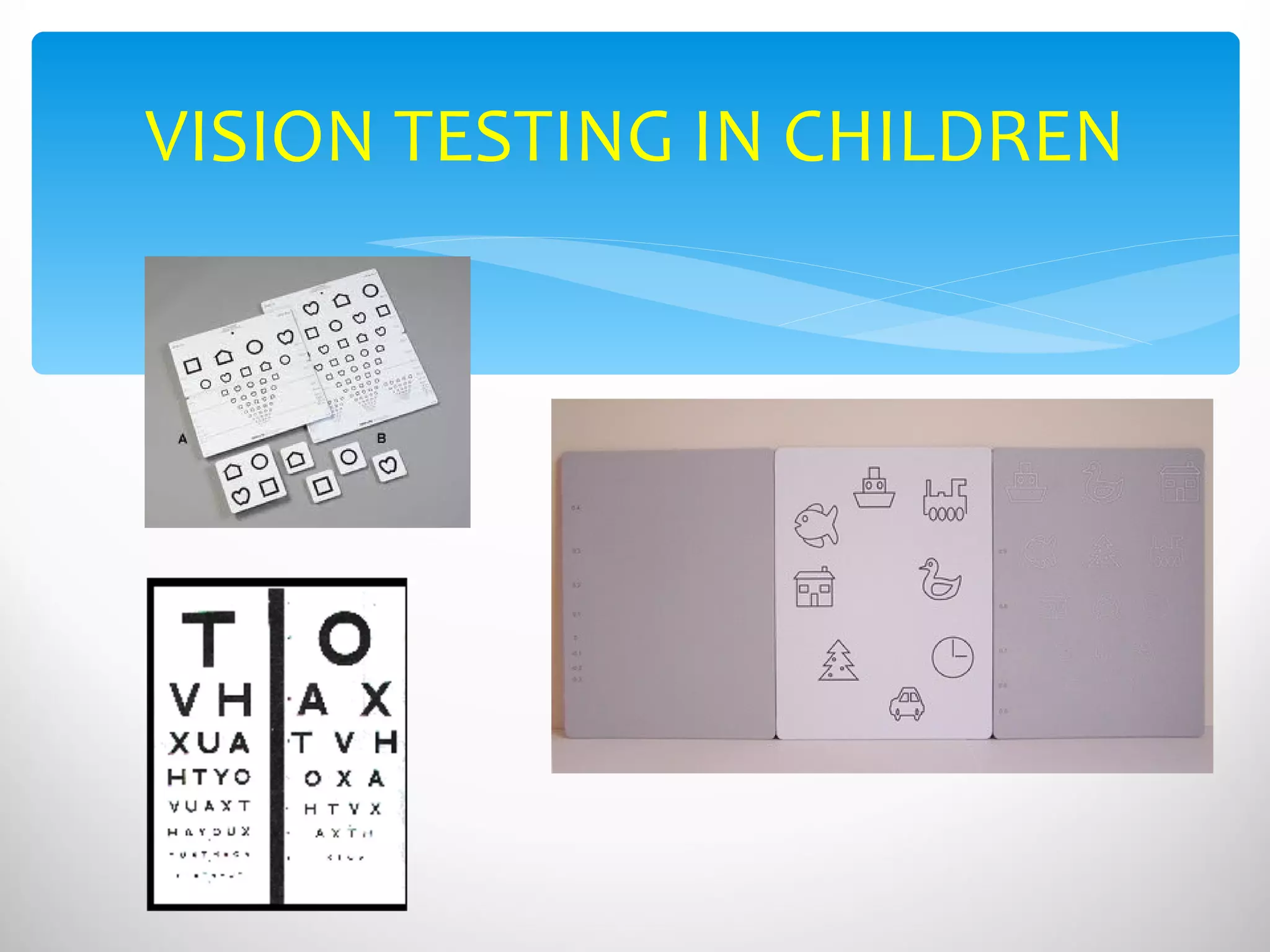
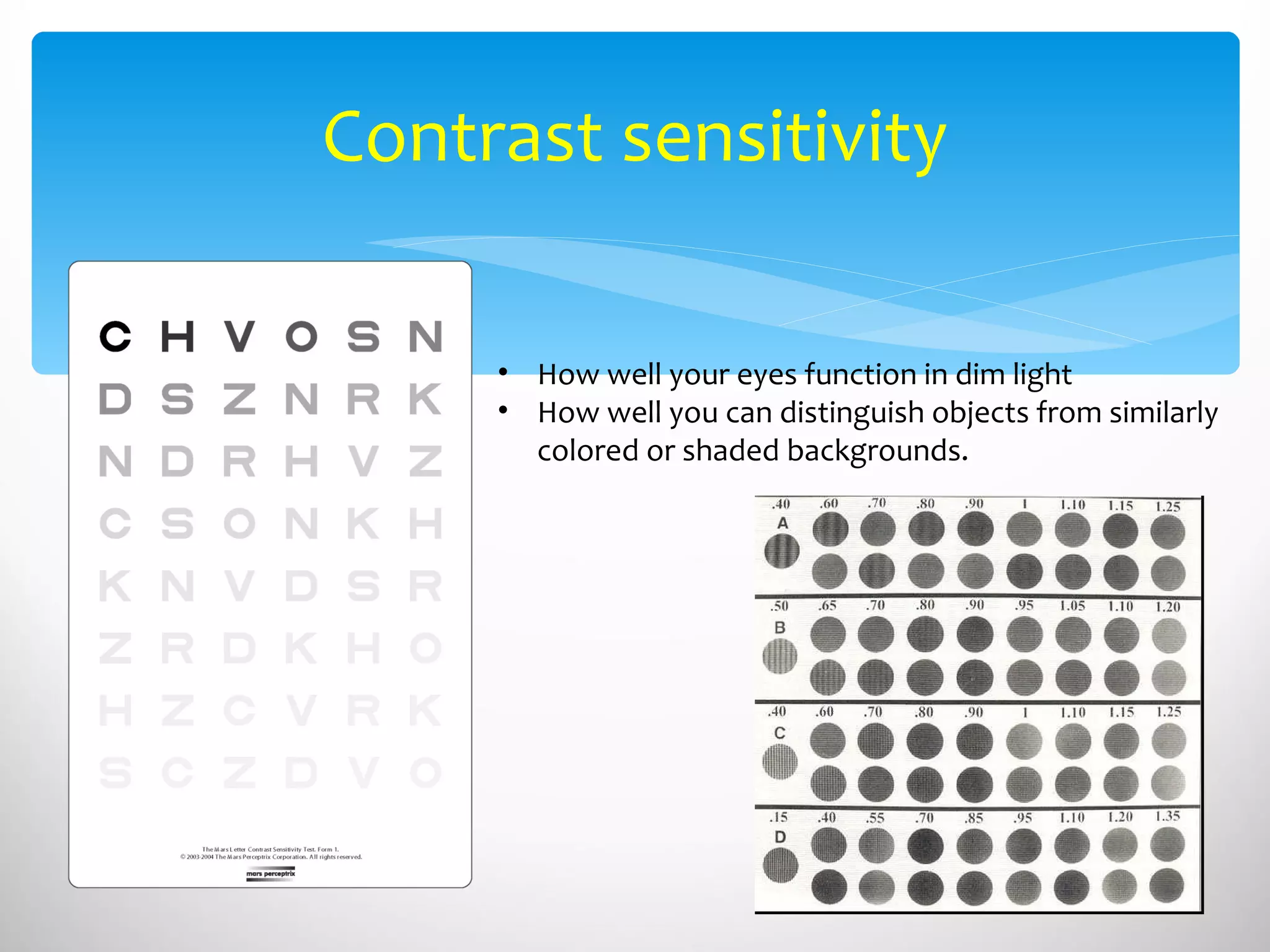
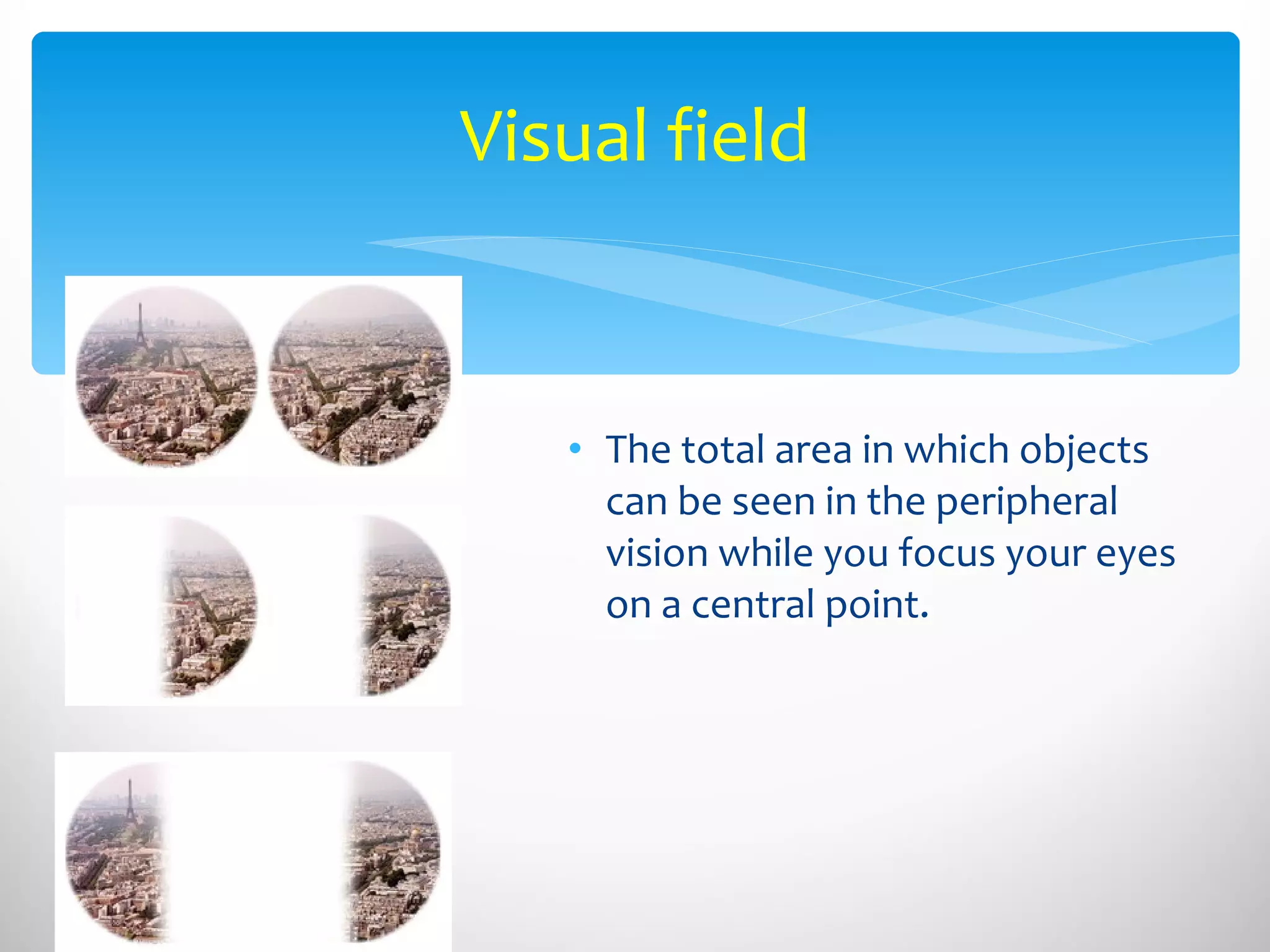
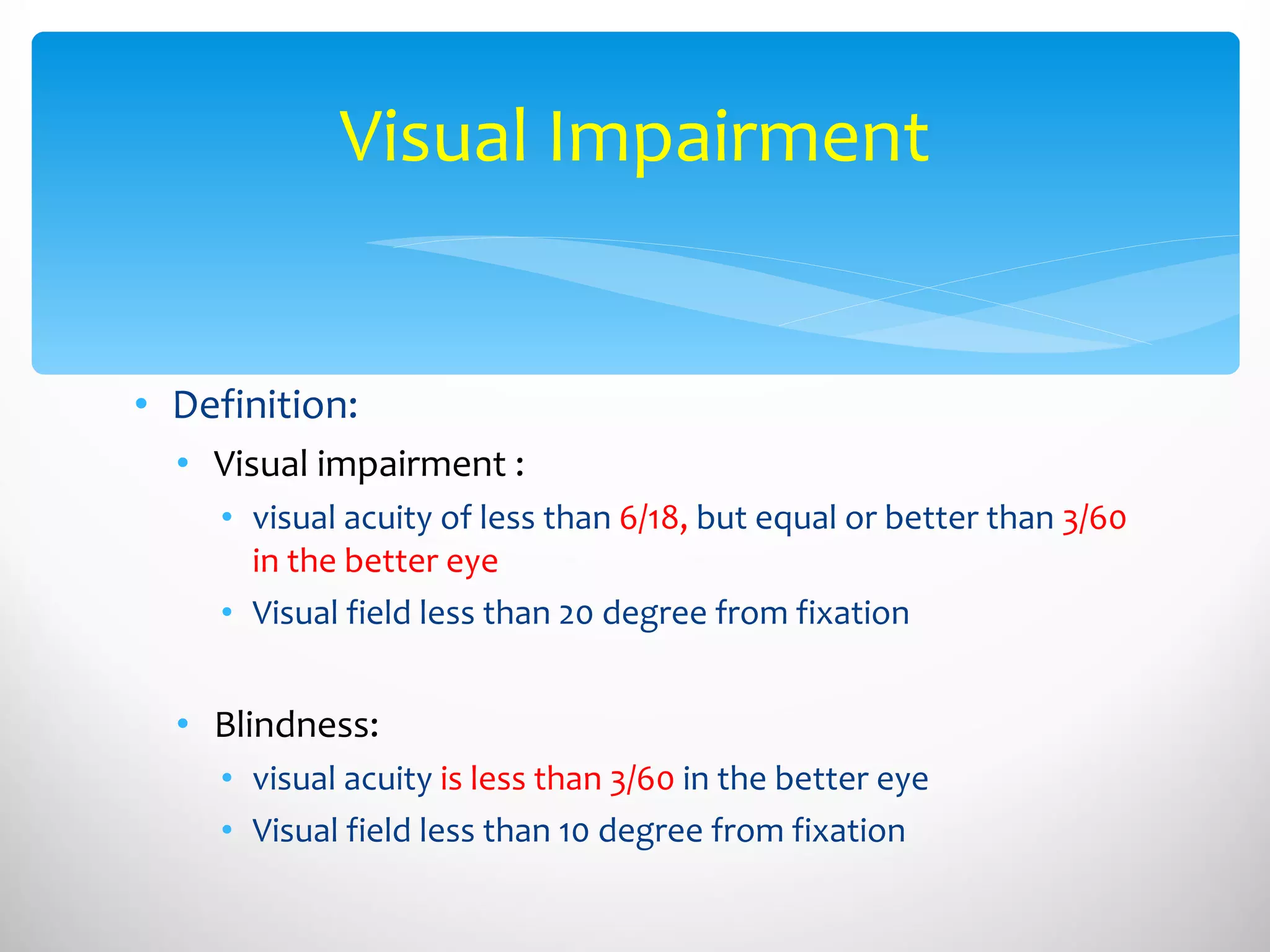
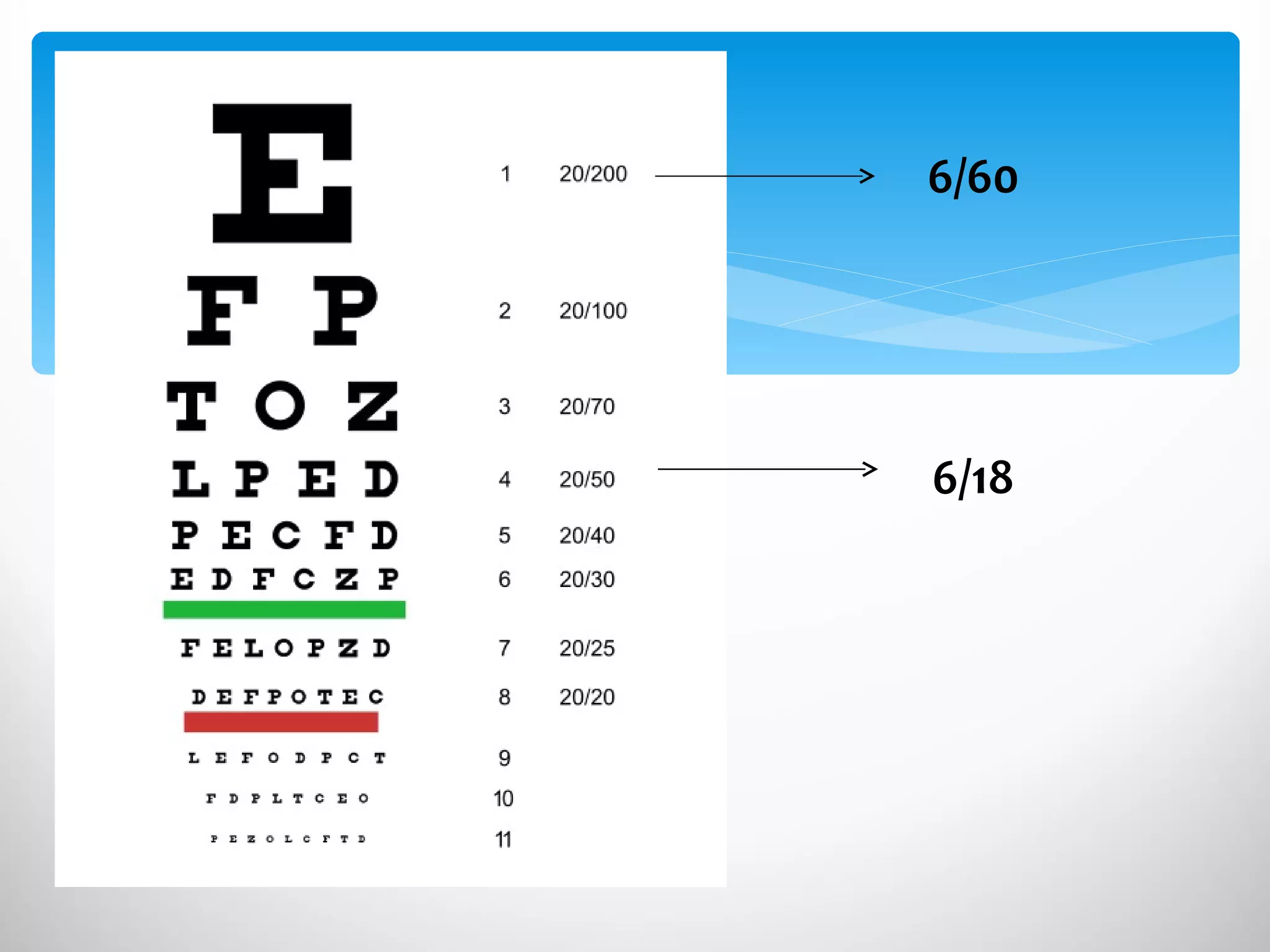
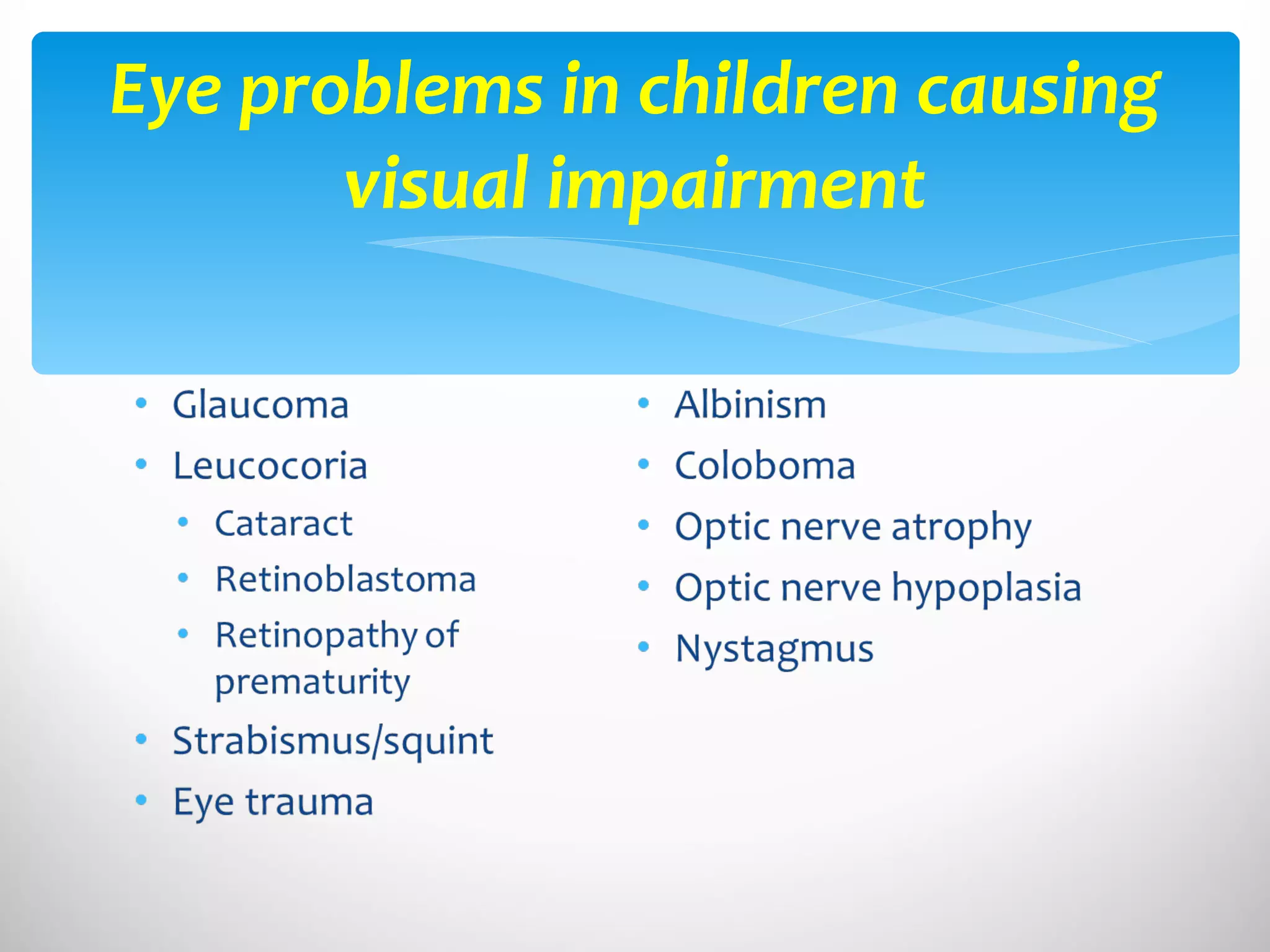
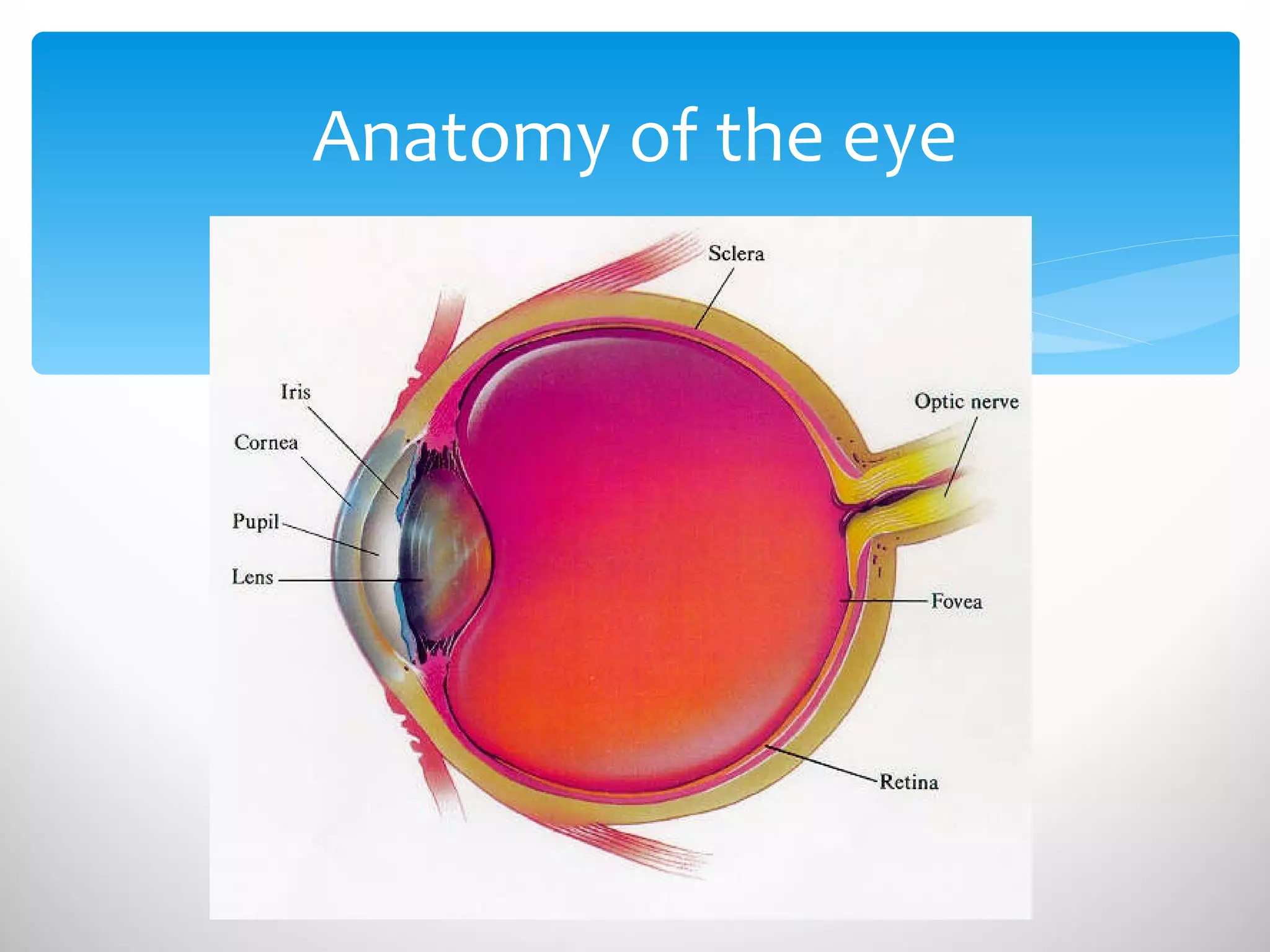
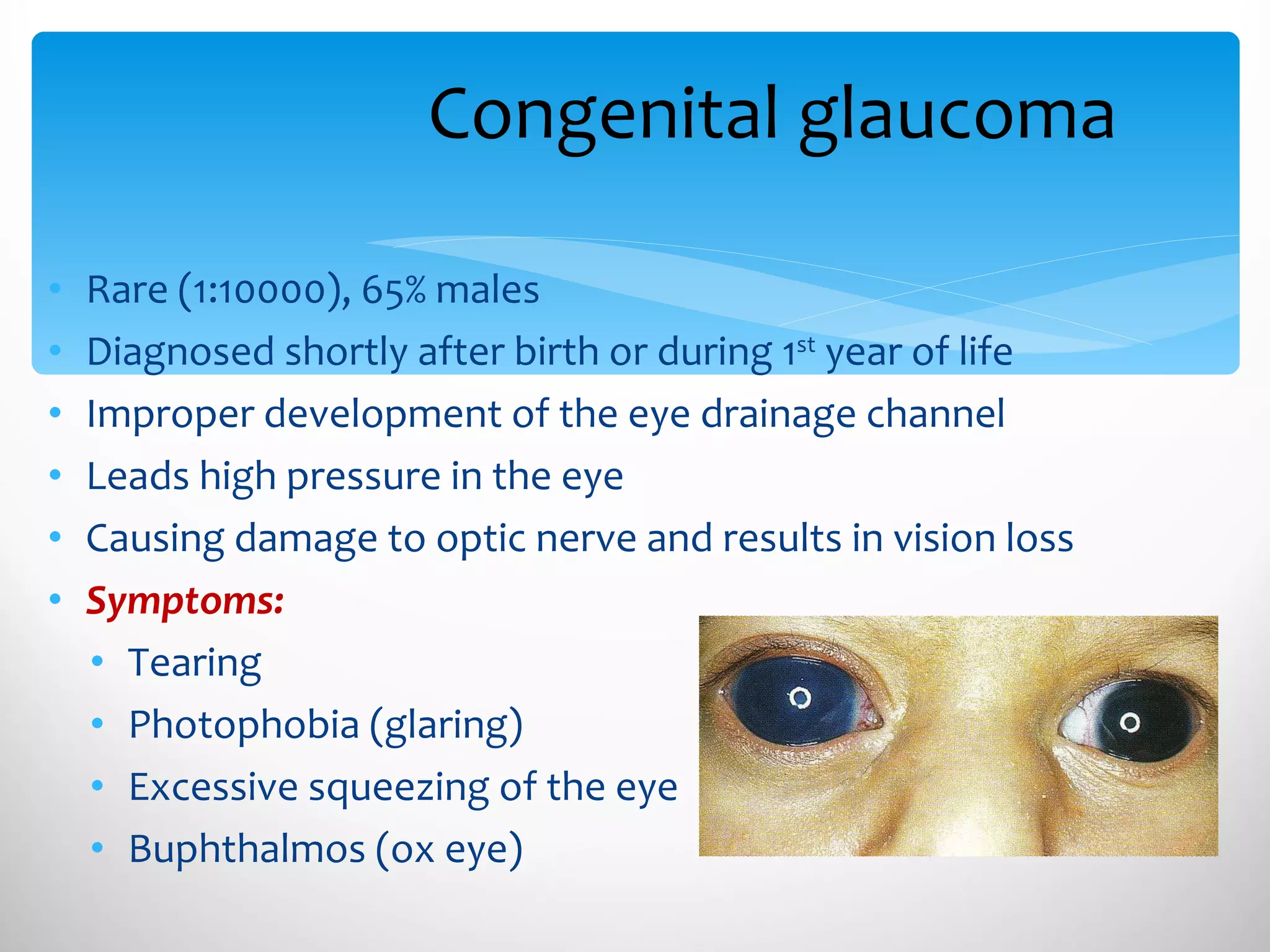
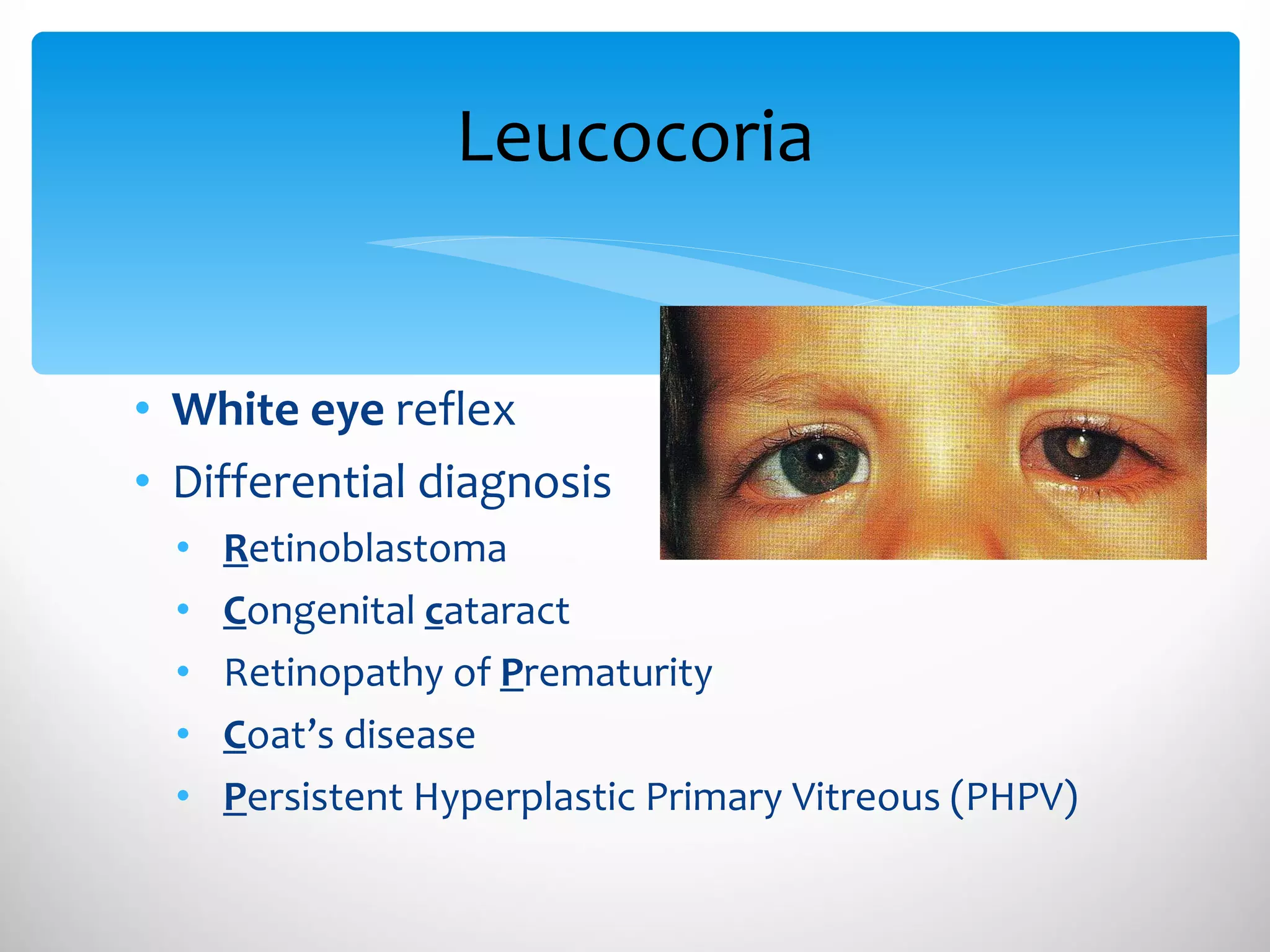
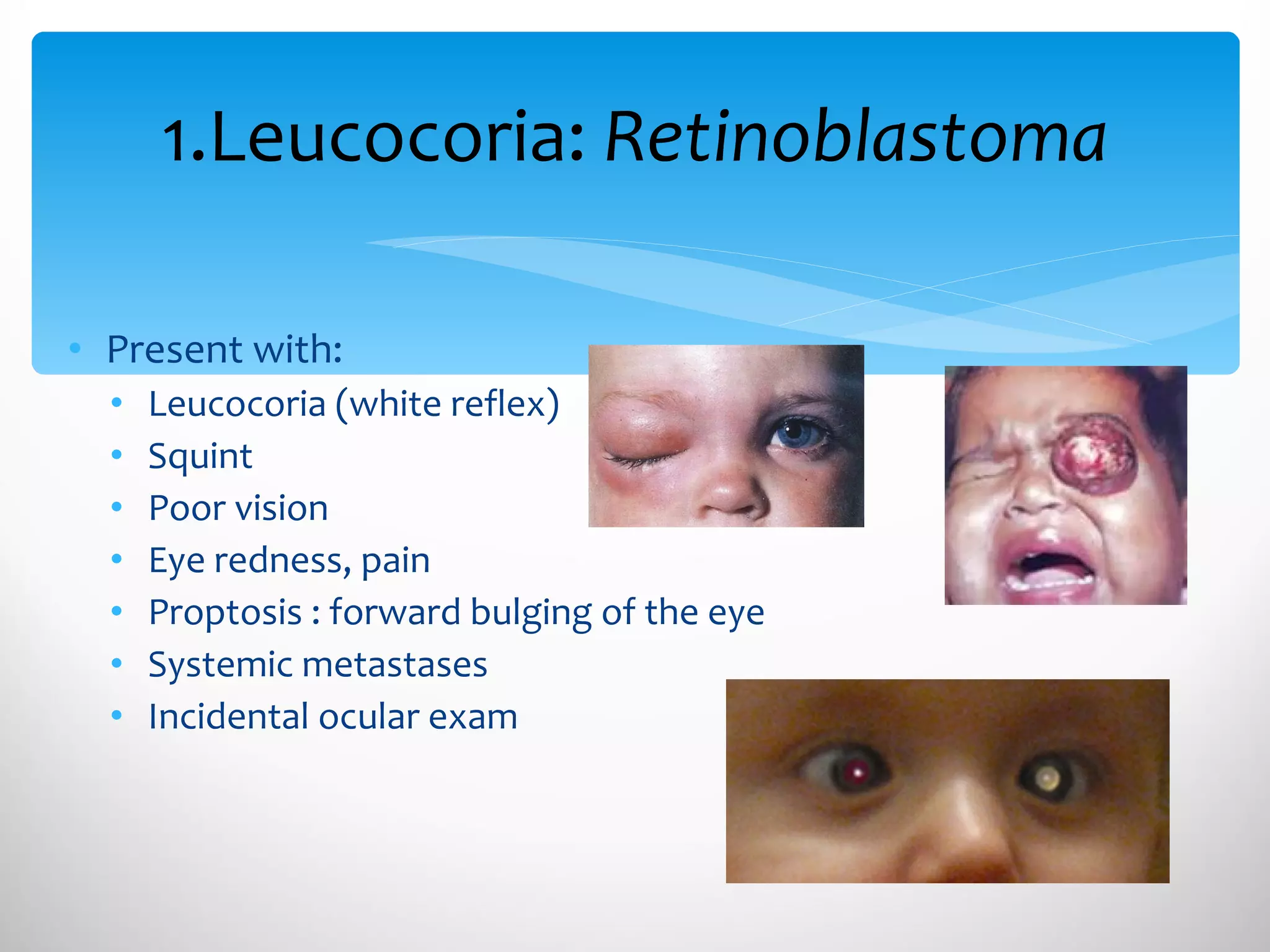
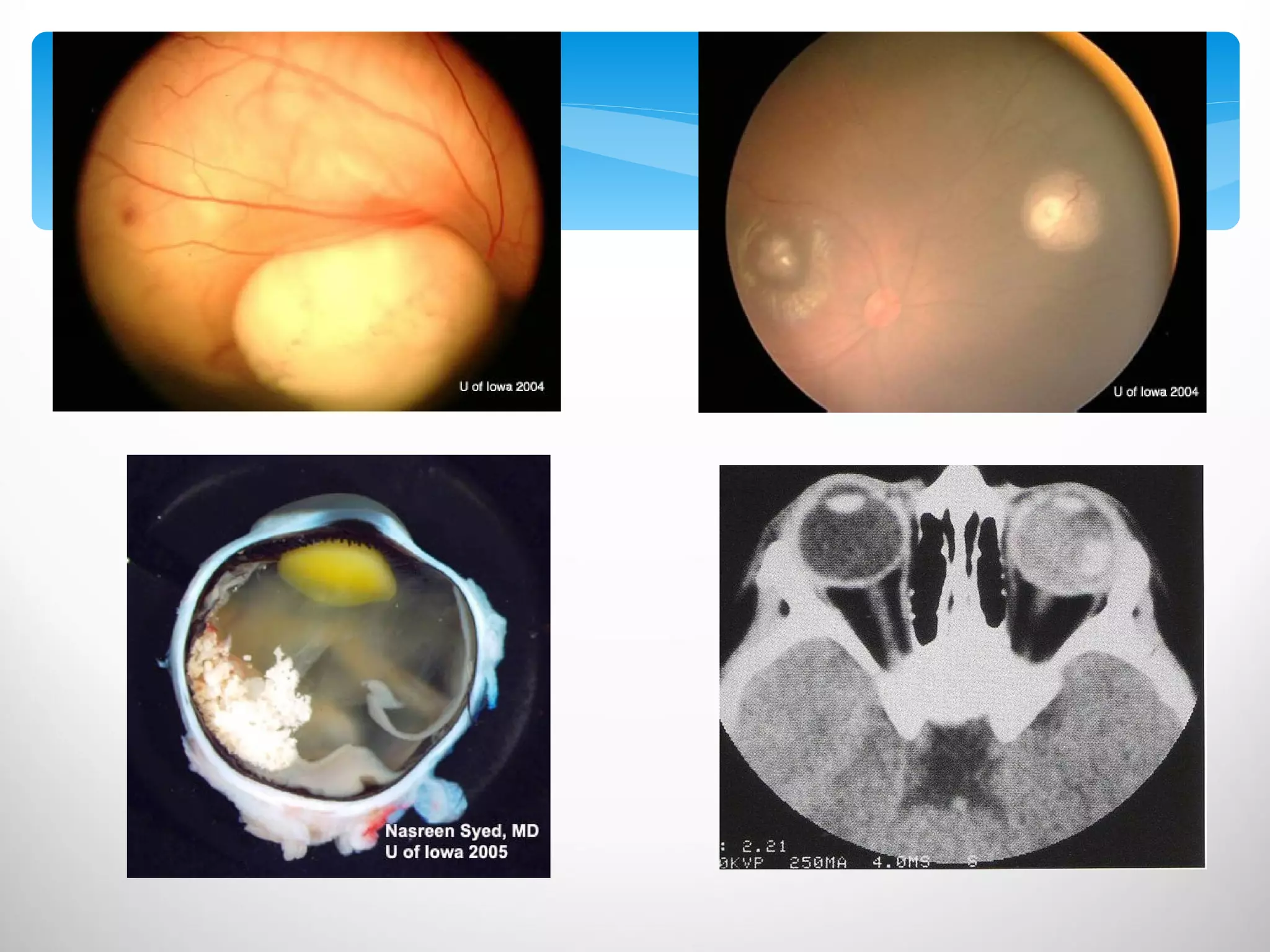
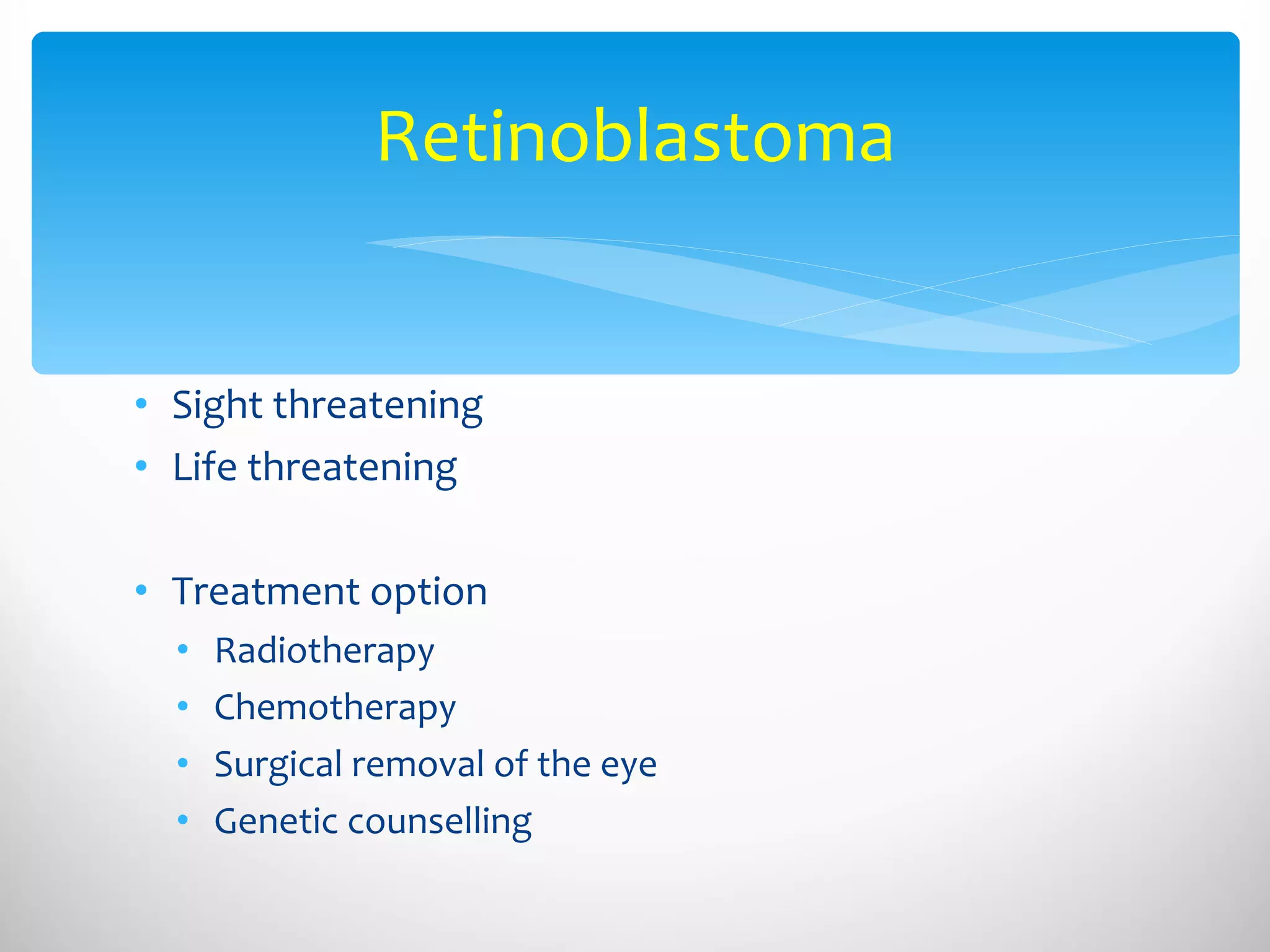
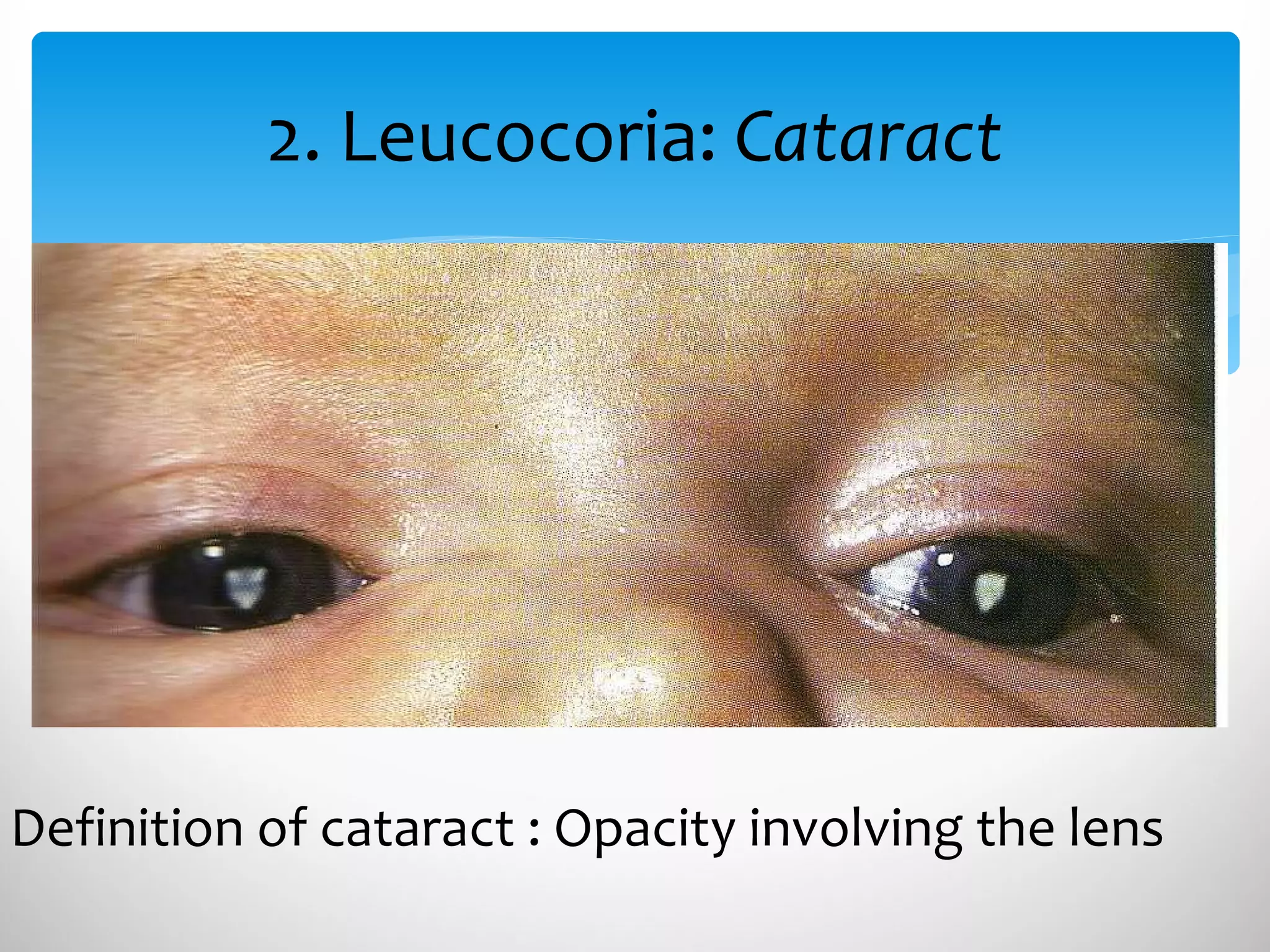
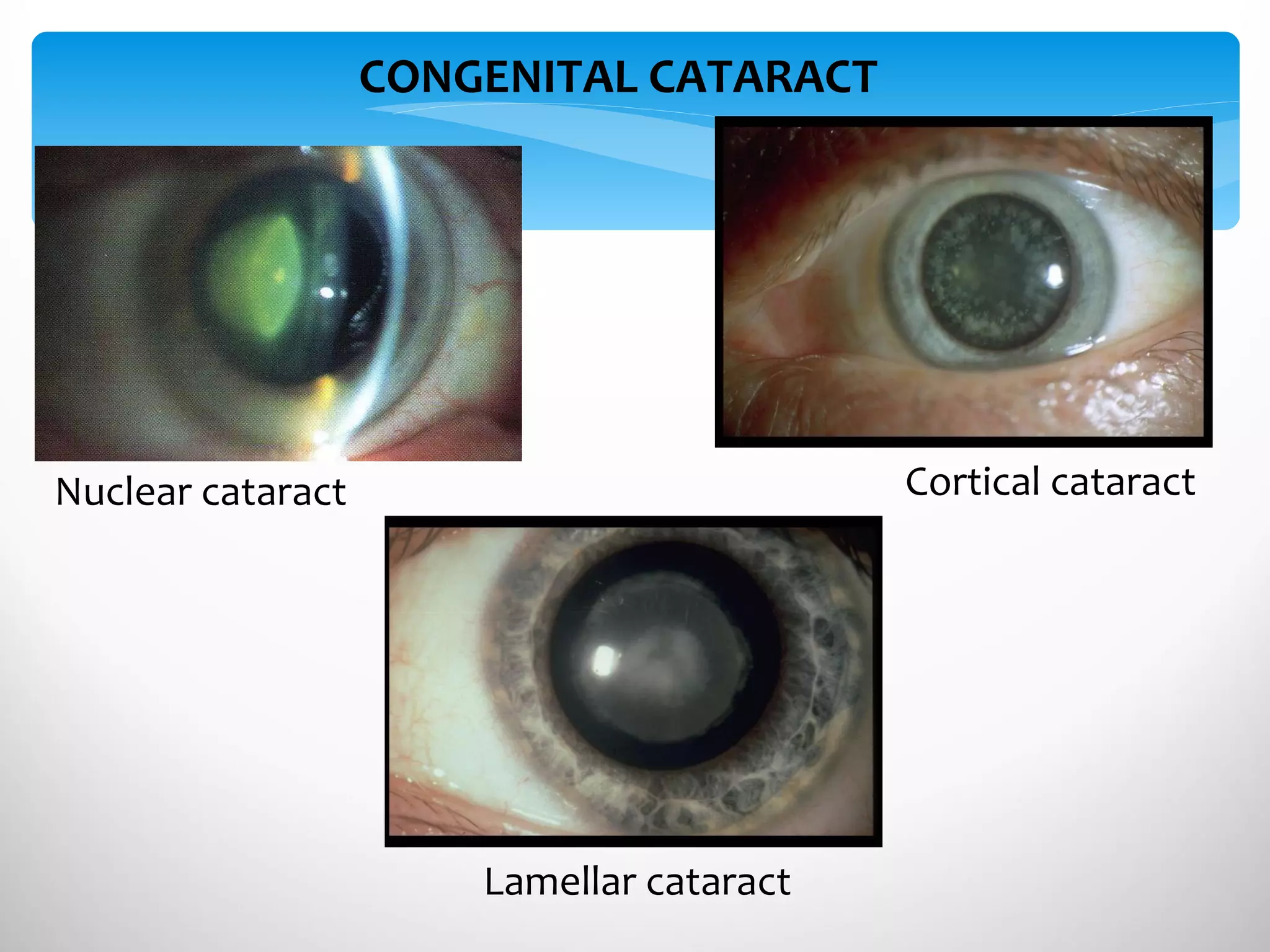
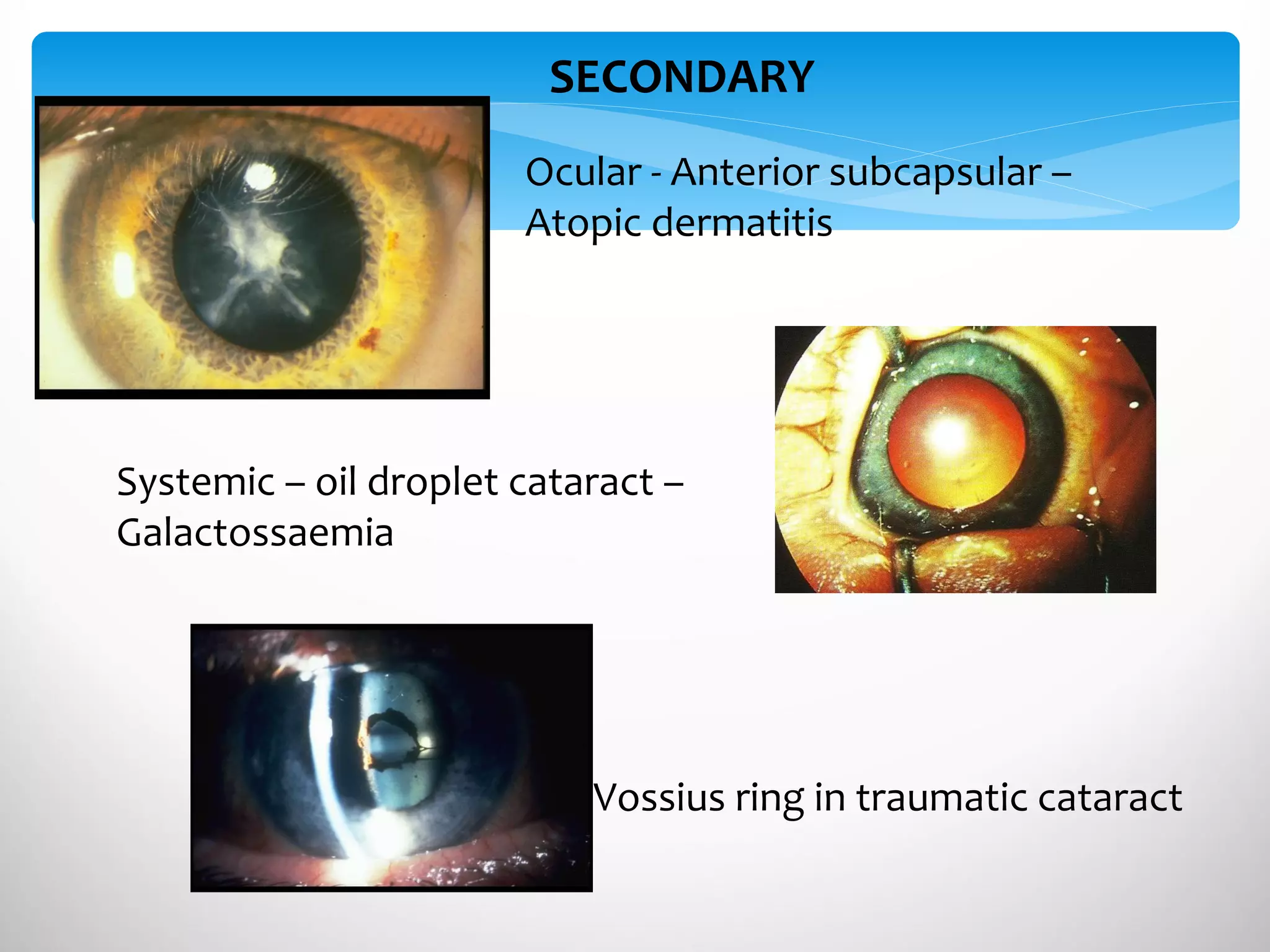
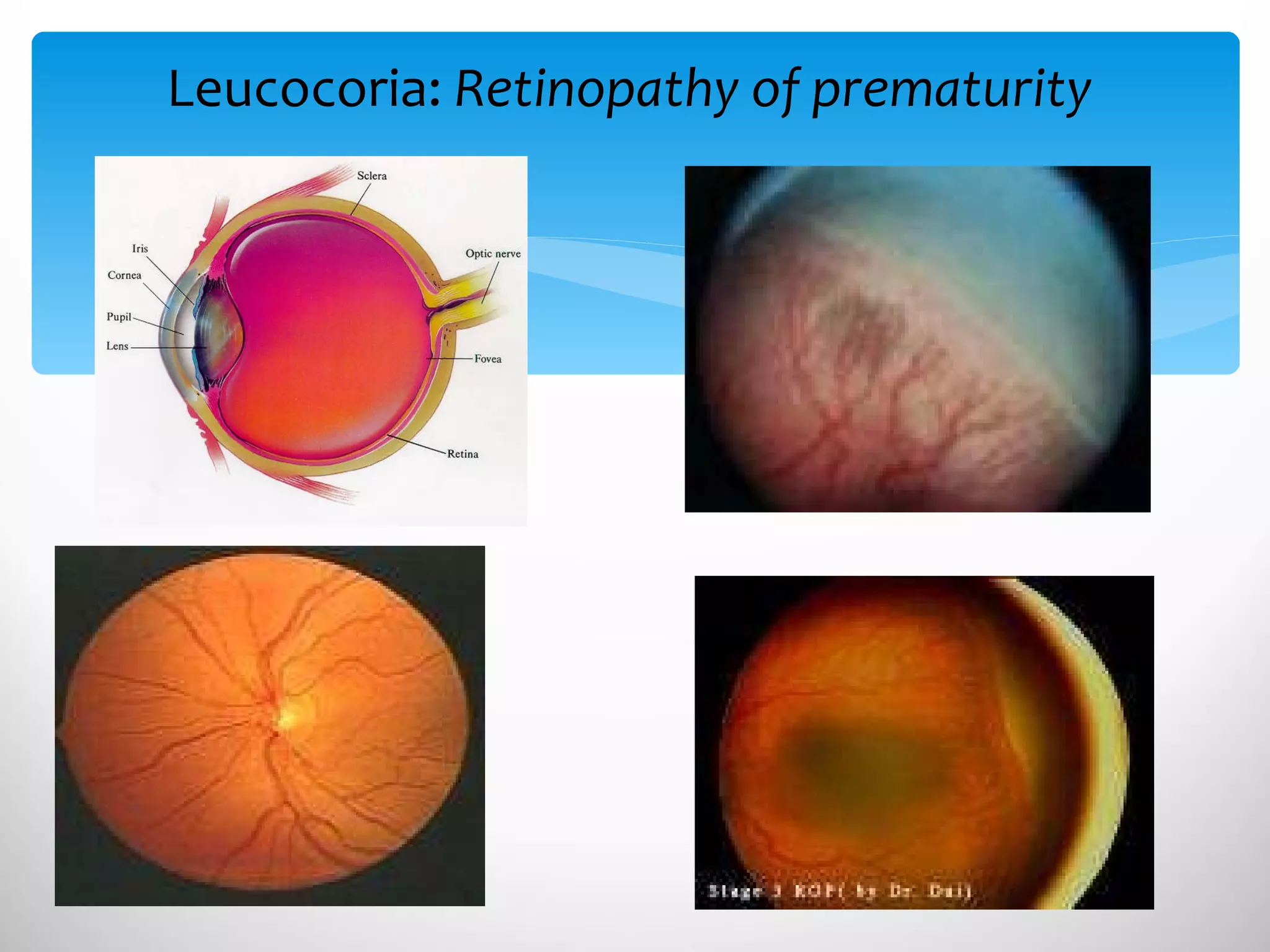
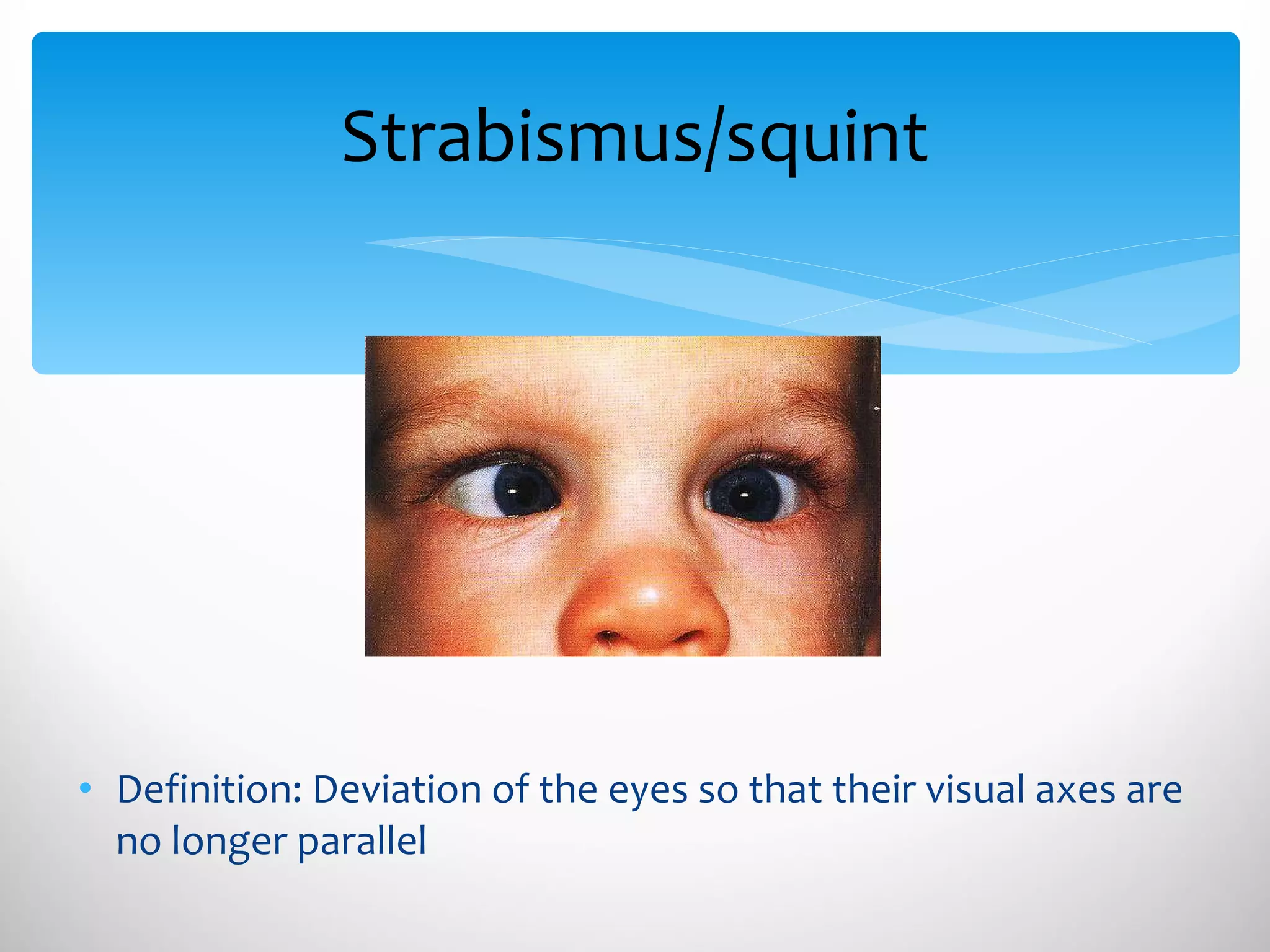
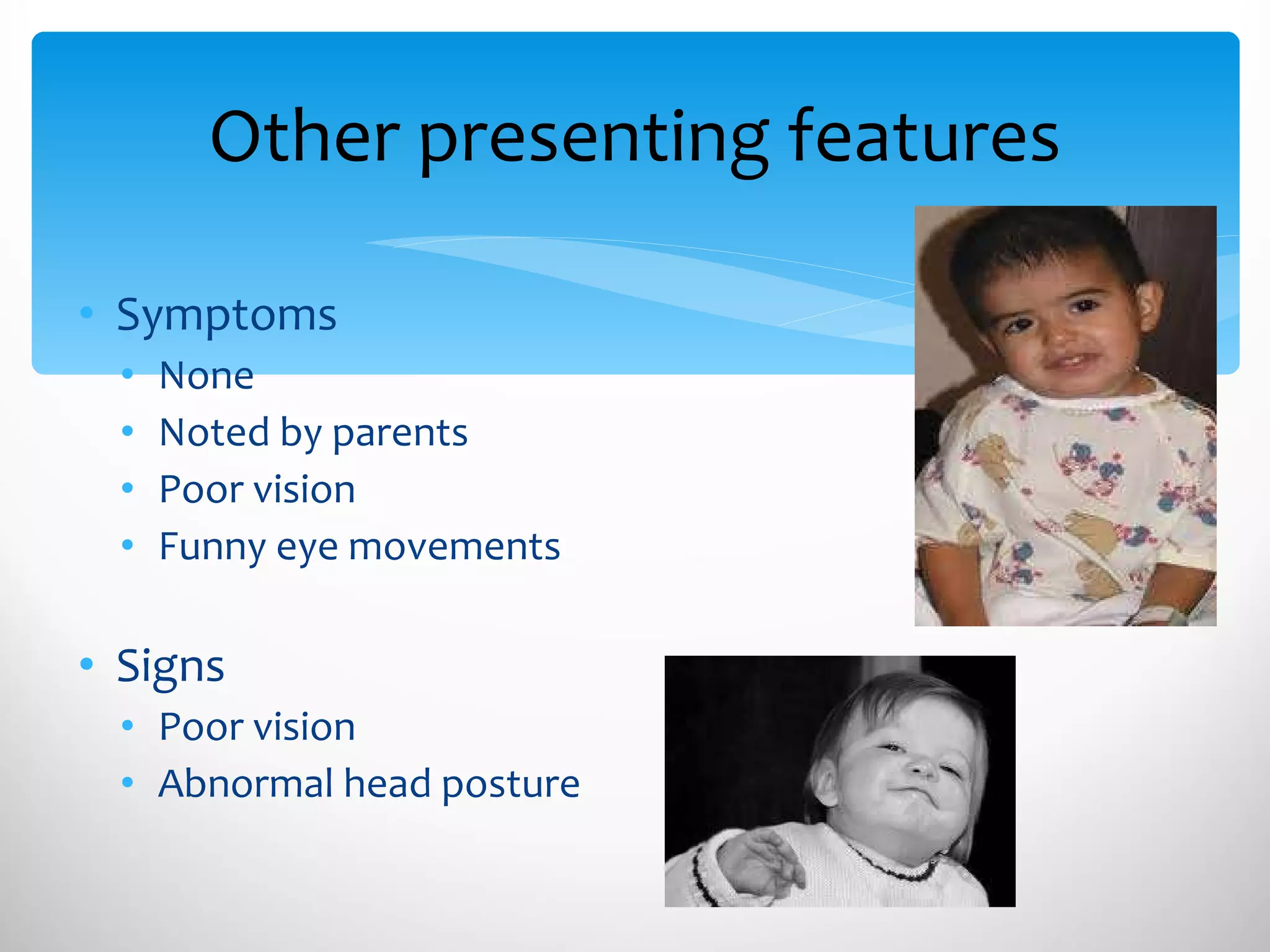
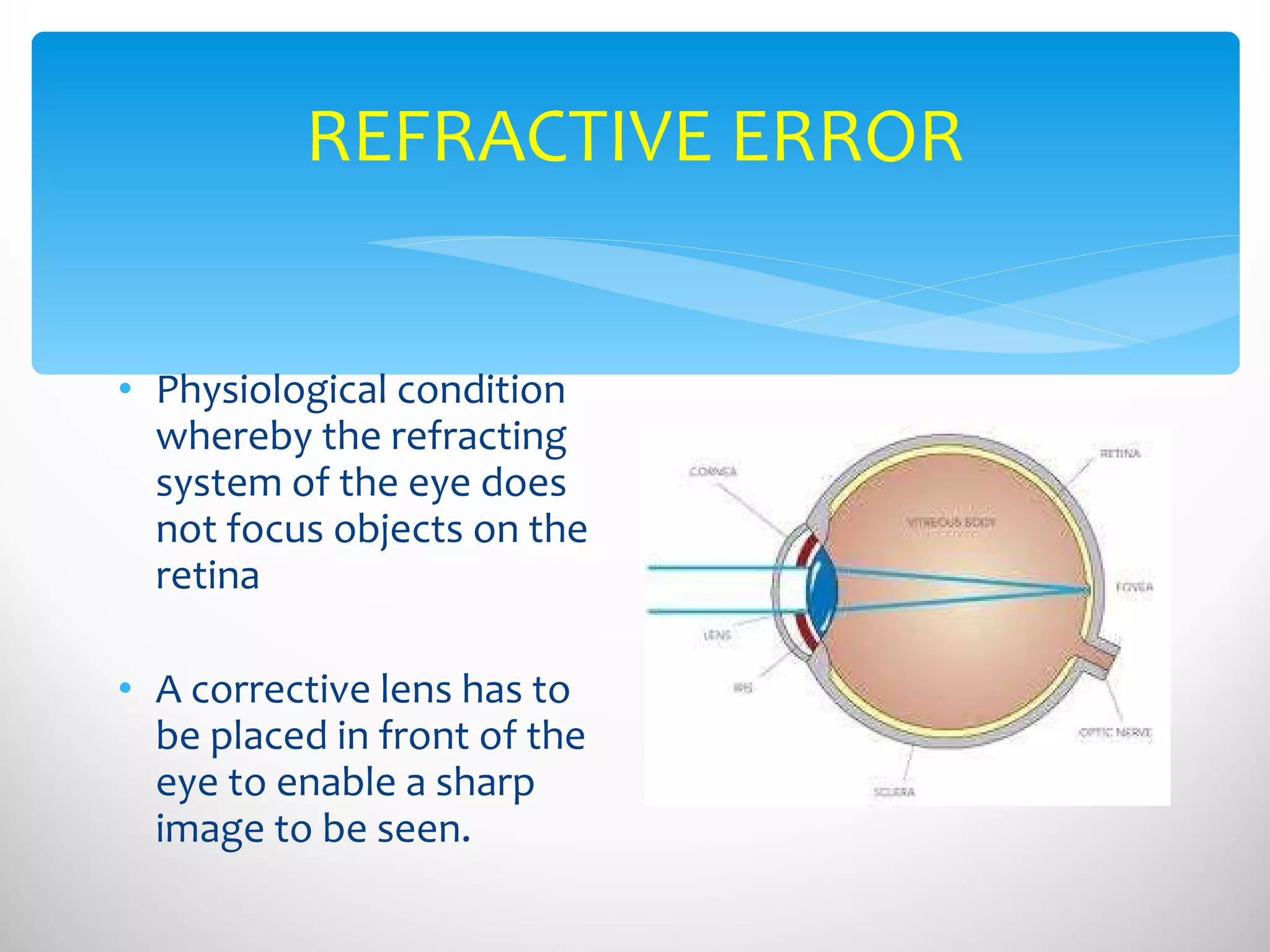
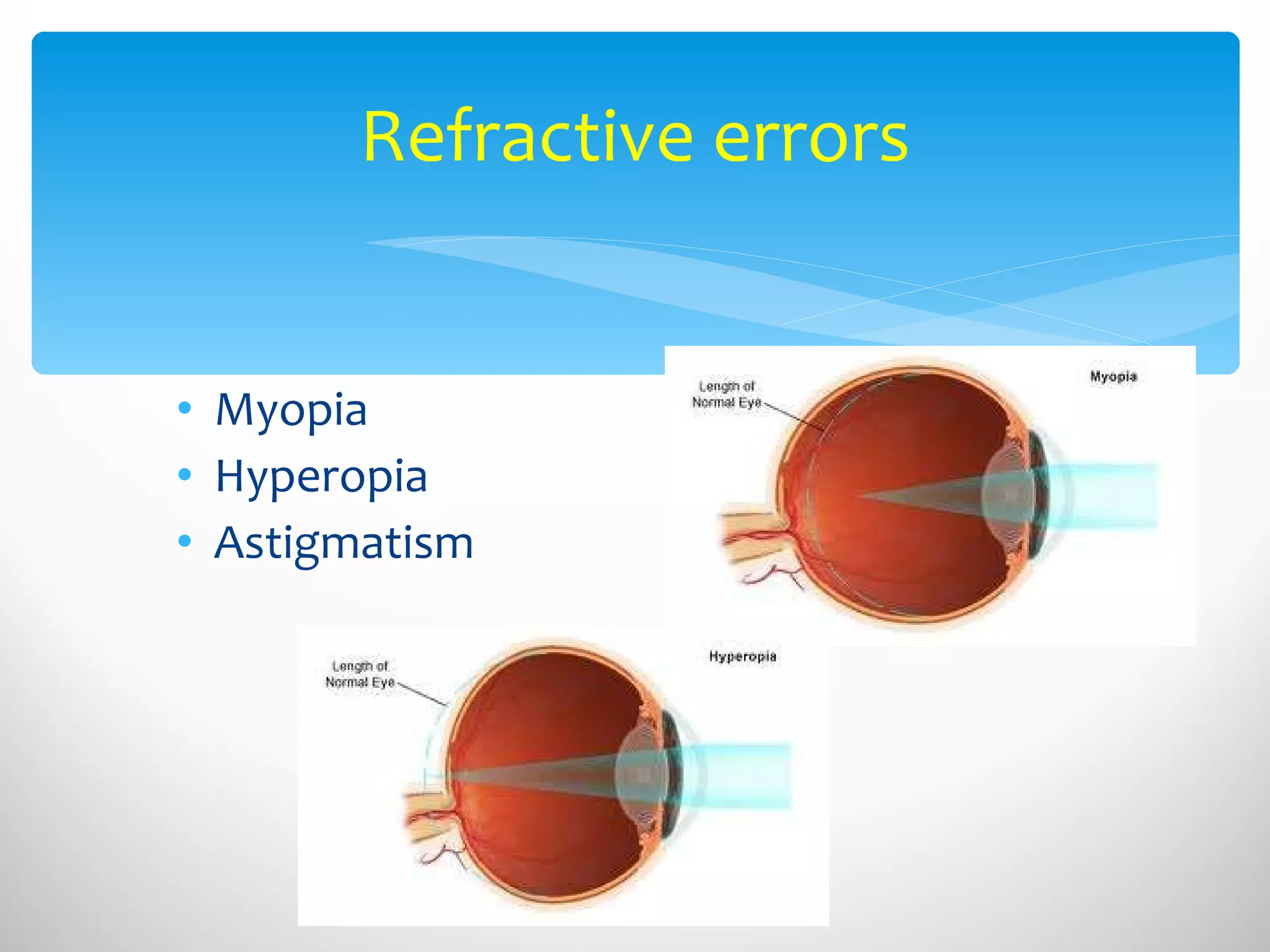
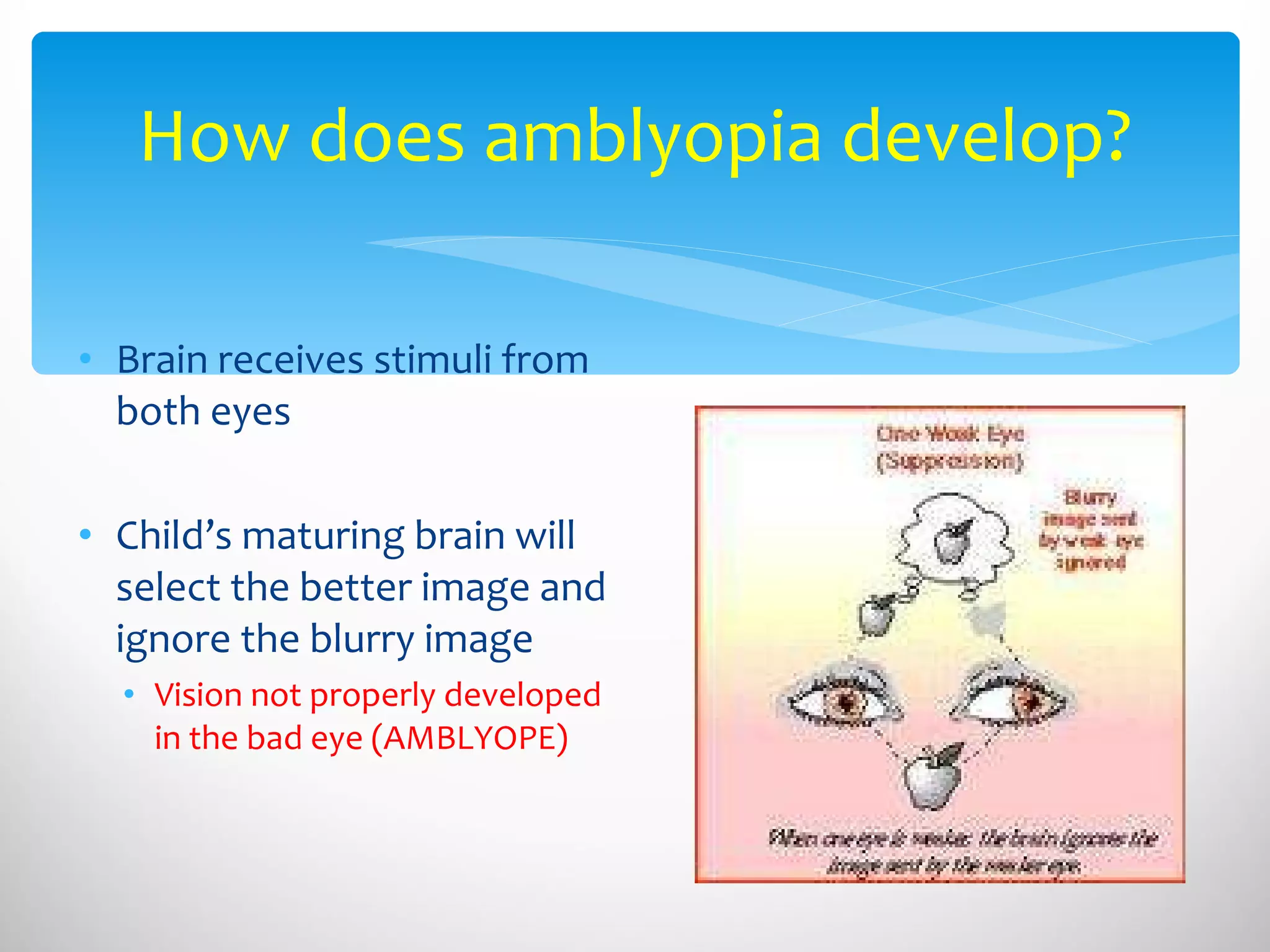
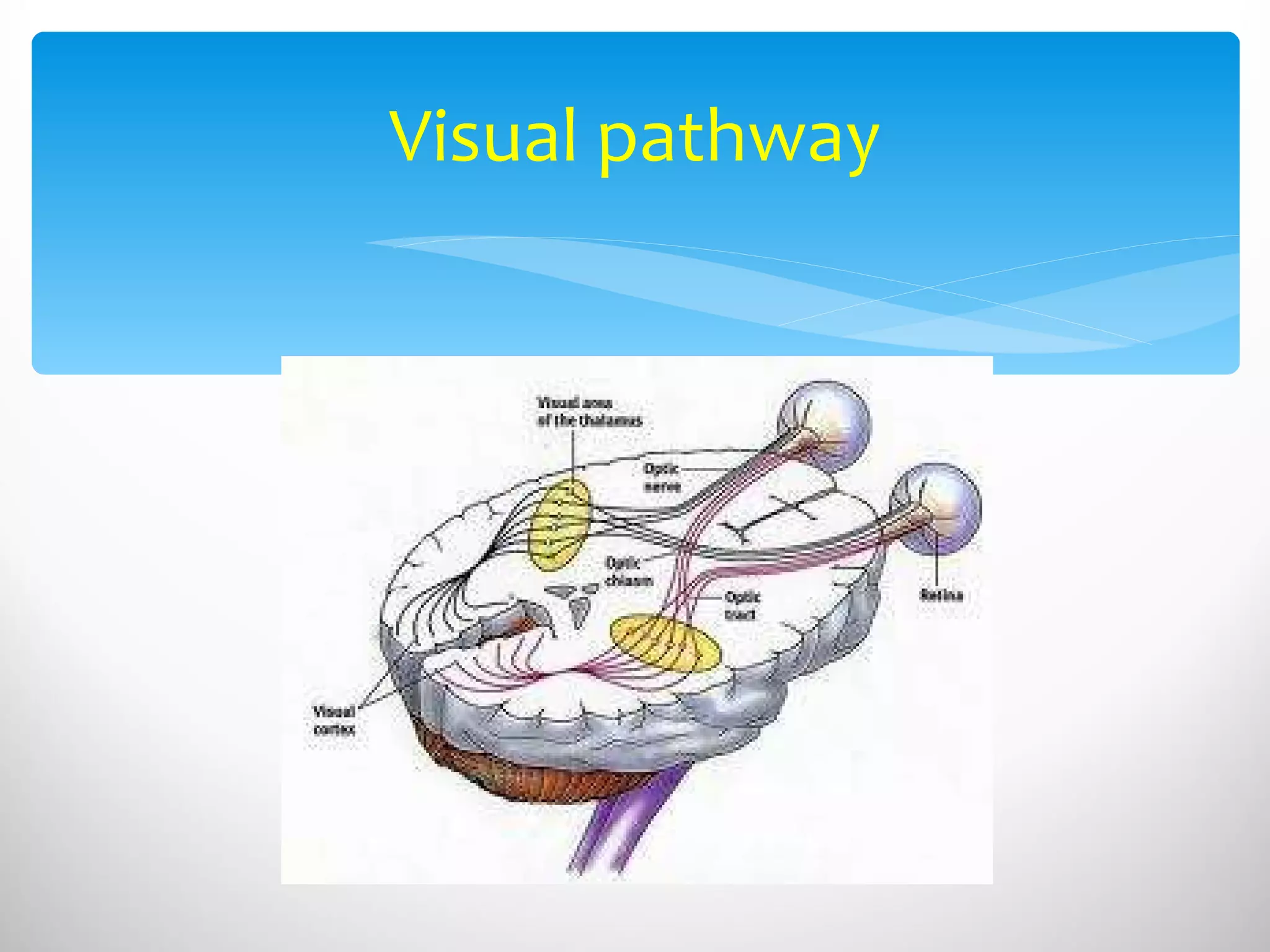
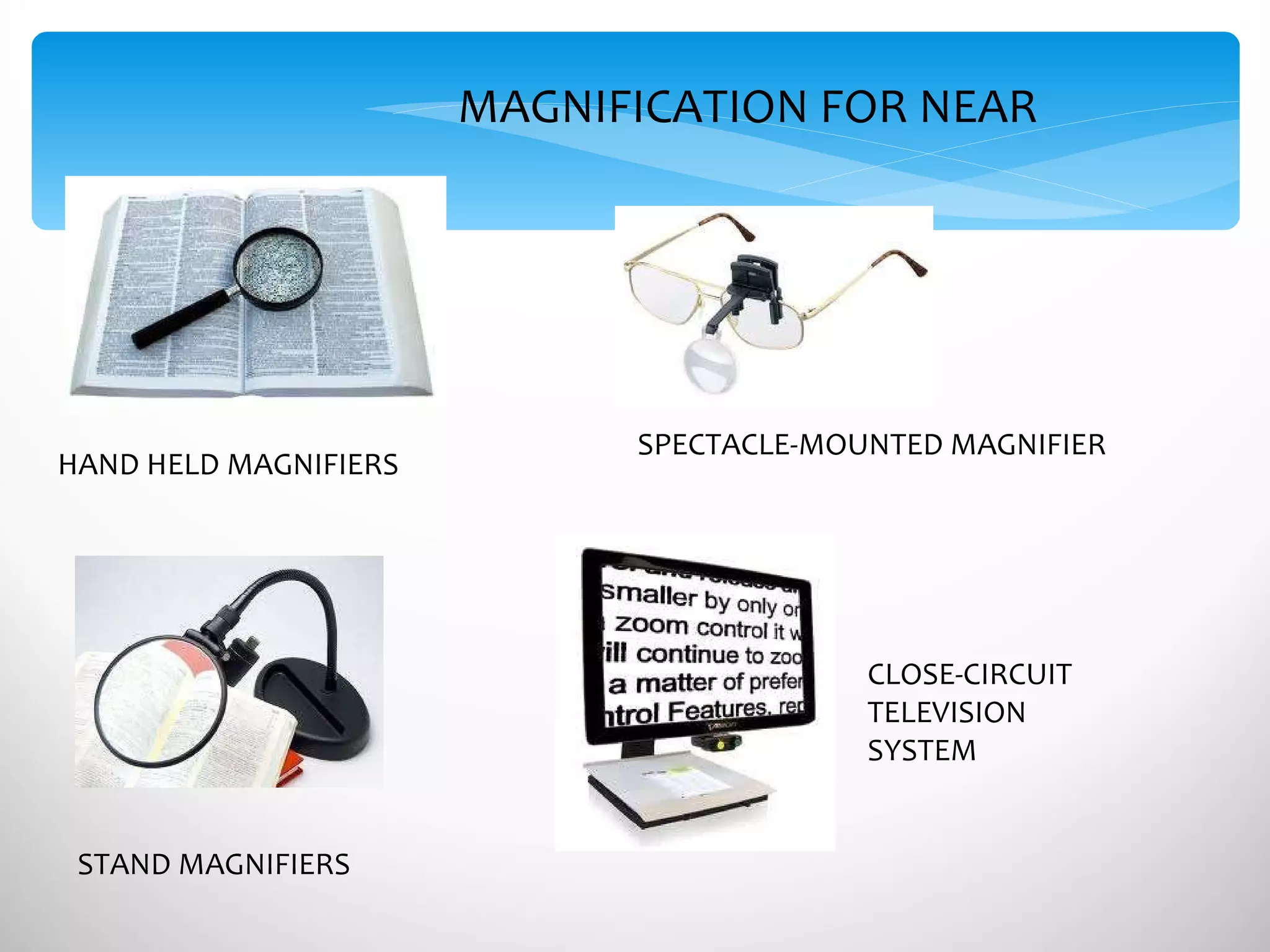
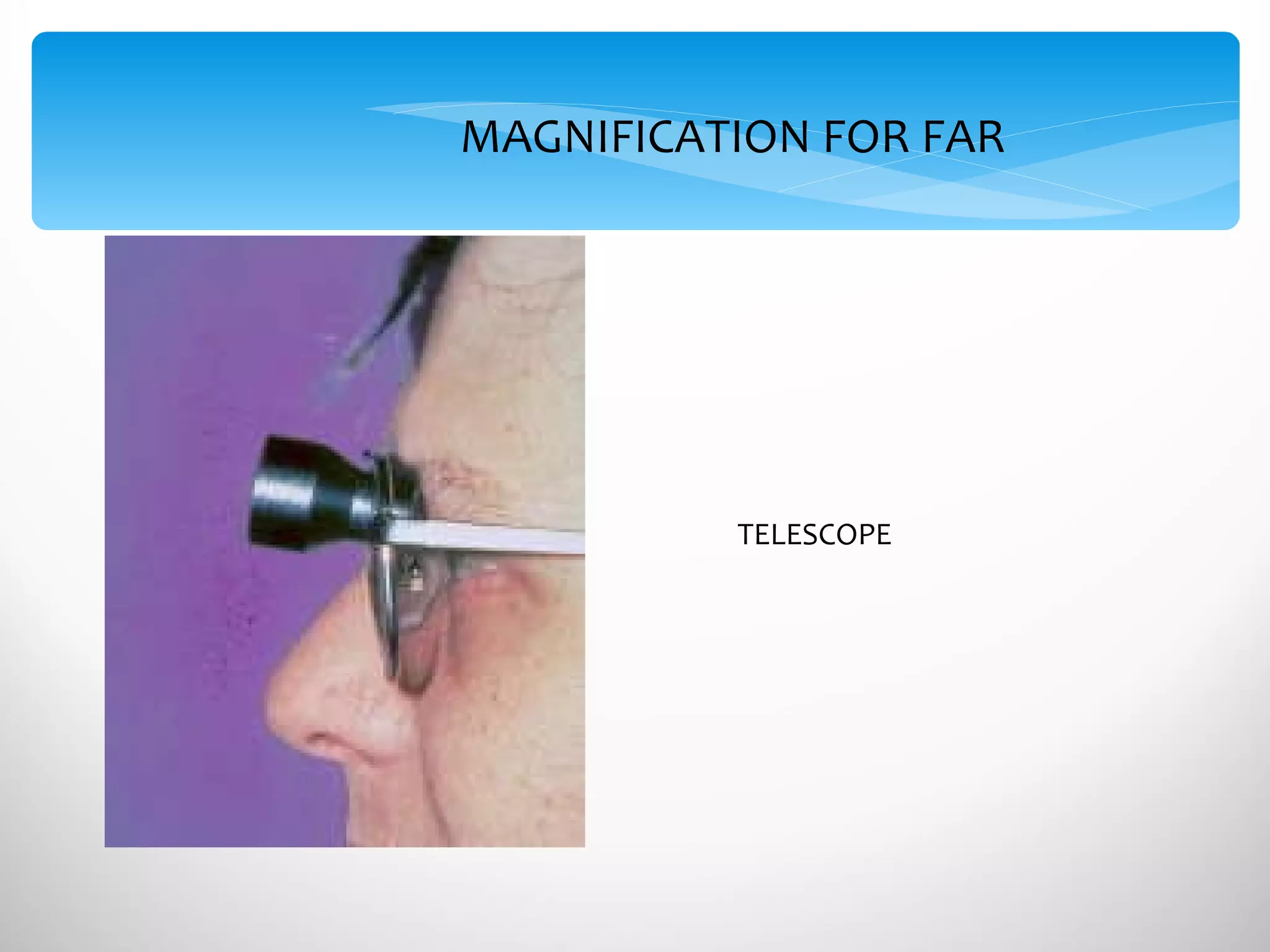
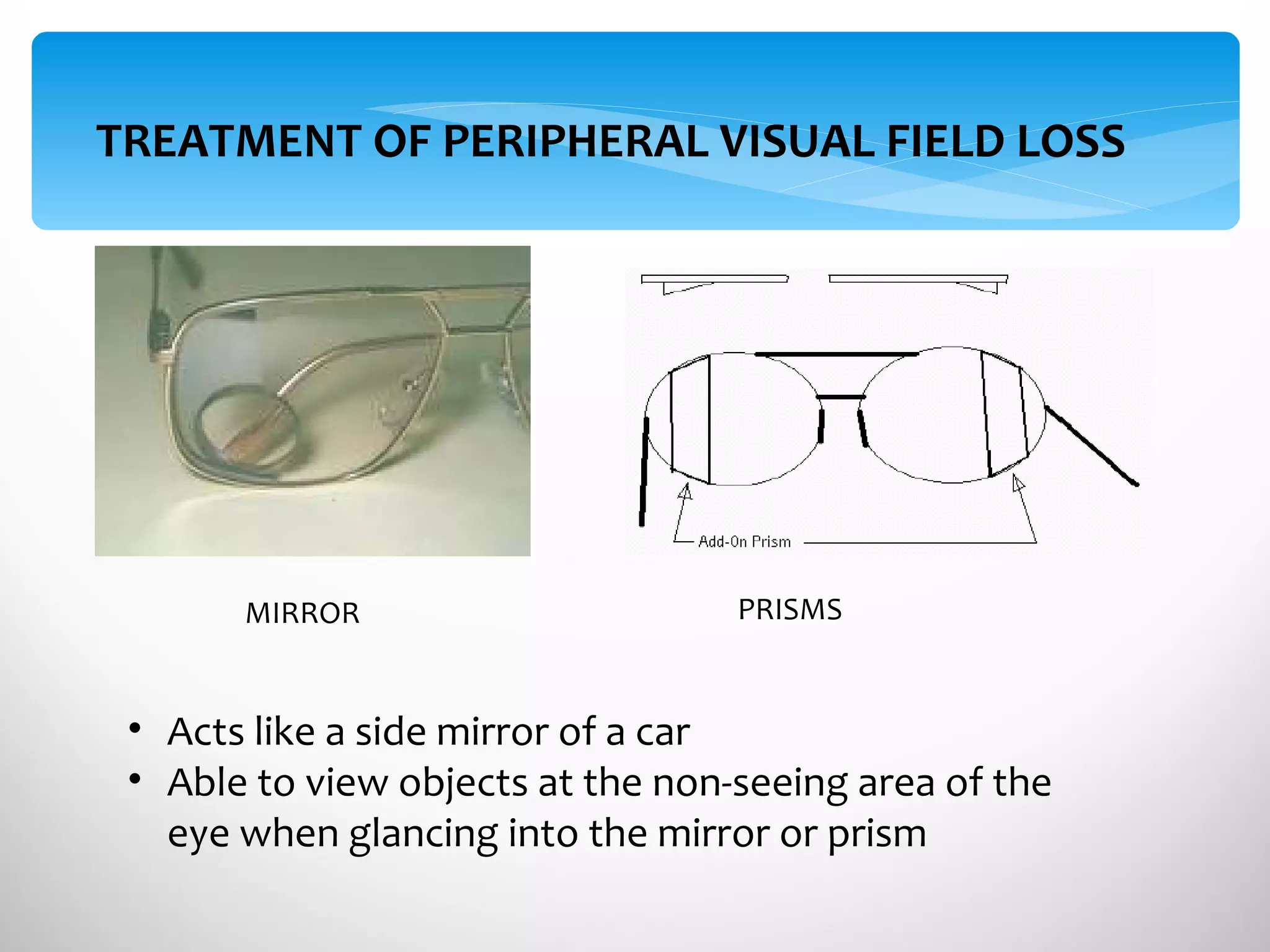
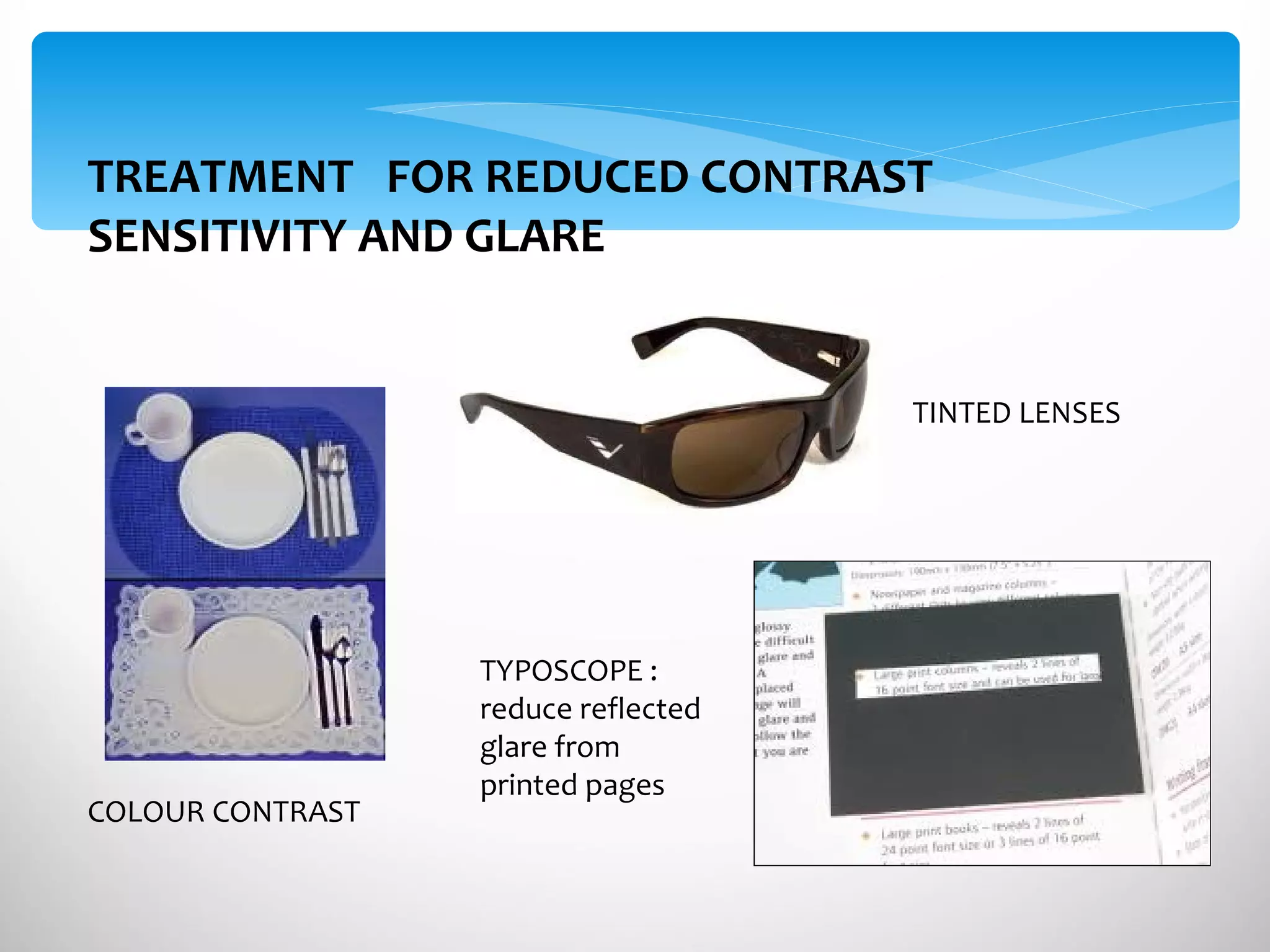
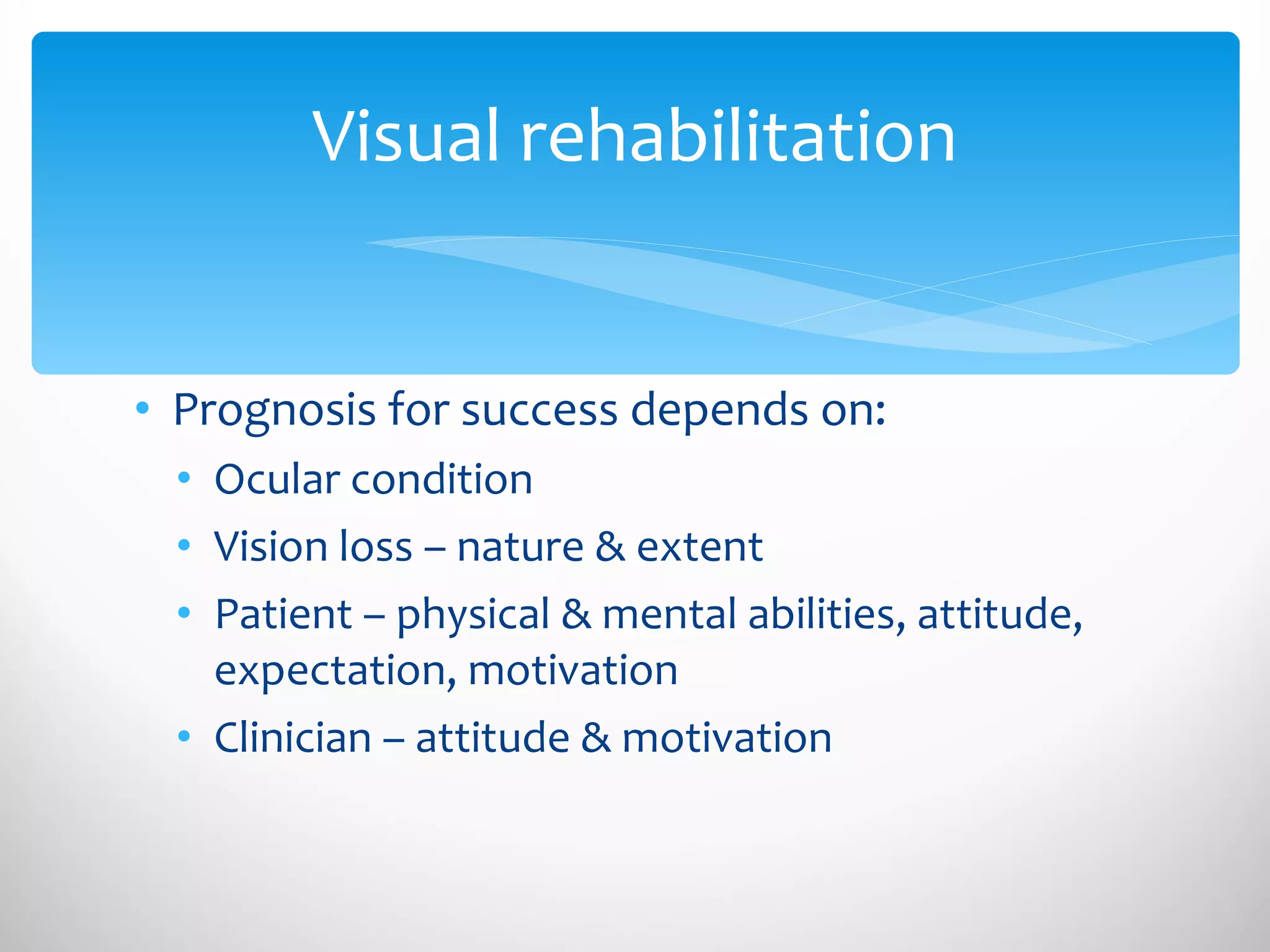
The document discusses visual impairment in children and its evaluation and diagnosis. It defines various types of visual impairment including reduced visual acuity and visual field loss. It describes examining a child's visual acuity, contrast sensitivity, and visual field. Common causes of visual impairment in children mentioned include congenital glaucoma, leucocoria (white eye reflex), cataracts, retinopathy of prematurity, and refractive errors. The evaluation process involves taking a history, performing eye examinations, and conducting investigations to confirm diagnoses. Treatment aims to detect issues early to prevent vision loss and may include optical devices, non-optical methods, and visual rehabilitation.