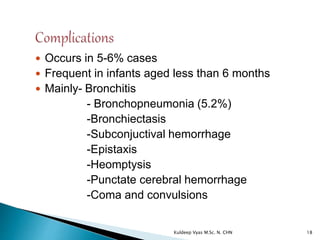
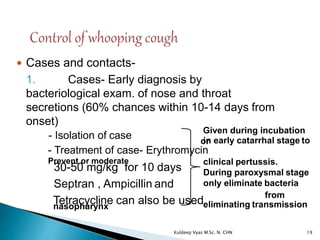
Pertussis, or whooping cough, is a highly contagious respiratory disease caused by Bordetella pertussis, primarily affecting children and characterized by severe coughing spells. In India, cases significantly declined after the introduction of an immunization program, although recent trends show increased incidence in older demographics. The disease spreads through person-to-person contact, often leading to severe complications, especially in infants under six months.