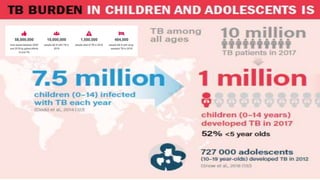
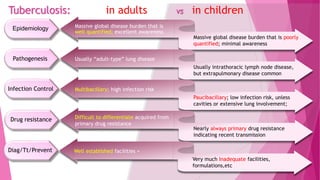
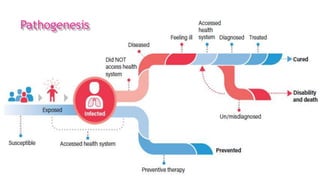
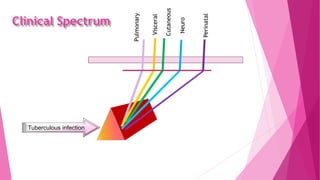
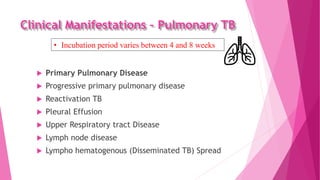
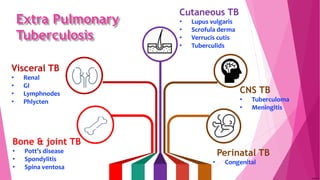
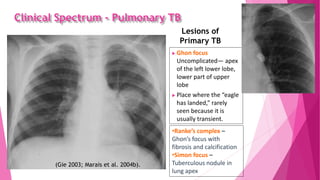
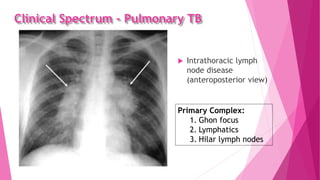
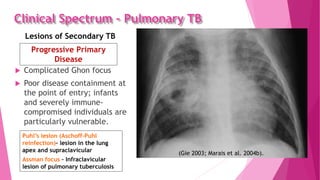
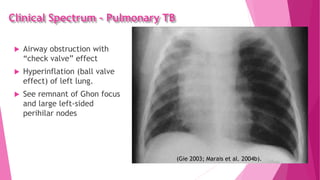
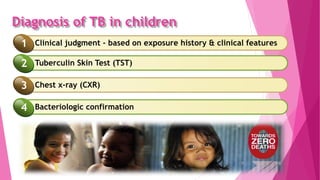
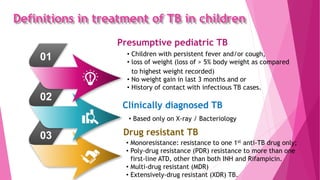
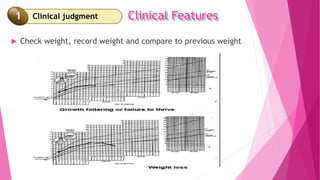
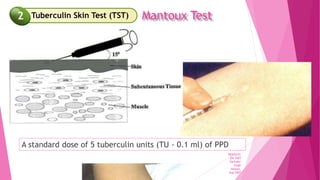
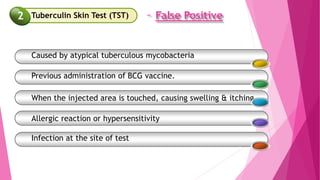
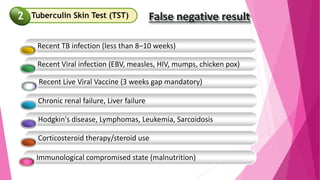
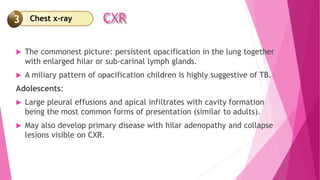
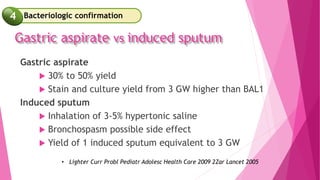
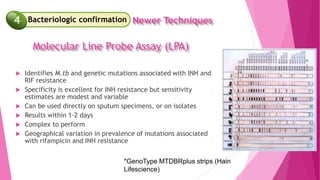
This document discusses tuberculosis (TB) in children. It begins with an overview of the clinical spectrum of TB in children, which can include pulmonary, visceral, cutaneous, neuro, and perinatal manifestations. Pulmonary TB lesions in children typically include primary complexes and intrathoracic lymphadenopathy. Extrapulmonary TB involves sites like bone, joints, the gastrointestinal tract, and the central nervous system. The document then covers the diagnosis of TB in children, which involves clinical judgment based on exposure history and symptoms, the tuberculin skin test, chest x-ray, and bacteriological confirmation via sputum sampling or gastric aspiration. Interpretation of diagnostic tests and their limitations are also discussed.




![ Rapid detection of M.tb and Rif resistance
Sensitivity: 95-99.5%; specificity: 95%
For sputum smear (+)/(-)
Minimal training
Minimal space requirements
Fully automated
Results in 2 hours
Cartridge Based Nucleic Acid Amplification Test
4 Newer Techniques
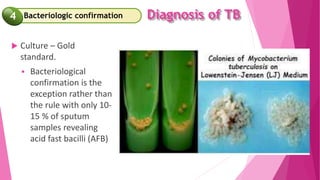
Bacteriologic confirmation
4
Gene Xpert Mtb/Rif [CBNAAT]](https://image.slidesharecdn.com/tbinpediatrics-210909074447/85/TB-in-pediatrics-46-320.jpg)