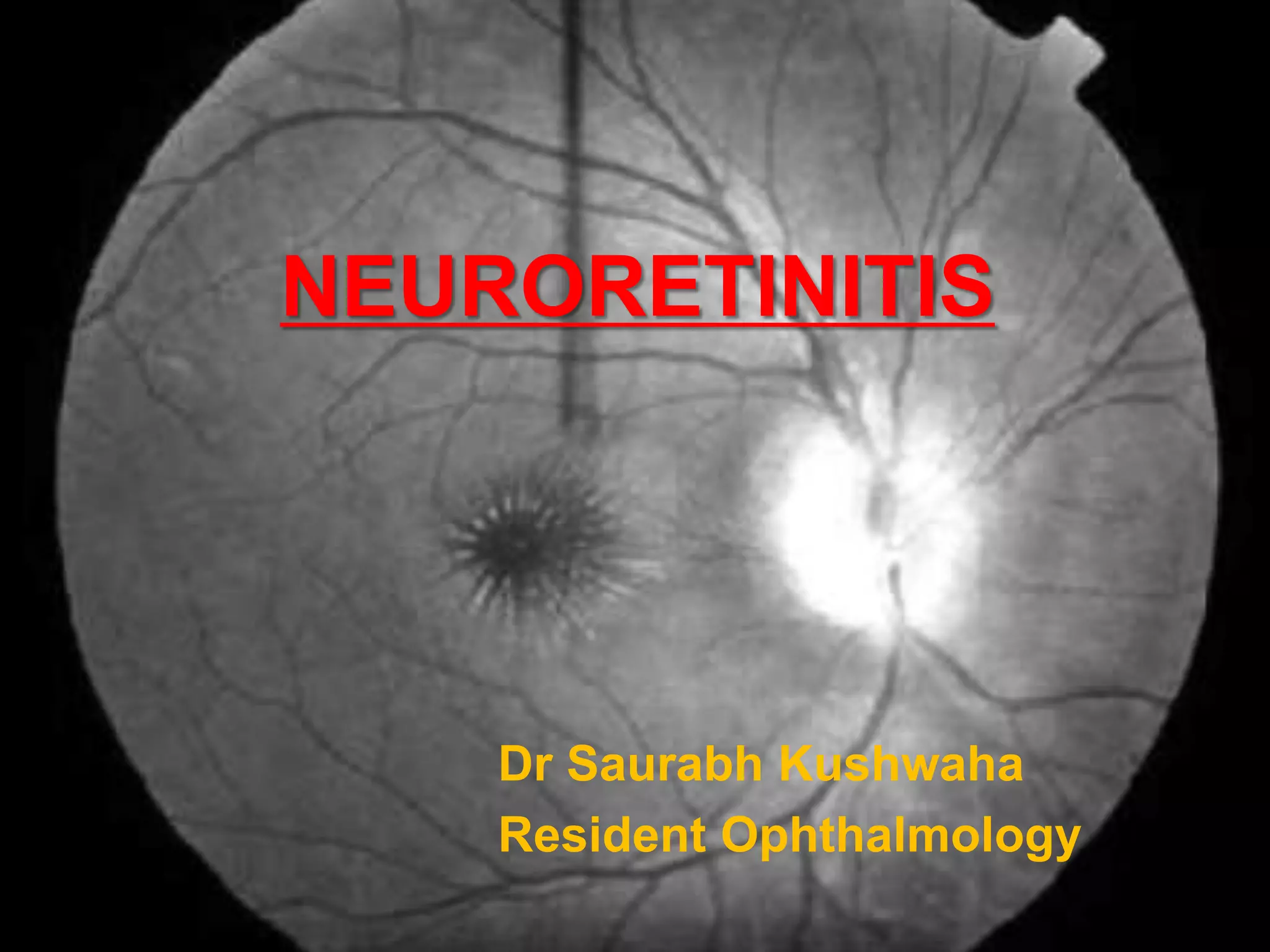
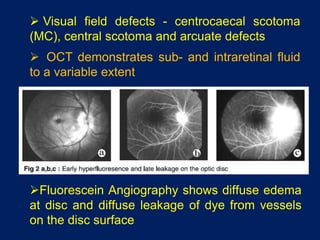
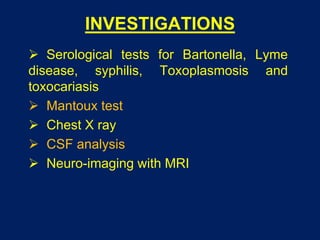
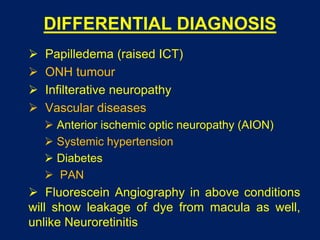
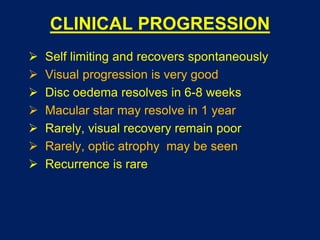
Neuroretinitis is characterized by optic disc edema and a macular star pattern. It is often idiopathic but can be associated with viral infections. Common symptoms include sudden vision loss without pain. Evaluation involves serological testing and imaging to investigate for infectious etiologies. While it typically resolves spontaneously on its own, specific antibiotic treatment may aid recovery if an infection is identified. The prognosis is generally good with resolution of disc edema within 6-8 weeks and macular star within a year, resulting in restored vision.