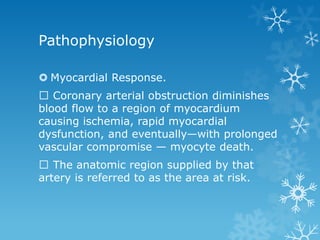
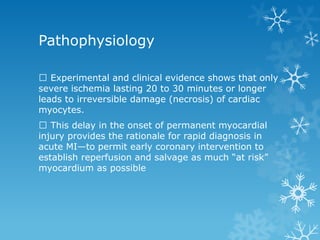
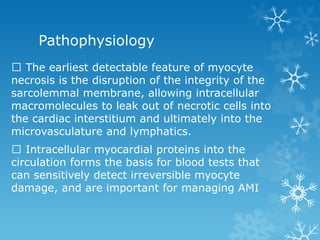
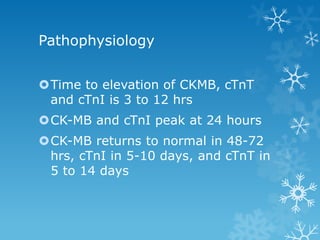
Acute myocardial infarction, or heart attack, results from prolonged ischemia due to a blockage in a coronary artery that supplies blood to heart muscle. Risk factors include increasing age, male sex, hypertension, dyslipidemia, diabetes, smoking, obesity, physical inactivity, excessive alcohol intake, and family history. Diagnosis involves electrocardiogram changes, elevated cardiac biomarkers, and symptoms like chest pain. Management focuses on oxygen, pain relief, antiplatelet/anticoagulant drugs, revascularization, and lifestyle changes to prevent future heart attacks.