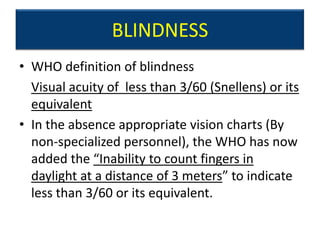
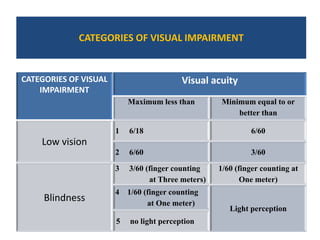
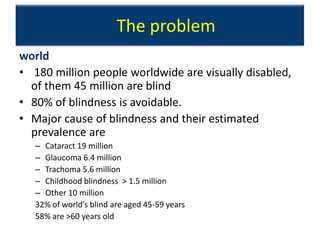
1) Blindness is defined as visual acuity less than 3/60 or inability to count fingers at 3 meters. It affects 180 million people worldwide, of whom 45 million are blind.
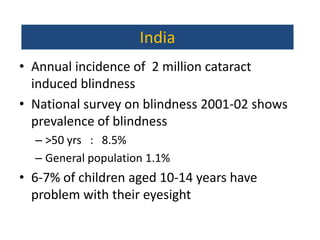
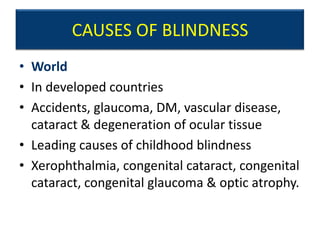
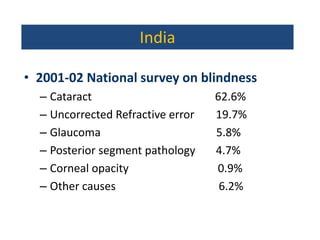
2) Cataract (19 million), glaucoma (6.4 million), and trachoma (5.6 million) are the leading causes of blindness globally. In India, cataract causes 62.6% of blindness.
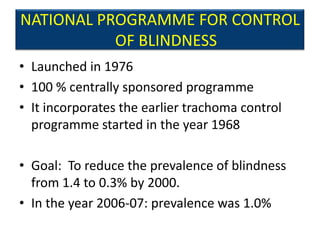
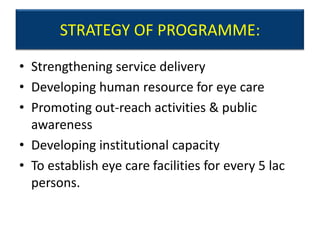
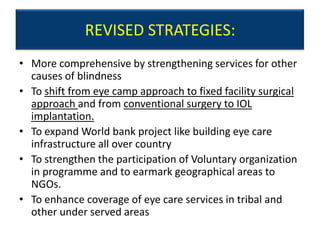
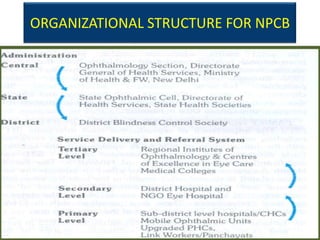
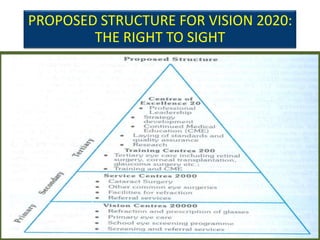
3) Prevention programs focus on primary, secondary, and tertiary eye care as well as specific initiatives for conditions like trachoma and school eye health services. The goal is to reduce blindness prevalence through improved access to eye care.