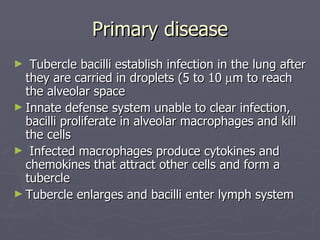
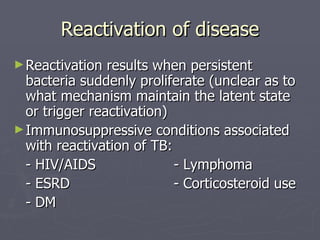
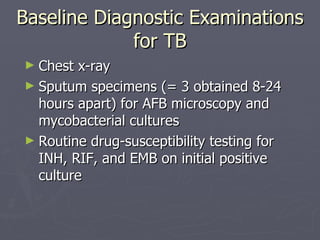
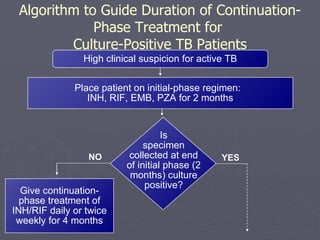
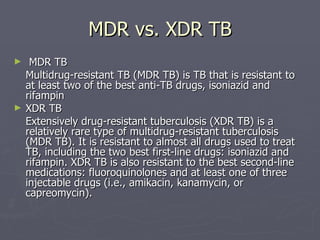
This document summarizes information about pulmonary tuberculosis, including its epidemiology, pathogenesis, signs and symptoms, complications, treatment recommendations, and drug-resistant strains. It notes that tuberculosis is one of the leading infectious causes of death worldwide. HIV infection is a major risk factor for reactivating latent tuberculosis. Treatment involves a combination of drugs over several months, with extensions for cavitary or drug-resistant cases. Multidrug-resistant tuberculosis is resistant to at least two key anti-tuberculosis drugs, while extensively drug-resistant tuberculosis is resistant to nearly all treatment options.