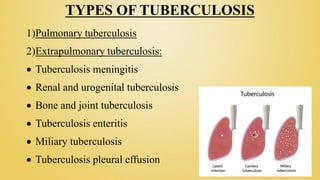
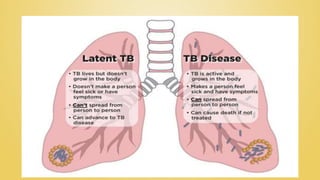
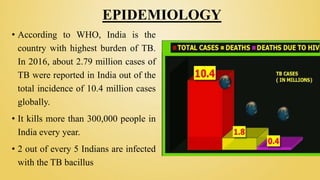
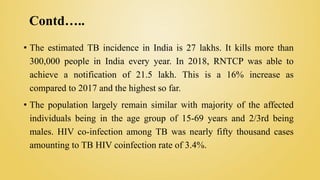
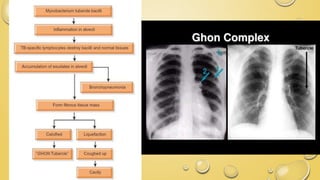
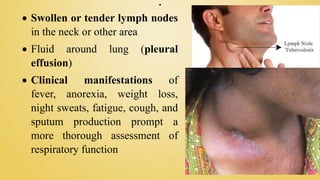
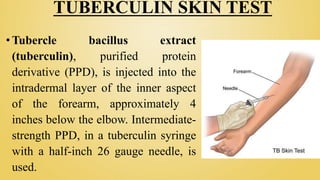
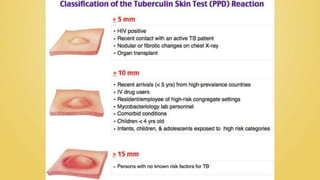
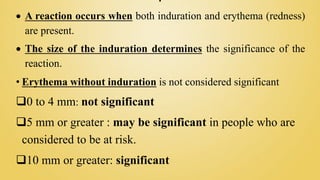
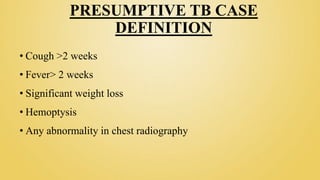
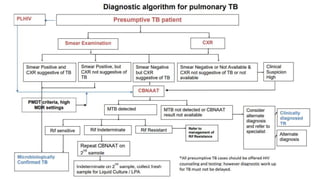
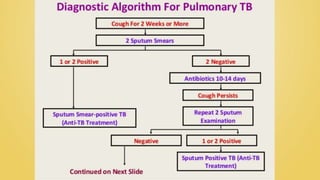
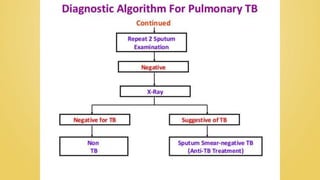
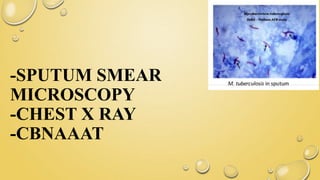
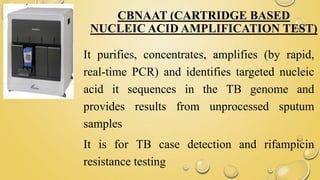
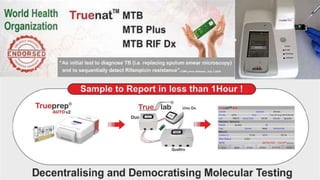
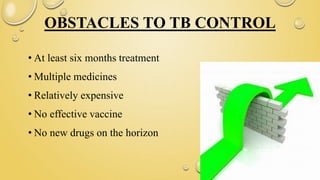
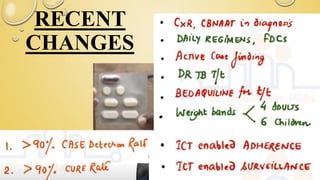
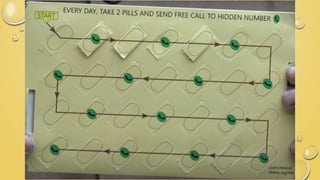
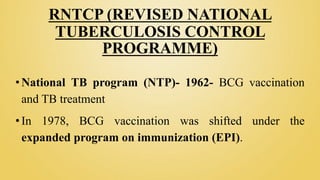
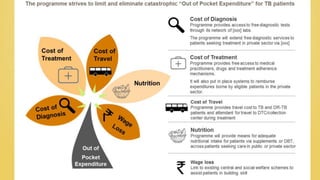
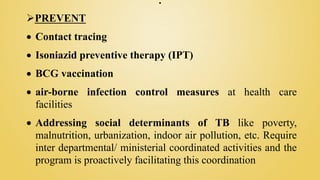
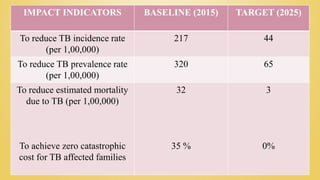
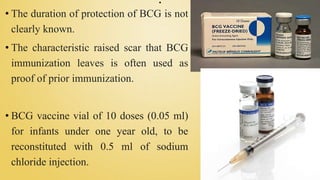
The document provides a comprehensive overview of pulmonary tuberculosis, including its epidemiology, diagnostic methods, treatment options, and prevention strategies. India has the highest burden of TB globally, with significant morbidity and mortality rates, necessitating effective public health interventions and treatment adherence. Key elements include the Revised National Tuberculosis Control Programme (RNTCP), which emphasizes detection, treatment, prevention, and building health systems to combat TB.