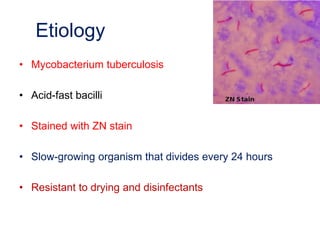
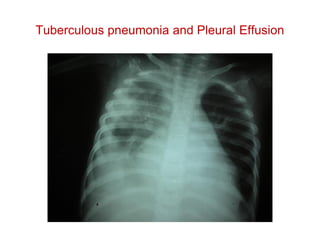
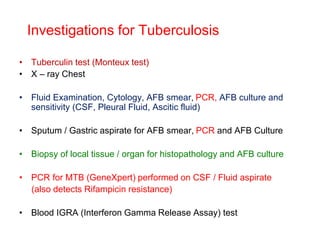
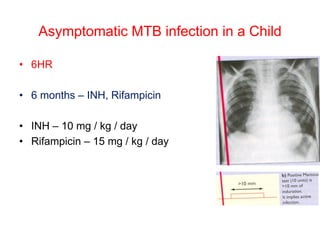
The document discusses tuberculosis in children, including its epidemiology, etiology, clinical features, diagnosis, and management. It notes that tuberculosis is endemic in Pakistan, with over 200,000 new cases annually. Children under 15 account for 20% of cases. The causative agent is Mycobacterium tuberculosis. Clinical features vary depending on the site of infection, and may include cough, fever, lymph node enlargement, and meningitis. Diagnosis involves tuberculin tests, chest X-rays, and culture of fluid/tissue samples. Standard drug regimens include isoniazid and rifampin for 6-12 months. Prevention involves BCG vaccination, contact screening, and prophylactic treatment of