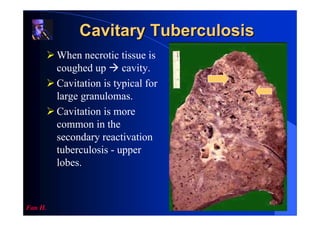
Tuberculosis (TB) remains a major global health problem, infecting one third of the world's population. It is caused by the bacterium Mycobacterium tuberculosis which primarily affects the lungs. TB is transmitted via airborne droplets when people with active pulmonary TB cough, sneeze or spit. Common symptoms include cough, chest pain, and weight loss. Diagnosis involves microscopic examination of sputum samples and culture testing. Treatment requires a combination of antibiotics over a period of 6-9 months. Improving living conditions and developing more effective vaccines are important for tuberculosis control and elimination.