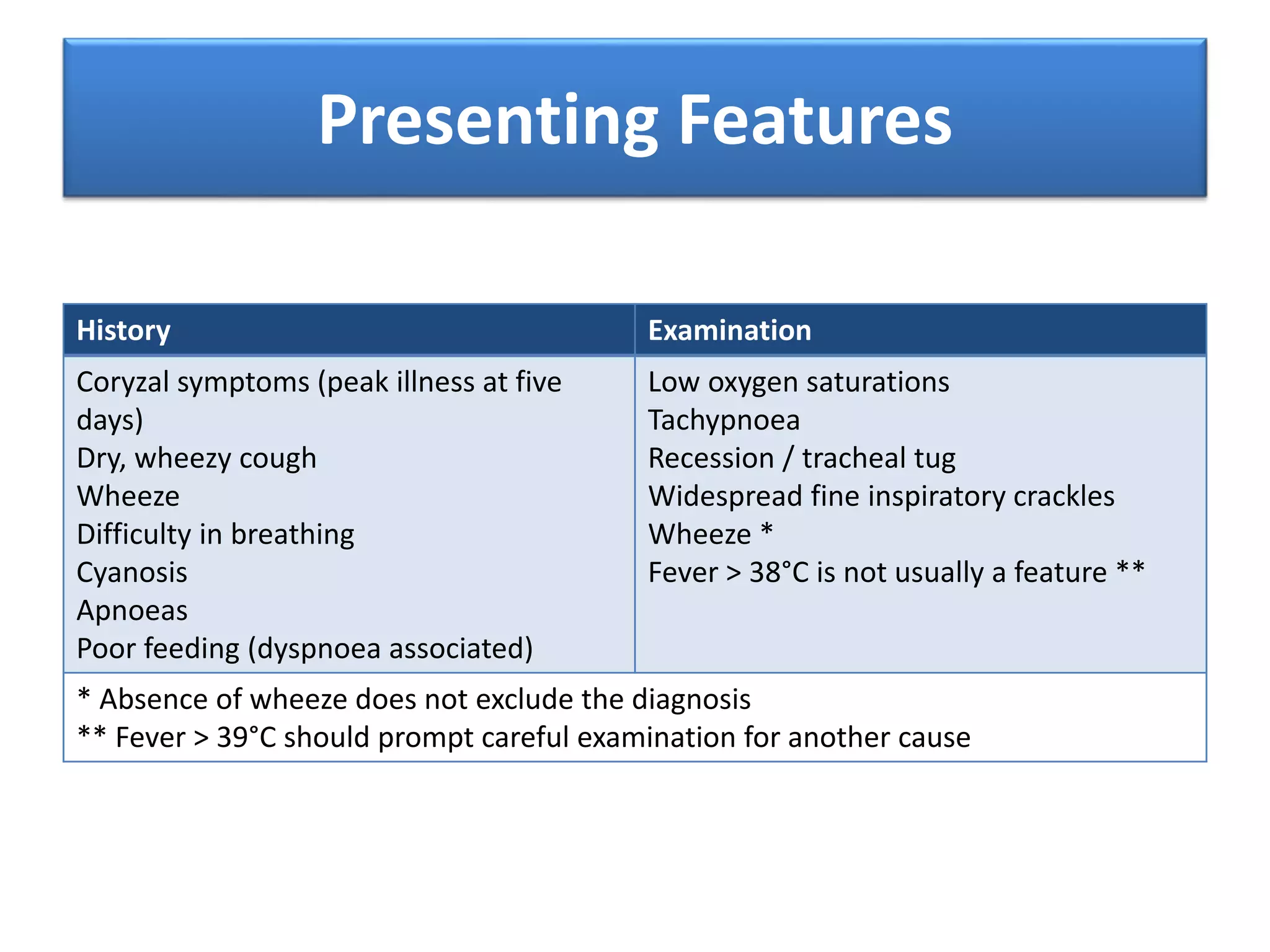
Bronchiolitis is a common viral infection that affects infants under 2 years old, usually caused by RSV. It involves inflammation in the small airways of the lungs. Symptoms include cough, wheezing, difficulty breathing, and low oxygen levels. Infants may require admission if their oxygen levels drop below 94%, respiratory rate is over 70, or they have trouble feeding. Treatment focuses on supportive care like oxygen, feeding support, and nebulized saline. Most infants recover in 4-5 days but cough can last 2-4 weeks.