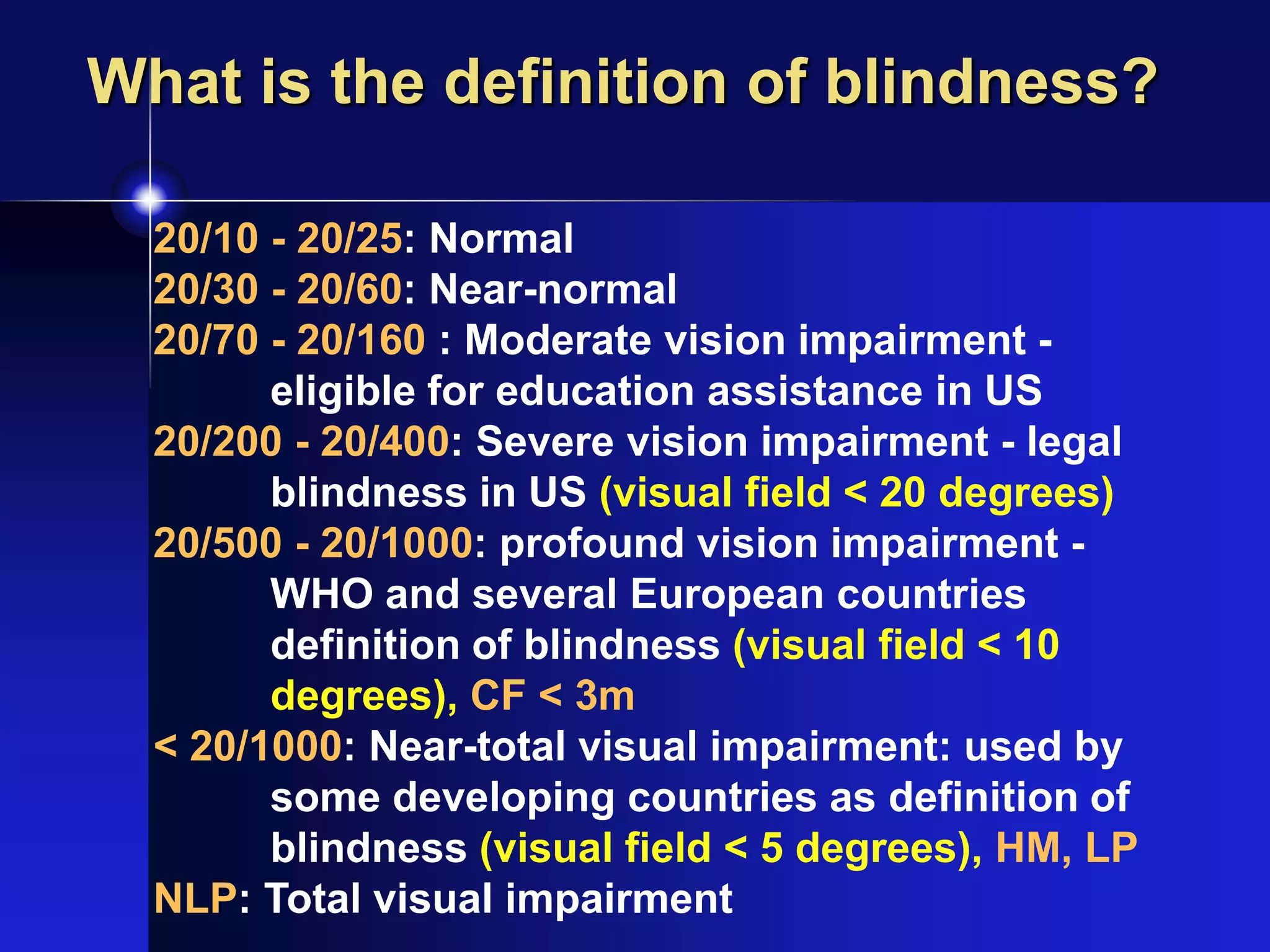
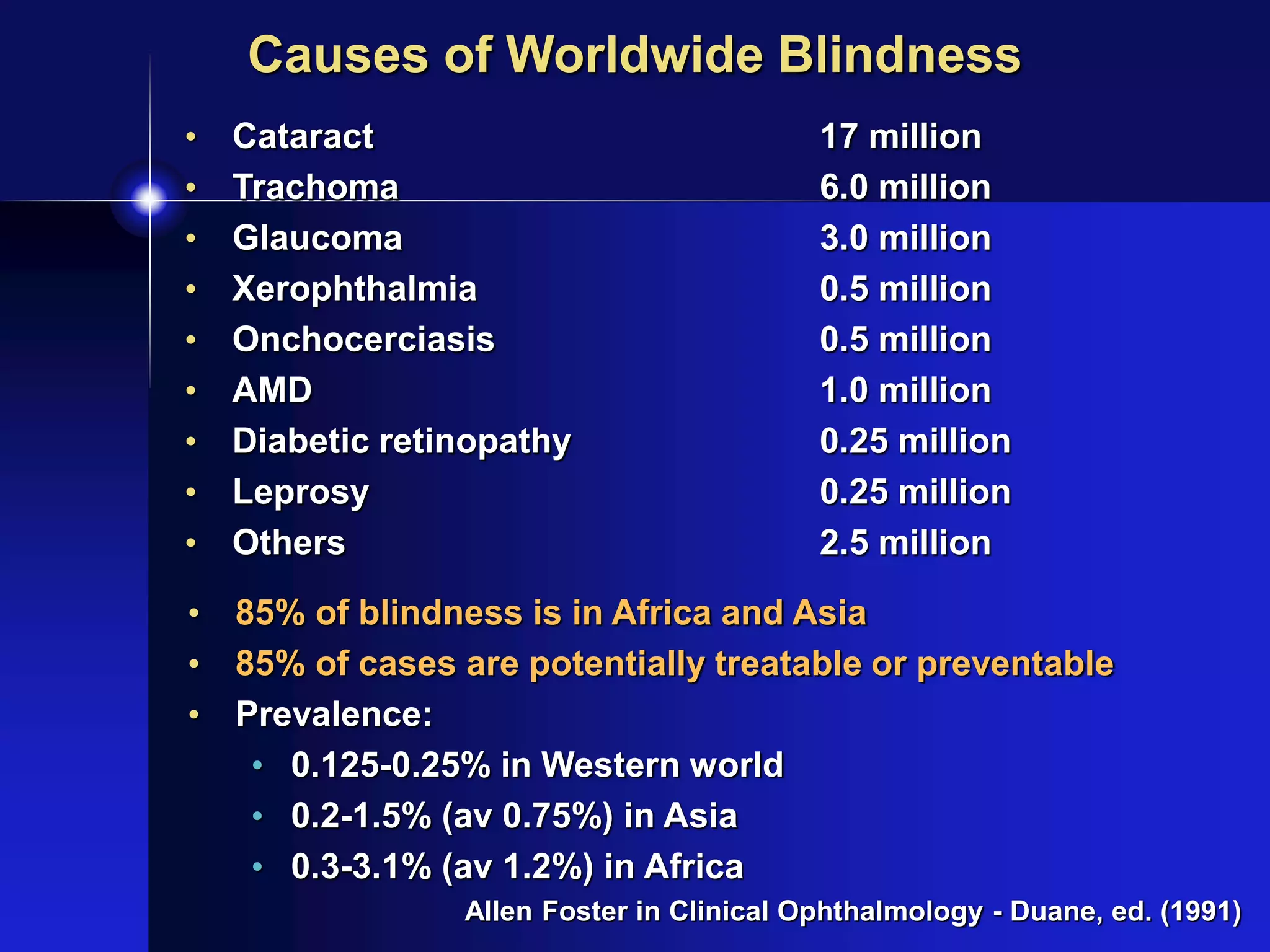
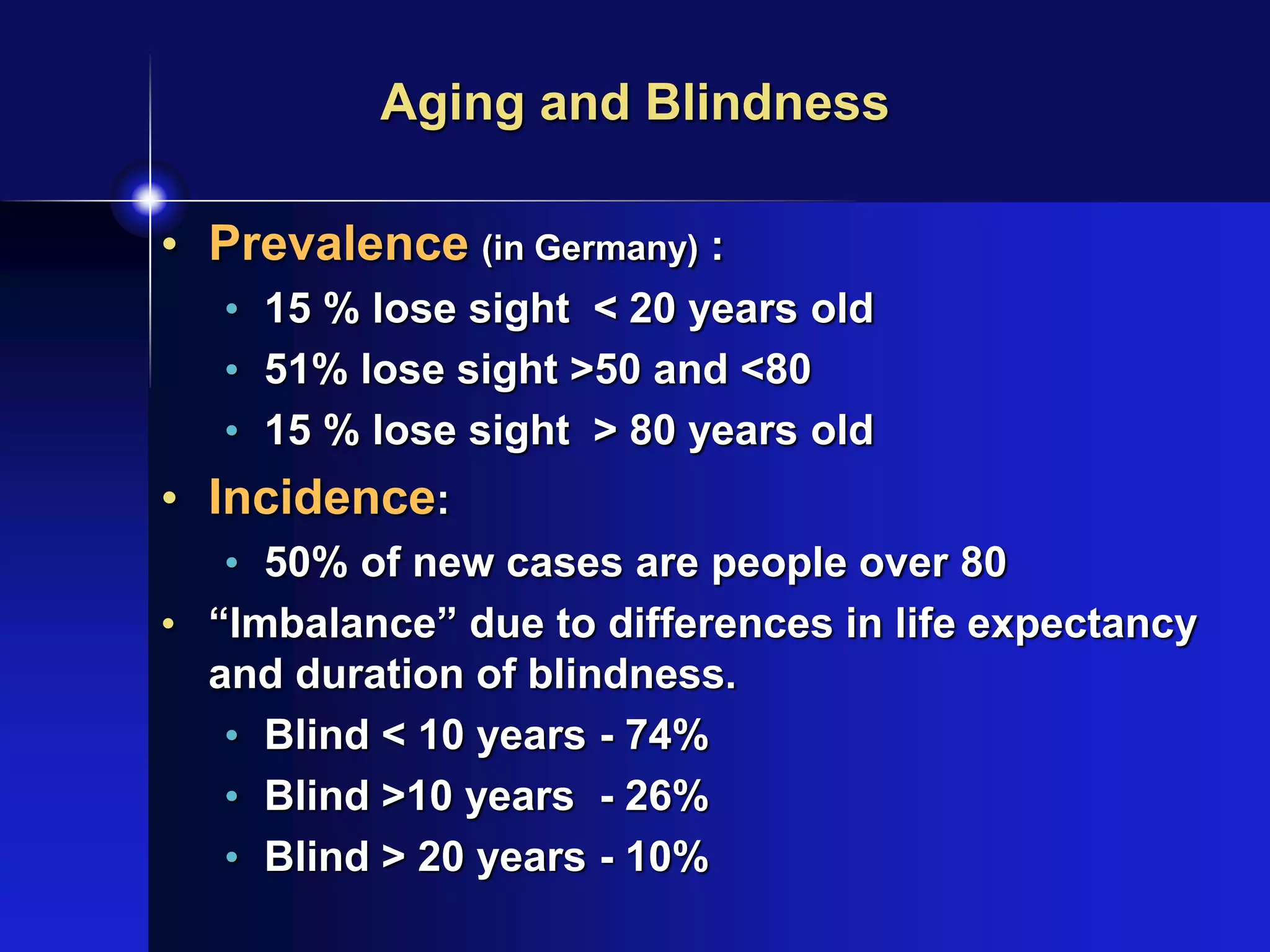
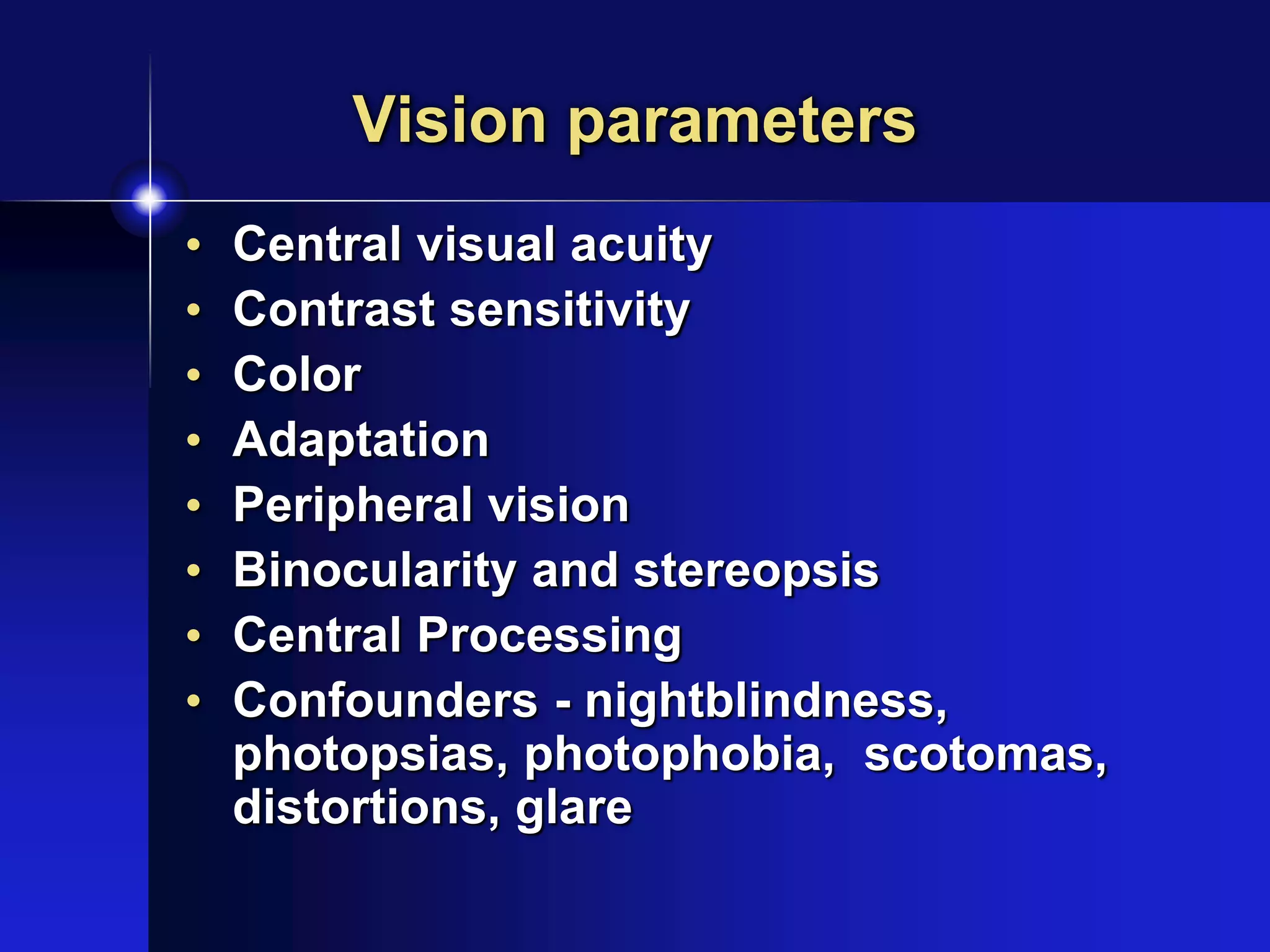
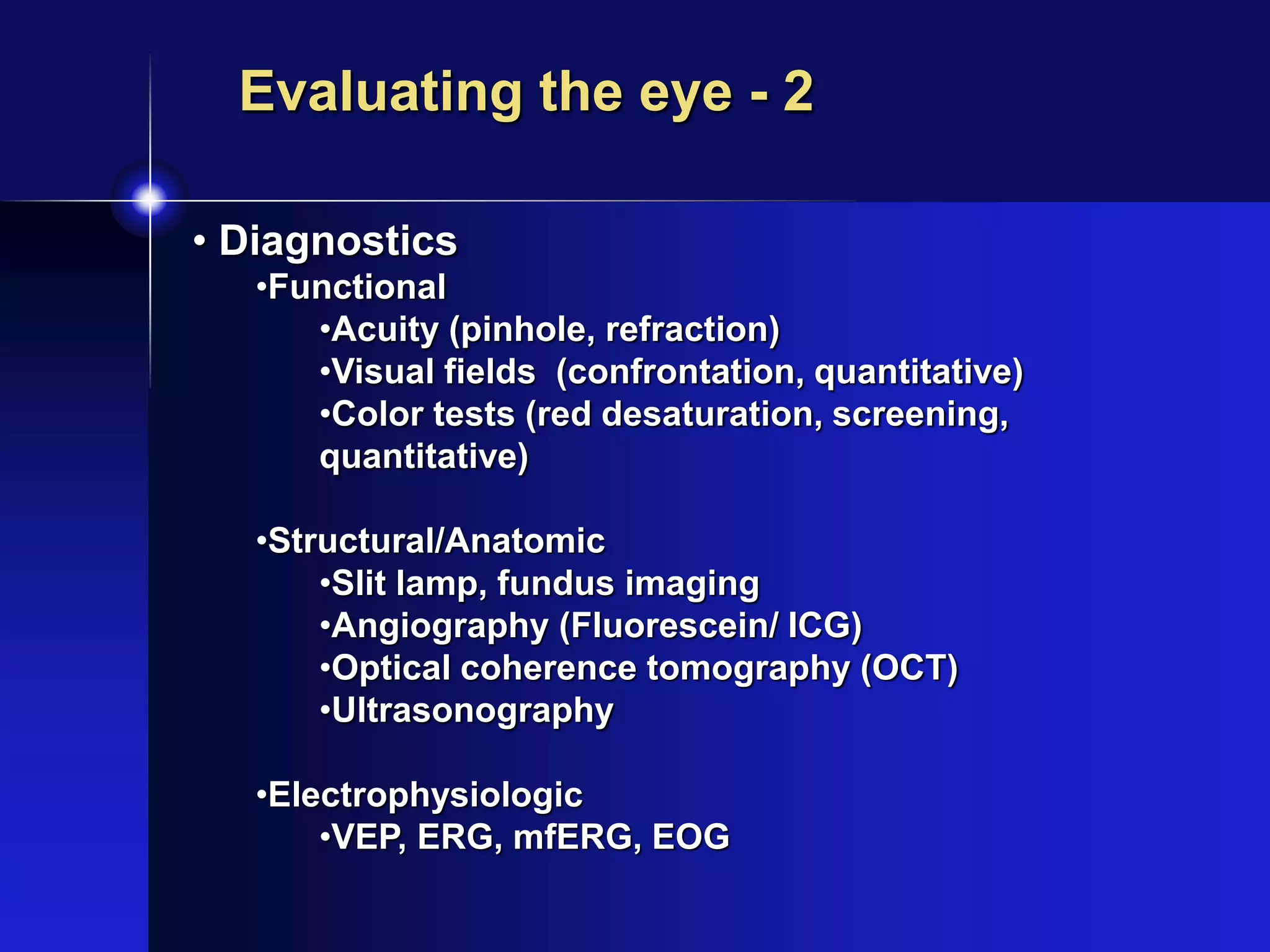
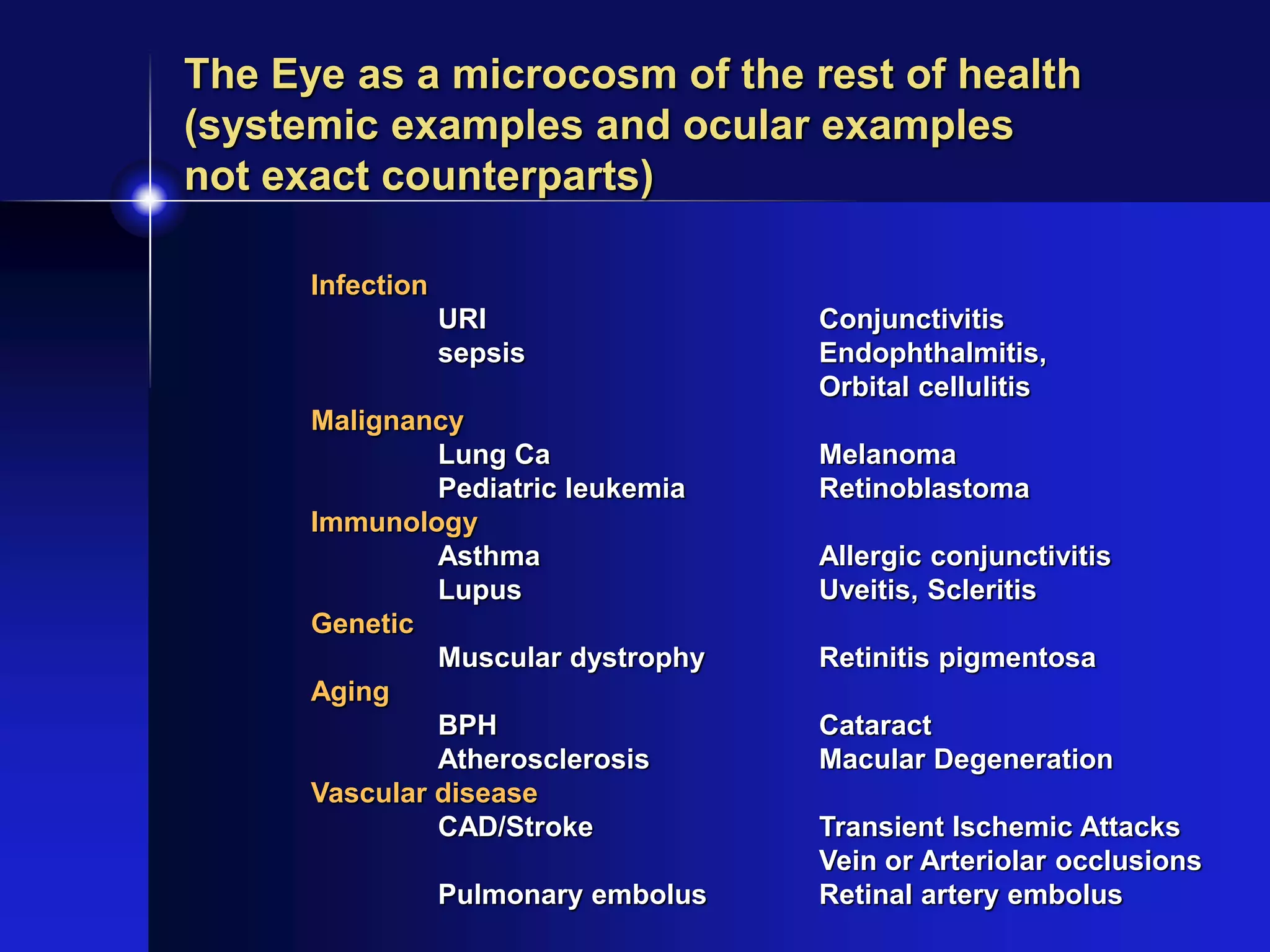
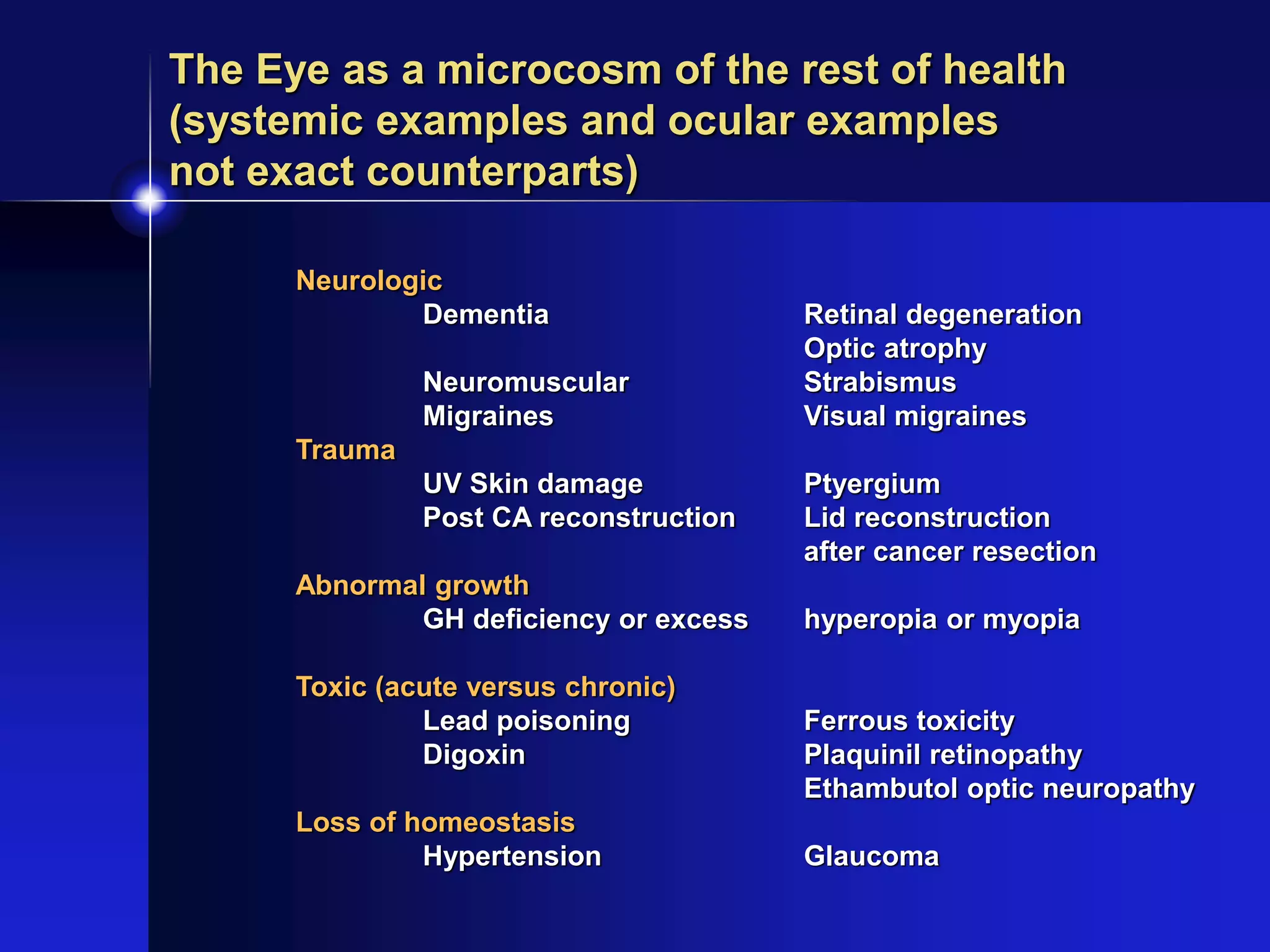
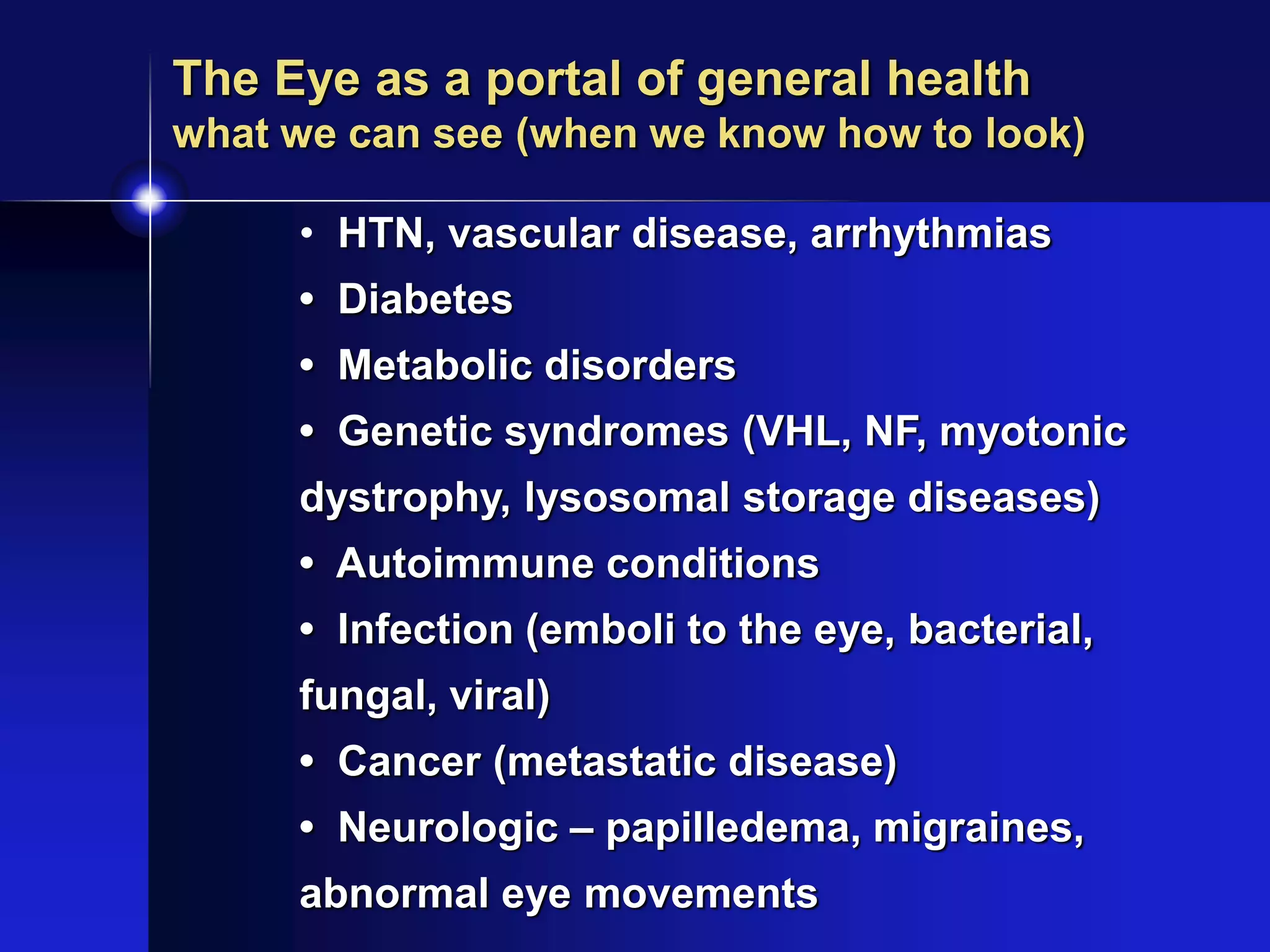
This document provides an overview of a talk on what general physicians should know about vision and the eye. It discusses key topics like defining blindness, common causes of blindness worldwide, aging and blindness, how to evaluate vision parameters, and how the eye can provide insights into general health and systemic diseases. The document outlines goals of understanding basic eye concepts, evaluation, and common eye diseases, but not detailed anatomy or management of conditions. It emphasizes that each patient's vision loss is unique based on their condition and individual factors.