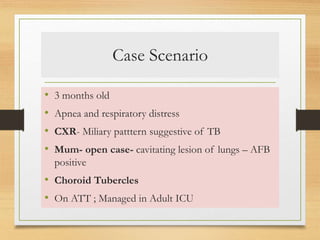
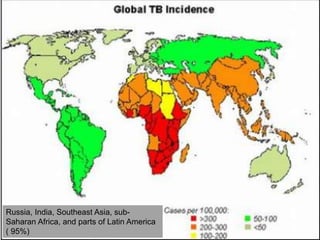
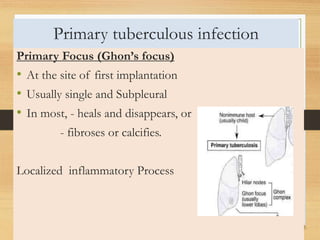
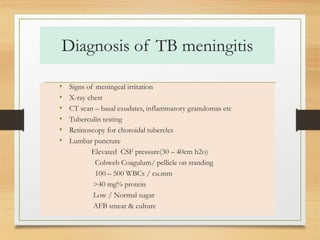
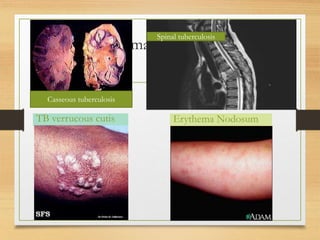
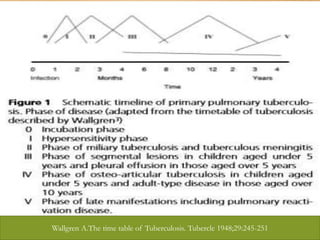
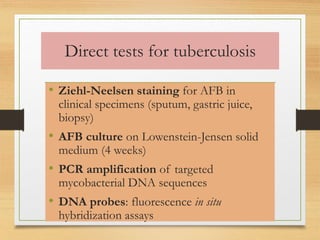
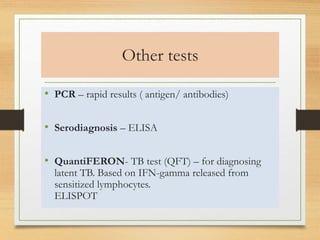
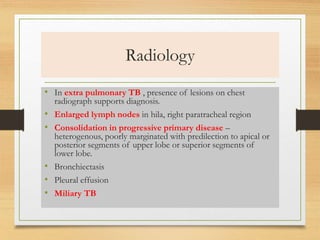
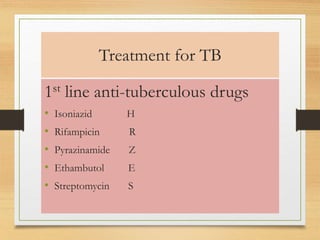
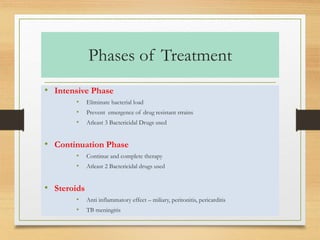
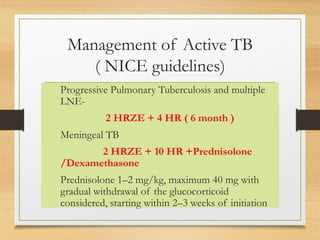
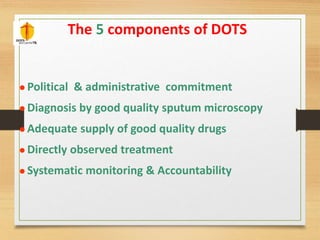
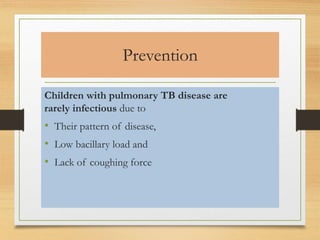
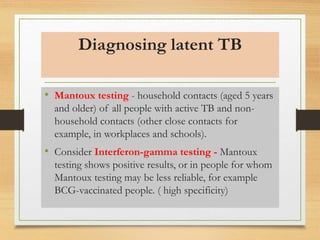
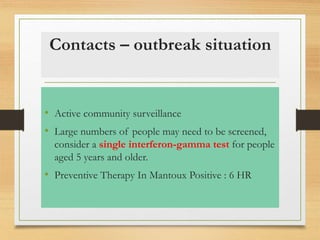
The document covers childhood tuberculosis, discussing its pathophysiology, epidemiology, clinical manifestations, and treatment strategies. It highlights the importance of diagnosis and management, including the use of first-line anti-tuberculous drugs and preventive measures. Additionally, it addresses the challenges of multidrug-resistant tuberculosis and the need for ongoing surveillance and education.