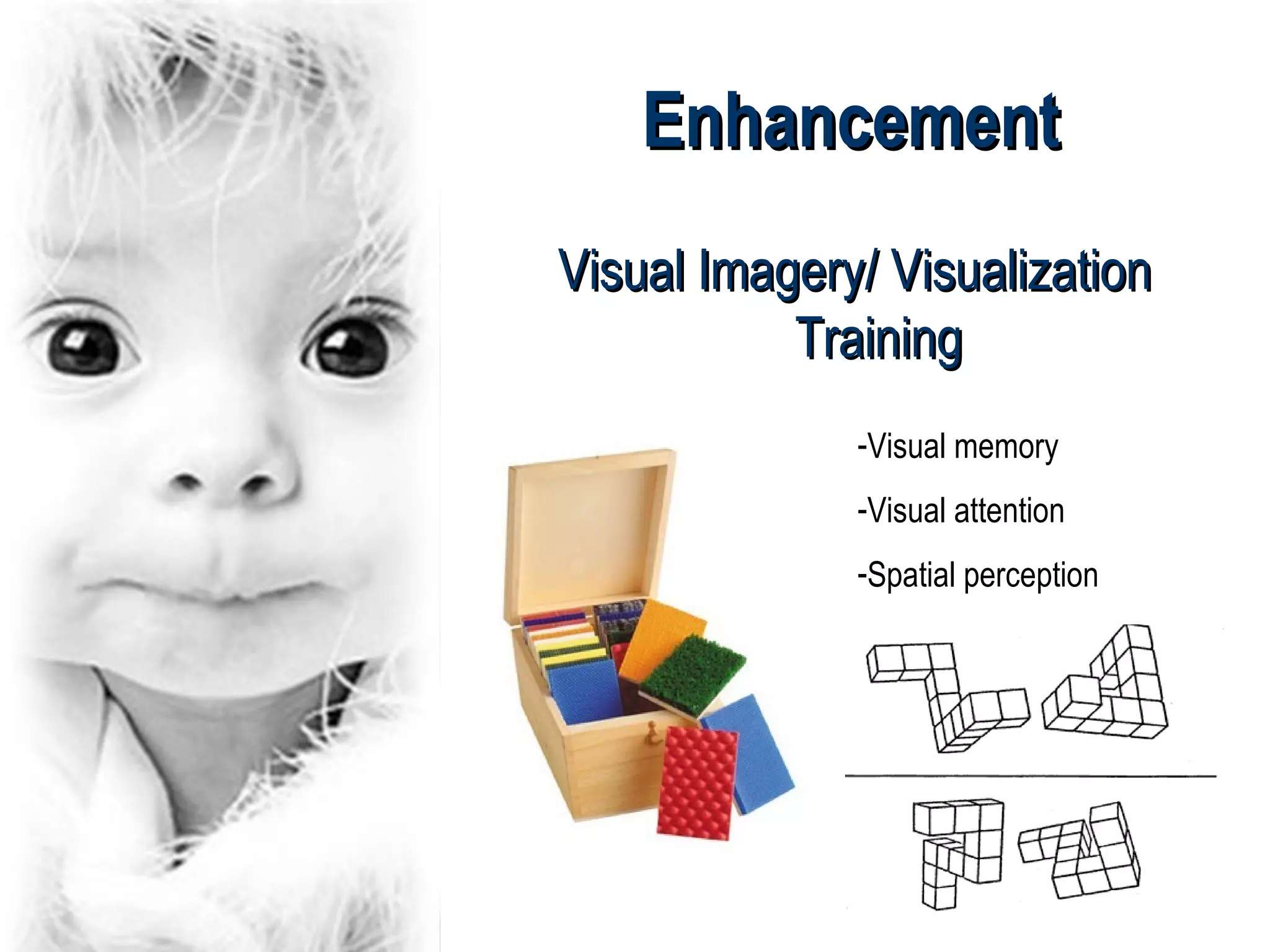
This document discusses low vision in childhood, including various pathologies that can cause low vision such as Leber's amaurosis, optic atrophy, and retinitis pigmentosa. It outlines the visual prognosis and visual field defects associated with each condition. The document also discusses the use of low vision aids in children, noting that children are more accepting of aids and that aids should be introduced early. Various types of aids are described, from magnifiers to closed-circuit television. The document concludes with references.