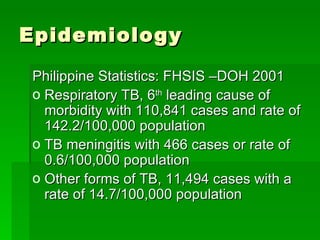
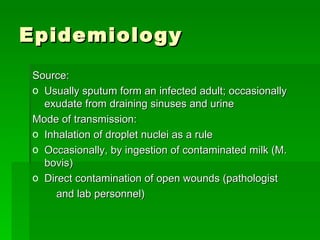
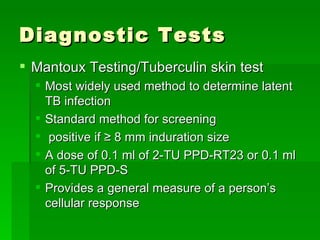
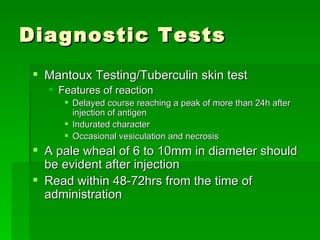
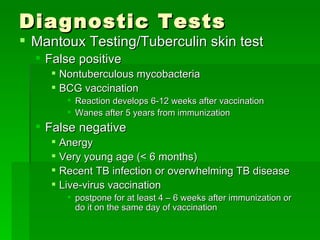
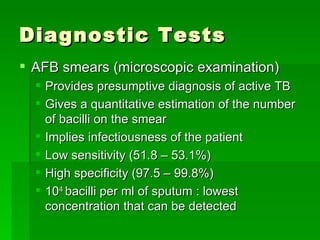
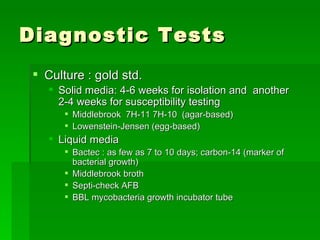
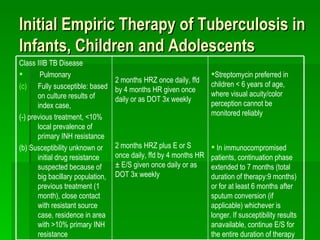
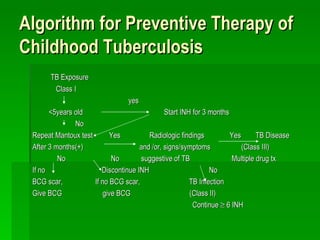
Pulmonary tuberculosis is caused by infection with Mycobacterium tuberculosis or Mycobacterium bovis. It is transmitted through inhalation of droplets from infected individuals. In the Philippines it is one of the leading causes of morbidity. Risk factors include close contact with active cases, immunosuppression, malnutrition, and other diseases like HIV. Diagnosis involves tuberculin skin testing, sputum smear and culture, chest x-rays, and biopsy when needed. Treatment consists of a combination of antibiotics over several months.