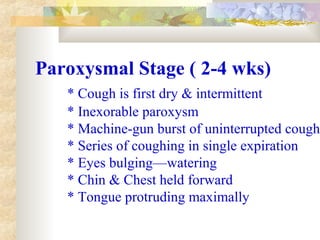
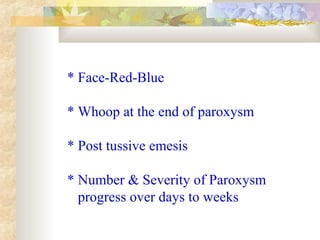
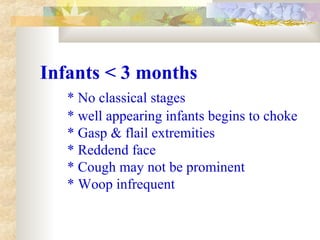
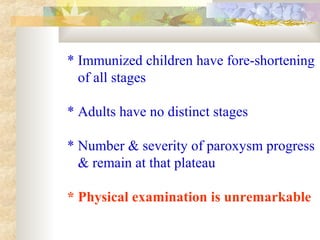
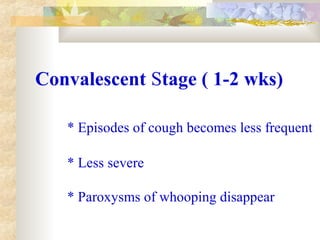
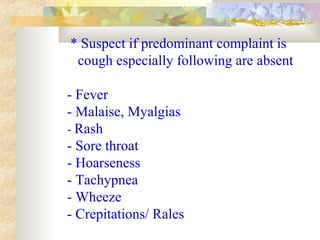
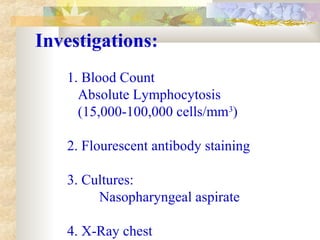
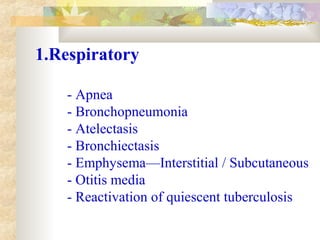
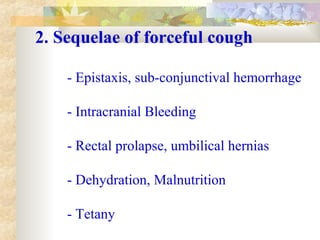
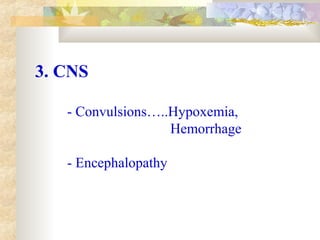
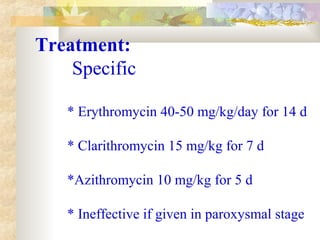
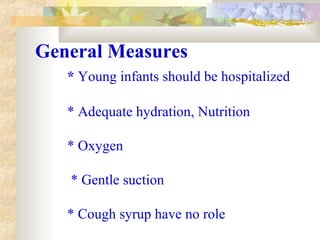
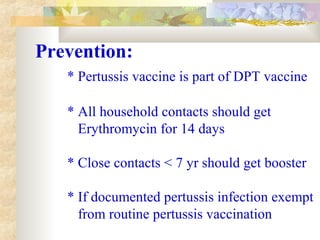
This document discusses pertussis (whooping cough), including its etiology, epidemiology, pathophysiology, clinical features, diagnosis, complications, treatment, and prevention. Pertussis is caused by the bacterium Bordetella pertussis and is highly contagious, especially in children ages 1-5 years old. It presents in stages including catarrhal, paroxysmal, and convalescent stages. Diagnosis is usually clinical based on paroxysmal coughing fits. Complications can include respiratory issues, seizures, and intracranial bleeding. Treatment involves erythromycin or similar antibiotics and supportive care. Prevention is through vaccination and prophylactic antibiotics for close contacts when