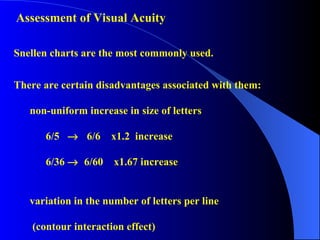
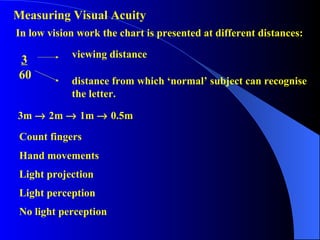
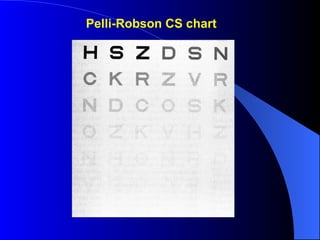
The low vision examination aims to determine a patient's visual abilities and needs through assessment, history taking, and trials of low vision aids. It involves evaluating visual acuity, refractive error, visual fields, and contrast sensitivity. The examiner also considers case history details, functional abilities, independence, and psychological factors to recommend the best low vision solutions and support for each patient.